Annemieke Videler, PhD, Elianne Eijffinger, MSc, OT, Frans Nollet, MD and Anita Beelen, PhD
From the Department of Rehabilitation, Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands
Annemieke Videler, PhD, Elianne Eijffinger, MSc, OT, Frans Nollet, MD and Anita Beelen, PhD
From the Department of Rehabilitation, Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands
OBJECTIVE: To assess initial efficacy and tolerability of a thumb opposition splint on manual dexterity, perceived upper limb functioning and occupational performance in patients with Charcot-Marie-Tooth disease.
DESIGN: One group pre-post design.
Patients and methods: Thirteen patients were provided with a neoprene opposition splint for their dominant hand. Manual dexterity (Sollerman hand function test), perceived upper limb functioning (Michigan Hand Outcomes Questionnaire) and occupational performance (Canadian Occupational Performance Measure) were assessed after using the splint and compared with pre-treatment scores (paired t-tests). Usability and tolerability were assessed with a questionnaire.
RESULTS: Sollerman test scores improved significantly from a mean of 47 (standard deviation (SD) 11) to 52 (SD 12) points (norm 80 points) (p = 0.006). Perceived functioning in the domain activities of daily living (scale 0–100) improved significantly from 51 (SD 20) to 60 (SD 17) points (p = 0.04). Both occupational performance and satisfaction scores improved significantly (p = 0.020). Efficacy did not relate to age, disease duration or severity. Subjects were satisfied with splint cosmesis and comfort.
CONCLUSION: These results indicate that a thumb opposition splint can be applied effectively to improve upper limb functioning in patients with Charcot-Marie-Tooth disease.
Key words: Charcot-Marie-Tooth disease; rehabilitation; hand; thumb; splints.
J Rehabil Med 2011; 00: 00–00
Correspondence address: Annemieke J. Videler, Department of Rehabilitation, A01, Academic Medical Center, University of Amsterdam, PO Box 22660, NL-1100 DD Amsterdam, The Netherlands. E-mail: annemieke@videler.nl
Submitted June 4, 2011; accepted November 9, 2011
INTRODUCTION
There is increasing interest in upper limb involvement in patients with Charcot-Marie-Tooth disease (CMT) (1–7). CMT, also known as hereditary motor and sensory neuropathy (HMSN) is the most common inherited neuropathy, affecting approximately one in every 2,500 individuals (8). It is characterized by slowly progressive, length-dependent bilateral distal muscle weakness, atrophy and sensory loss (9, 10). Hand weakness and dysfunction may be present from the earliest stages of the disease (11) and may be associated with limitations in daily activities (7). In a previous cross-sectional study among 49 adults with CMT type 1A, we found that impaired manual dexterity and perceived limitations in upper limb related activities are common findings, especially with activities that require fine motor function, such as writing, buttoning, using zips, and picking up money (6). It has been shown recently that tripod pinch strength and the ability to oppose the thumb are the most important determinants of impaired manual dexterity in CMT, explaining 67% of the total variance in manual dexterity scores (12). These earlier results provided the evidence-based foundation for therapeutic intervention strategies to improve manual dexterity and preserve or enhance daily life functioning of patients with CMT. We hypothesized that improving the ability to oppose the thumb with a splint may improve manual dexterity, and thus upper limb functioning. There is no literature available on any kind of splint therapy in patients with CMT. Based on promising clinical experiences with CMT patients we developed a short thumb opposition splint. The aim of this prospective intervention study was to assess the initial efficacy of this splint on manual dexterity, perceived upper limb functioning and occupational performance in patients with CMT, and to assess the usability and tolerability of the splint.
METHODS
Participants
Thirteen patients with CMT, known at the Department of Rehabilitation or Neurology of the Academic Medical Centre (AMC) in Amsterdam, participated in this pre- and post-intervention study. Inclusion criteria were: (i) diagnosis of CMT confirmed by DNA or electrophysiological study; (ii) age between 18 and 75 years; (iii) limited thumb opposition (Kapandji score < 6, inability to oppose the thumb to the 5th finger (13); and (iv) perceived impairments of hand function. Subjects were excluded if any other disabling disorders in their medical history might influence hand function of the dominant hand or if they had difficulty understanding the Dutch language. The medical ethics committee of the hospital approved the study and all subjects gave written informed consent.
Intervention
The intervention consisted of a short thumb opposition splint for the dominant hand. This splint positions the thumb more opposite to the fingers, enabling the patient to form a better pinch grip between the thumb and the fingers (Figs 1 and 2). The splint was custom made for each patient and fabricated from 2.4-mm thick neoprene material. On the radial side of the thumb, additional support with thermoplastic material was applied (Fig. 2). Patients were instructed to wear the splint as much as possible during the day for the intended duration of 5 weeks and for a minimum of 1 week.

Fig. 1. The neoprene thumb opposition splint positions the thumb more opposite the fingers.

Fig. 2. A thermoplastic piece on the radial side of the splint provides additional opposition support, enabling a better pinch grip.
Measurement instruments
Maximal isometric grip and pinch strength was assessed to indicate disease severity, using digital handgrip dynamometers (Lode Medical Technology, Groningen, The Netherlands) according to a recommended and standardized testing procedure (14). Patients were seated on a height-adjustable chair and received verbal encouragement during the strength measurements. For grip strength testing, the handle of the dynamometer was set in the recommended second position (15). The mean force (in Newtons) of 3 trials was taken for all strength measurements. The use of hand-held dynamometry to measure hand strength has been shown to be highly reliable and valid in adults with CMT (5).
Manual dexterity of the dominant hand was assessed with the Sollerman hand function test (SHT). The SHT test assesses unilateral and bilateral handgrip function and reflects the most common handgrips used in daily life. It provides information on both the functional ability and the quality of movement of the hand and also includes a time factor. It consists of 20 subtests, each comprising a task considered to be an activity of daily living. Each subtest is scored by the examiner on a scale from 4 to 0 points according to guidelines for scoring. A sum-score was calculated. The scoring rules were chosen so that subjects with normal manual dexterity would achieve 80 points with the dominant hand. The SHT has been applied previously in CMT with excellent test-retest reliability (intraclass correlation coefficient 0.99; 95% confidence interval (CI) 0.98–0.99) (2, 5). Differences greater than 3 points can be interpreted as a change in dexterity (5).
Perceived physical functioning of the upper limb was assessed using the Dutch language version of the Michigan Hand Outcomes Questionnaire (MHQ-DLV) (16). The MHQ is a self-administered questionnaire that contains 6 distinct domains: (i) overall hand function; (ii) activities of daily living; (iii) pain; (iv) work performance; (v) aesthetics; and (vi) patient satisfaction with hand function. For each domain a score between 0 and 100 was derived, with higher scores indicating better hand function and less pain. A total MHQ-score can be calculated by determining the mean of the scores of the 6 domains. The MHQ has been shown to be a reliable and valid instrument in patients with various types of hand conditions (17).
Occupational performance was assessed with the Dutch language version of the Canadian Occupational Performance Measure (COPM-DLV) (18). The COPM is designed as an individualized outcome measure to detect change in patients perceived problems in occupational performance over time. Problems in occupational performance are identified in the areas of self-care, productivity and leisure. The COPM is administered with a semi-structured interview. The client identifies the 5 most urgent or important problems in their occupational performance, and rates each of these problems on an ordinal 10-point scale with regard to performance and satisfaction. A total performance score, and a total satisfaction score can be obtained by summing the scores and dividing them by the number of identified problems. A positive difference of 2 or more points between the total pre- and post-intervention scores is considered to be clinically meaningful (18). Test-retest reliability and validity of the COPM have shown to be good, as have criterion- and construct-responsiveness (19–21). The COPM was administered by a trained occupational therapist (EE) with ample experience.
Usability and tolerability of the thumb splint was evaluated with a questionnaire specifically designed for this study. It consisted of questions on the number of hours the splint was used, advantages and disadvantages with daily activities, and visual analogue scale (VAS)-scores for comfort, aesthetics, and ease of putting on and taking off the splint.
Protocol
All patients were invited twice to the Department of Rehabilitation of the AMC. During the first visit dominant grip and pinch strength were measured, manual dexterity (SHT) of the dominant hand was assessed, and the MHQ was completed. Following these assessments the COPM was administered and the splint was custom made by the participating occupational therapist (EE). After a few days of splint wear, the occupational therapist contacted the patient by telephone to check the fitting of the splint. If the splint needed any modifications, an extra visit was planned. The second visit was planned after 5 weeks of splint wear. During this second visit, manual dexterity was re-evaluated with the use of the splint, the MHQ and COPM were administered, and patients rated the splint usability and tolerability. Measurements were performed by the same examiners, in the same location and same order.
Statistical analyses
Patient demographics, grip and pinch strength values, and data on usability and tolerability of the splint were analysed using descriptive statistics. Published reference values of dominant grip strength of healthy subjects, stratified by age and gender, were recalculated into Newtons and compared with CMT patients (14). Initial splint efficacy was assessed by comparing pre- and post-intervention outcomes with paired Student’s t-tests. Associations between initial efficacy of the splint (SHT change scores) and age, disease duration, grip and pinch strengths were explored with Spearman’s rank correlation coefficients. A p-value < 0.05 was considered to be statistically significant. All statistical analyses were performed using the SPSS software package for Windows version 16.0 (SPSS, Chicago, IL, USA).
RESULTS
From the 15 invited patients with CMT, 14 were willing to participate, all of whom had CMT type I. One patient was excluded because of hand surgery. The mean age on examination of the remaining 13 patients (7 male) was 55.6 years (range 40–73 years). Disease duration, expressed as time since the first recall of disease symptoms, varied between 34 and 62 years (mean 47.7 years). Hand involvement varied from 5 to 58.6 years (mean 27 years). All patients were right handed. Grip and pinch strength values are given in Table I.
| Table I. Dominant hand strength (n = 13) | |||
| Median (P25; P75) | Range | % of the norm Mean (SD) [range] | |
| Grip strength (n) | 60 (43; 190) | 8.3–483 | 32.4 (27.7) [3.4–93] |
| 2-point pinch strength (n) | 2 (0; 9.5) | 0–29 | |
| Tripod pinch strength (n) | 0 (0; 13) | 0–24 | |
| Lateral pinch strength (n) | 16 (6.5; 24.5) | 0–61 | |
| 6 patients with Charcot-Marie-Tooth were not able to perform a 2-point pinch, 7 were not able to perform a tripod pinch and 1 patient was not able to perform a lateral pinch, which all resulted in a score of 0 Newton. | |||
Manual dexterity scores improved significantly with the use of the splint, from a mean SHT sum sore of 47 (standard deviation (SD) 11) to 52 (SD 12) points (norm 80 points) (p = 0.006, Table II). The subtests that improved significantly were: turning a screw with a screwdriver (p = 0.007), unscrewing a lid from a jar (p = 0.018), doing up buttons (p = 0.025), and picking up a telephone (p = 0.046). On an individual basis an improvement of at least 3 points (smallest real difference, (5), was found in 7 out of 13 patients (range 6–11 points). The use of the splint hampered manual dexterity (> 3 points) in one patient (SHT –5 points); this patient was elderly, with severely affected hands and a long disease duration. The initial efficacy of the splint did not relate to age, disease duration, grip and pinch strengths (Fig. 3).
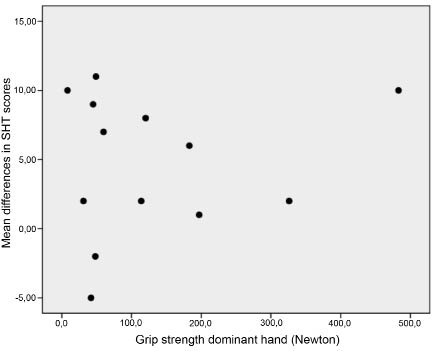
Fig. 3. Relationship between grip strength and differences in manual dexterity (Sollerman hand function test (SHT)) scores.
COPM performance and satisfaction scores improved significantly, but for perceived upper limb functioning, only the improvement in the MHQ domain “activities of daily living” reached significance (Table II).
| Table II. Pre- and post-intervention scores of a thumb opposition splint in patients with Charcot-Marie-Tooth disease | ||||
| Tests | Pre-intervention Mean (SD) | Post-intervention Mean (SD) | Mean Difference Mean (SD) | p-value* |
| SHT | 47 (11.9) | 51.7 (11.4) | 4.7 (5.1) | 0.006* |
| MHQ domain scores | ||||
| Overall hand function | 46.5 (18.2) | 51.9 (17.1) | 5.4 (13.6) | 0.18 |
| Activities of daily living | 51.0 (20.3) | 59.8 (16.7) | 8.7 (8.9) | 0.004* |
| Work | 72.7 (25.6) | 80.8 (23.4) | 8.1 (18.4) | 0.14 |
| Pain | 78.5 (25.2) | 85 (22.5) | 6.5 (15.2) | 0.15 |
| Aesthetics | 69.2 (29.3) | 76.4 (22.4) | 7.2 (29.7) | 0.40 |
| Satisfaction | 42.6 (20.3) | 43.6 (23.6) | 0.96 (17.7) | 0.85 |
| MHQ sum score | 60.0 (18.3) | 66.2 (15.5) | 6.2 (11.4) | 0.08 |
| COPM performance | 4.4 (1.1) | 5.3 (1.5) | 0.9 (1.4) | 0.03* |
| COPM satisfaction | 3.3 (1.7) | 4.9 (1.9) | 1.6 (2.1) | 0.02* |
| *p < 0.05. n = 13; differences between tests were determined with paired-samples t-tests; SHT: Sollerman Hand function Test (norm 80 points); COPM: Canadian Occupational Performance Measure (scale 1–10); MHQ: Michigan Hand Outcomes Questionnaire (scale 0–100, high scores denote better hand performance and less pain); SD: standard deviation. | ||||
All patients used the splint on a daily basis for 1–14 h, with a mean of 6 h/day (SD 4.3). The mean duration of splint wear was 5 weeks (SD 1.6) (range 2–7 weeks). Twelve patients completed the usability and tolerability questionnaire, and indicated that they were moderately satisfied with the splint. On a 10-point VAS a mean score of 5.9 (SD 2.5) (range 2–9) was given for “splint comfort”, a score of 6.3 (SD 2.0) (range 2–9) for “aesthetics” (appearance of the splint) and a score of 6.3 (SD 2.1) (range 3–10) for “ease of use”, such as taking the splint off and putting it on. Patients reported that with the splint on, activities, such as grasping small objects, using eating utensils, doing up buttons, zipping, shaking hands and picking up money were easier to perform. Furthermore some patients reported that after wearing the splint for some time, their thumb remained more in opposition even without the splint on. Disadvantages that were reported included hygiene problems during activities such as self-care, toileting and cooking, and profuse sweating while wearing the splint for a prolonged period of time during hot weather.
The opposition splint also appeared to have a positive impact on other aspects of the hand: with the splint on, clawing of the fingers was less obvious and the hand appeared to be more relaxed.
DISCUSSION
This study showed that the use of a custom-made neoprene thumb opposition splint improves manual dexterity, perceived functioning in daily activities, and occupational performance of patients with affected hand function due to CMT.
More than half of the patients benefited from the splint in performing the SHT. The splint positioned the thumb in more opposition to the fingers, resulting in a better grip and improved thumb stability. This made it easier for patients with CMT to perform test activities that require fine motor skills, such as doing up buttons, as well as activities that require a power grip, such as unscrewing a lid from a jar. Although improvements of > 3 points on the SHT are considered as real changes (i.e. changes that fall outside the measurement error) this does not necessarily imply that these improvements are clinically relevant for individual patients in performing activities of daily living. We have therefore assessed perceived upper limb functioning (with the MHQ) and performance of activities that are meaningful for the patients (COPM). Significant improvements were found on the MHQ in the domain “activities of daily living” (ADL) and on the COPM for both performance and satisfaction scores. Nevertheless, effect sizes were relatively small, and large variability was found, indicating that in some patients the splint had little or no functional benefit. Splint efficacy was not associated with daily wearing time or total duration of splint wear. Unfortunately, our sample size was too small to identify any patient characteristics predictive of splint efficacy.
Although the splint positions the thumb more functionally, it cannot compensate for a weak pinch strength. Previous study showed that in CMT patients thumb opposition explained 10% of the total variance in manual dexterity scores, but loss of tripod pinch strength explained not less then 57% (12). This diminished pinch strength will therefore still hamper many functional activities. Some patients reported, for example, that with the splint they were now able to pick up a key but they still lacked the strength to turn this key in the lock. With a surgical procedure, such as a tendon transfer, an improvement in pinch strength as well may be obtained (22–24). Nevertheless, if surgery is considered, a thumb opposition splint may be provided as a preoperative treatment to mimic effects of a tendon transfer.
With a custom-made splint particular attention should be paid in CMT patients to precise fitting. Pressure points or irritation in the thumb web may easily arise due to the severe atrophy of the intrinsic muscles. Neoprene is one of the softest splinting materials that can be used to fabricate a splint that also provides sufficient support. Nevertheless, there are some disadvantages of this material: it wears out rapidly when used intensively, it can be sweaty during hot weather and although it can get wet it cannot be used during hygienic activities (washing hands, toileting and food preparation). Individual patients have different perceptions and expectations of bracing. Splints may be found to be cumbersome or uncomfortable. Some do not like to use a splint because it draws attention to their impairment. The patients in this study were quite satisfied with splint comfort, the appearance of the splint and with the ease of taking the splint off and putting it on.
With the splint on, some patients experienced difficulties with the altered movement pattern. Older patients, in particular, found it difficult to get used to the splint. This is not surprising after many years of adaptation to, and compensation for, loss of opposition. If people are used to grasping objects with only their fingers instead of using fingers and thumb, it may be more difficult to learn to use their thumb again. If a part of the body has not been used for years, an altered or diminished motor representation of the thumb in the brain may occur (25). Based on these findings it was hypothesized that the efficacy of the splint may differ between more- and less-affected patients. In our study sample age, disease duration and severity of hand involvement appeared not to be a predictive factor for splint efficacy.
An unexpected finding was the positive impact of the splint on the whole hand. With the splint on, clawing of the fingers became less apparent and the hand appeared to be more relaxed. An explanation for this may be that, with the thumb in a more anatomical resting position, the imbalance of intrinsic and extrinsic hand muscles is influenced positively.
This study is the first to evaluate the efficacy of any kind of hand splint for patients with CMT. Nevertheless, it has some weaknesses; firstly, the small sample size. Furthermore, comparing grip strength with healthy reference values showed that the hands of the participating CMT patients were quite severely impaired, and thus they are a highly selected subgroup of CMT patients with affected hand function. Secondly, we assessed initial efficacy and not long-term effectiveness. Due to a restricted study duration some patients used the splint for no longer than one week. This might be too short to adapt to the different thumb position and movement pattern. It would be valuable to study the long-term efficacy and durability of the splint. Future research with a longer intervention duration will give patients more time to adapt to the new thumb position and movement pattern. Together with a larger sample size, sufficient to identify subgroups, this will provide more knowledge about characteristics of patients who benefit from a splint, the long-term effects, durability and suitability of a thumb opposition splint in CMT patients. Furthermore, it would also be valuable to search for a material that is comfortable in all circumstances, that is durable and that can be used while performing hygienic activities. Due to the fact that both hands are affected in CMT, it remains important to pay attention to the design of the splint and to the “ease of use”, such as taking the splint off and putting it on.
In conclusion, a thumb opposition splint should be considered as an effective intervention strategy to improve manual dexterity, perceived upper limb functioning and daily activities of CMT patients with affected hand function.
References
