OBJECTIVE: To validate the dimensionality, hierarchical properties, and reliability of the Frenchay Activities Index.
DESIGN: Self-report survey of patients with stroke.
Patients: A total of 127 patients provided 254 observations before and after treatments.
METHODS: Multidimensional Rasch model was conducted.
RESULTS: The 2-factor model showed the significantly smallest deviance and fitted the data best among 6 possible models. The 2-factor structure was stable before and after treatments, after the rating scale was revised from 4 points to 3 points. Differential item functioning relevant to the time since stroke was detected for 2 tasks. The item difficulty hierarchy of the 2 domains was determined. The correlation between the 2 domains was 0.58. The scale demonstrated acceptable ceiling and floor effects. The overall person (separation) reliability was 0.99. The reliabilities for the 2 domains were 0.81 and 0.73.
CONCLUSION: The Frenchay Activities Index is a useful 2-dimensional scale for evaluating daily functions in stroke patients. The item difficulty hierarchy and significant differential item functioning related to the time since stroke might reflect the changes in the recovery course after stroke. The Frenchay Activities Index could be improved by adding items to capture patients with high and low levels of daily activities in domestic chores.
Key words: activities of daily living; stroke; rehabilitation; reliability and validity.
J Rehabil Med 2012; 00: 00–00
Guarantor address: Ching-Yi Wu, Department of Occupational Therapy and Graduate Institute of Behavioral Sciences, Chang Gung University, 259 Wen-Hwa 1st Road, Kwei-Shan Tao-Yuan, Taiwan. E-mail: cywu@mail.cgu.edu.tw
Submitted April 11, 2011; accepted September 22, 2011
Introduction
Stroke is a main cause of disability and death worldwide (1). Although stroke mortality is decreasing, stroke survivors often experience residual difficulties in participating in activities of daily living (ADL) and suffer from significant losses in body function and structure, resulting in reduction in participation in social activities (2). Therefore, assessing the limitations of a patient’s ability to participate in ADL relevant to his or her life role is of particular importance in stroke rehabilitation (2).
The primary outcome measures to assess the level of independence in ADL include basic and instrumental ADL (IADL) scales (3, 4). Basic ADL scales focus on simple, self-care activities, such as feeding and toileting (5), and these have been criticized for the lack of higher levels of physical activities and significant ceiling effects as recovery progress (4, 6) as well as for the lack of information to reflect ADL (7). To address the limitations of basic ADLs, IADL scales, such as the Frenchay Activities Index (FAI) (7) and the Nottingham Extended ADL Scale (8), were developed to capture patients’ abilities to perform complex activities. IADL scales usually involve hobbies, shopping, housekeeping, and social interactions and require higher levels of body functions in the home and community. IADL performance might affect the quality of life in stroke patients and has received much attention in rehabilitation research (9).
The FAI is a widely used measure of IADL (3, 10). The FAI, corresponding to the participation domain in the World Health Organization (WHO) International Classification of Functioning, Disability, and Health (ICF) (11, 12), was originally designed to reflect everyday activities of pre-morbid living (7). The FAI usually takes a few minutes to complete and is very easy to administer (13). Researchers have used classical test theory to exclusively study convergent validity, reliability, and responsiveness in stroke patients and in elderly individuals. The FAI showed significant correlations with the Barthel Index, the Sickness Impact Profile, and the Stroke Impact Scale-ADL/IADL (9), as well as with the modified Nottingham Extended ADL Scale (8), supporting the convergent validity. The internal consistency (range 0.70–0.90) and the inter-rater agreement (range 0.26–0.94) supported adequate reliability (9, 14–16). Wu et al. (8) reported that the standardized response mean of the FAI equals 0.50, approaching moderate responsiveness. The FAI is a relatively sound measure of IADL; however, further research to validate the FAI is needed to identify the dimensionality and underlying components of this instrument.
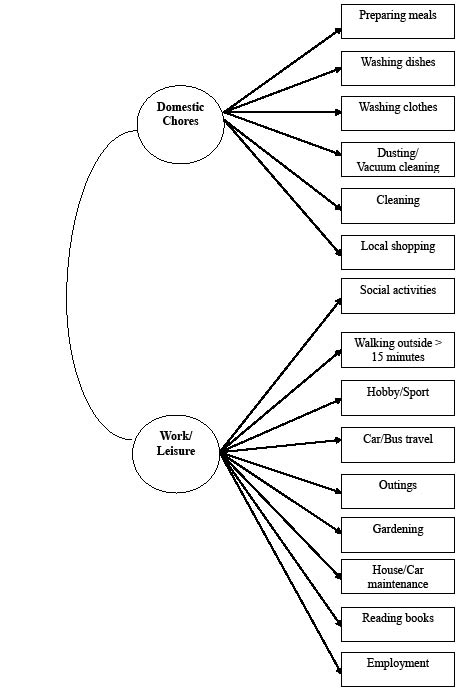
Previous studies reported inconsistent results of the construct validity of the FAI. Most research indicated that the FAI is multidimensional, ranging from 2 to 4 dimensions. Holbrook & Skilbeck (7), who used exploratory factor analysis (EFA), suggested that the FAI consisted of 3 factors: domestic chores (e.g. preparing meals, washing dishes, washing clothes, vacuum cleaning, and cleaning), leisure/work (e.g. social activities, hobby/sport, outings, and employment), and outdoor activities. Some researchers reported 2-factor solutions, including domestic chores and work/leisure domains (9, 17) derived from EFA or confirmatory factor analysis. Han et al. (13) reported a 4-factor solution (domestic chores, outdoor work, leisure, and hobby) for the Korean version of the FAI. Of note, some items of the FAI cross-loaded to more than 1 factor in the 2- and the 3-factor solutions. These discrepant findings imply that the FAI has a complex structure, where domains might overlap or be intercorrelated, and more research on the construct validity of the FAI is needed.
Although most research has reported the multidimensionality of the FAI, two studies assumed that the FAI was unidimensional and performed Rasch analysis to examine the item characteristics of the FAI in patients with stroke and in those with spinal cord injury (12, 18). These two studies suggested removing items to meet the assumption of unidimensionality, but ignored the need for assessing a patient’s comprehensive functional status in diverse skills (19). Since the FAI might measure more than one important underlying ability (7), the test structure of the FAI warrants further scrutiny using specific study samples.
The multidimensional Rasch model offers advantages of exploring the dimensionality of the FAI test structure (20–22). This model not only can transform ordinal scores into interval data and determine if the response categories of a scale can differentiate participants by their responses, but also can specify the structure and the relationship between persons and items within multiple underlying traits of a scale. The analysis of the multidimensional Rasch model is essentially confirmatory in nature, where items are pre-assigned to dimensions based on theoretically grounded hypotheses or empirical evidence in previous studies. In addition, the multidimensional Rasch model can identify easy items, which are easy enough for subjects with low IADL functions, and difficult items, which are challenging enough for patients with good IADL functions.
Unlike the unidimensional Rasch model, the multidimensional Rasch model may prevent distortion and improve precision of estimates by taking into account correlations among factors within a measure (23), as well as empirically exploring the potentials in forming subscales of an instrument (24). The multidimensional Rasch model yields more accurate estimates about the extent an individual item rates and what items can be grouped to form a subscale.
A general form of the multidimensional Rasch model is the multidimensional random coefficient multinomial logit model (MRCMLM) (25). This method can deal with between-item and within-item multidimensionality. A test that consists of several unidimensional subscales is regarded as between-item, whereas a test containing items related to more than one latent dimension is considered within-item. Given the complex nature of the FAI test structure, which might imply between-item or within-item multidimensionality, this study used multidimensional Rasch analysis (i.e. MRCMLM) to examine the test structure and item characteristics of the FAI.
The purpose of this study was to investigate the dimensionality of the FAI and its item difficulty in patients with stroke. The 1-, 2-, 3-, and 4-factor models were examined to determine which model fit the data best.
MethodS
Participants
All participants in the present study were recruited from 4 rehabilitation departments in Taiwan and enrolled in our clinical investigations of stroke motor rehabilitation between 2006 and 2008 (e.g. distributed constraint-induced therapy, bilateral arm training, and conventional rehabilitation). The inclusion criteria included: (i) first-ever stroke; (ii) ability to understand the study and respond to questions; (iii) demonstration of Brunnstrom stage II or higher for the proximal and distal parts of the affected upper limb (26); and (iv) a Mini-Mental State Examination score of 22 or higher. Excluded were patients with physician-determined major medical problems, such as severe aphasia, a vision problem, or poor physical condition. Ethical approval for this study was obtained from the Human Ethics Committees of all the study sites. All patients provided written informed consent.
Procedures
Eligible participants were randomly assigned into 1 of the 3 treatment groups for 90 min over a period of 3 weeks: distributed constraint-induced therapy, bilateral arm training, or control treatment. Six certificated occupational therapists with training in the administration of the intervention protocols provided treatments in the present study. Five independent evaluators masked to the participant group administered the assessments before and after treatment at the participating cites.
Outcome measure
The FAI was used to assess pre-morbid lifestyle and changes in activities after stroke. The items are on a 4-point scale and ask engagement in 10 daily activities during the past 3 months and in 5 activities performed during the last 6 months.
Data analysis
ConQuest version 2.0 (Australian Council for Educaitonal Research, Camberwell, Australia) (27), using the MRCMLM to analyse responses (25), was used in the present study. Six models were examined, including a 1-factor (12, 18), 2 distinct 2-factor (9, 17), 2 3-factor models (28), and a 4-factor model (13). χ2 difference tests were used to determine which model fit the data best: χ2difference=|d1–d2|/dfdifference, here d is deviance. If the χ2 difference test is significant, the model with a smaller value of deviance is considered better than the other.
Once the best model was determined, local response dependency was examined by inspecting the inter-item residual correlation matrix in individual factors. A single correlation above 0.30 indicated minimal local dependence (29). When high residual correlations were detected, these items were combined into “testlets” (30).
Rating scale diagnostics was examined using a rating scale model. The criteria were as follows (31): at least 10 responses per rating category; the average participation in a task of each rating category increases as the rating value increases; outfit mean squares (MNSQ) of each rating category less than 2, and each category in an item with approximately equal frequencies. If a rating category failed to meet these criteria, collapsing the rating category would be considered.
After the rating scale diagnostics step, item fit was checked through the unweighted (outfit) and the weighted (infit) MNSQs as well as the weighted t and the unweighted t. Values of MNSQs beyond the range of 0.6 and 1.4 and the absolute t values greater than 2 indicate misfit items (32). The order of item difficulty and response biases related to time (before and after treatment), and onset (< 12 months and ≥ 12 months) were deemed present if t-tests were significant using a Bonferroni-corrected significance level at 0.003.
The item-person map was used to understand the relation between item difficulty and person ability, termed as targeting. This was examined by the mean participant ability of the individual domain in relation to the overall difficulty in that domain and by floor and ceiling effects. A floor effect was a participant who scored 0 in every task, whereas a ceiling effect represented an individual who reported 3 in all activities. Floor or ceiling effects exceeding 20% of the sample size are considered significant (33). Lastly, test reliability was assessed via person (separation) reliability of the whole test and the Cronbach’s alpha of the individual domains.
Results
We approached 790 individuals for eligibility, and 576 of them did not meet the inclusion criteria. Eighty-seven patients refused to participate in this study. A total of 127 community-dwelling stroke patients, providing 254 observations before and after treatment, were included in the present study. Table I enlists patients’ clinical and demographic characteristics.
| Table I. Demographic and clinical characteristics of patients |
| Characteristics | Value |
| Gender, n (%) | |
| Male | 93 (73.23) |
| Female | 34 (26.77) |
| Age, years, mean (SD) | 55.27 (11.73) |
| Time since stroke, months, mean (SD) | 16.82 (16.05) |
| Side of stroke, n (%) | |
| Right | 60 (47.24) |
| Left | 67 (52.76) |
| Stroke type, n (%) | |
| Haemorrhage | 46 (36.22) |
| Infarction | 50 (39.37) |
| Ischaemia | 27 (21.26) |
| Unknown | 4 (3.15) |
| Onset, n (%) | |
| < 12 months | 68 (53.54) |
| ≥ 12 months | 59 (46.46) |
| Brunnstrom stage, median (interquartile range) | |
| Proximal upper limb | 4 (4–5) |
| Distal upper limb | 4 (4–5) |
| Mini-Mental State Examination, mean (SD) | 27.76 (2.02) |
| Functional Independence Measure, mean (SD) | 115.8 (13.32) |
| Education, years, mean (SD) | 10.24 (4.10) |
| SD: standard deviation. |
Factor structure of the Frenchay Activities Index
The 6 models were examined in this study. Table II provides information of fit indices, reliability, and misfit items. The 2-factor model (17) (Fig. 1) showed the smallest value of deviance and significance in χ2 difference tests, indicating that this model fit the data best among those models. The two domains were domestic chores and work/leisure. Only this model was examined in the following analyses.
| Table II. Fit indices of 6 models |
| Variables | Models |
| 1-factor (18) | 2-factor (17) | 2-factor (9) | 3-factor (7) | 3-factor (28) | 4-factor (13) |
| Deviances | 7293.90 | 7049.59 | 7329.81 | 7069.94 | 7186.08 | 7052.66 |
| Parameters | 18 | 20 | 20 | 23 | 23 | 27 |
| Degrees of freedom | 236 | 234 | 234 | 231 | 231 | 227 |
| Person (separation) reliability for the whole test | 0.99 | 0.99 | 0.99 | 0.99 | 0.99 | 0.99 |
| Reliability for individual domains (Cronbach’s alpha) | 0.88 | 0.81 0.76 | 0.78 0.71 | 0.82 0.78 0.69 | 0.83 0.68 0.74 | 0.87 0.67 0.86 0.64 |
| Misfit items | Hobby/sport Reading books | None | Social activities Hobby/sport | Washing clothes Household/car maintenance | Hobby/sport Household/car maintenance | None |
Fig. 1. Two-factor activities of daily living (ADL) model (17).
Local response dependency and rating scale diagnostics
None of pairs of items revealed residual correlations above 0.30, and the assumption of local independence was held. Disordered thresholds were observed, indicating the 4-point scale could not effectively differentiate patients and showed the redundancy of 4 rating categories. From the disordering of the step difficulties and response frequency on each category of the items, we decided that the category 0 was retained, categories 1 and 2 were collapsed as 1, and the rating 3 was re-coded into 2. Reanalysis showed that the new 3-point scale (Table III) met all essential criteria and functioned properly.
| Table III. Response category of the revised Frenchay Activities Index |
| | Response category |
| Never | Occasionally or more | Most days |
| Preparing meals | 0 | 1 | 2 |
| Washing dishes/up | 0 | 1 | 2 |
| | Never | Occasionally or more | At least weekly |
| Washing clothes | 0 | 1 | 2 |
| Dusting/vacuum cleaning (light housework) | 0 | 1 | 2 |
| Cleaning (heavy housework) | 0 | 1 | 2 |
| Local shopping | 0 | 1 | 2 |
| Social activities | 0 | 1 | 2 |
| Walking outside > 15 minutes | 0 | 1 | 2 |
| Hobby/sport | 0 | 1 | 2 |
| Car/bus travel | 0 | 1 | 2 |
| Outings | 0 | 1 | 2 |
| | Never | Light to moderate | All |
| Gardening | 0 | 1 | 2 |
| Household/car maintenance | 0 | 1 | 2 |
| | None | At least once in the last 6 months | Over a fortnight |
| Reading books | 0 | 1 | 2 |
| | None | ≤ 30 h/ week | > 30 h/week |
| Employment | 0 | 1 | 2 |
Item fit and differential item functioning of the revised Frenchay Activities Index
No evidence of misfitting items was detected (Table IV). Responses were invariant across time, supporting the decision to combine the data collected before and after treatment. Significant differential item functioning, however, was detected relevant to onset. Compared with patients with stroke onset of less than 12 months, patients with onset of 12 months or greater reported higher frequencies in hobby/sport and car/bus travel.
| Table IV. Item statistics of the revised Frenchay Activities Index |
| Item | Item difficulty measure | Item difficulty (SE) | Infit | Outfit |
| MNSQ | t Statistics | MNSQ | t Statistics |
| The domain of domestic chores |
| Preparing meals | 0.56 | 0.08 | 0.91 | –1.00 | 0.99 | –0.10 |
| Washing dishes | 0.28 | 0.08 | 0.72 | –3.50 | 0.87 | –1.40 |
| Washing clothes | 0.27 | 0.08 | 0.63 | –4.90 | 0.87 | –1.40 |
| Dusting/vacuum cleaning (light housework) | –0.55 | 0.07 | 0.97 | –0.30 | 0.91 | –1.00 |
| Cleaning (heavy housework) | 0.45 | 0.08 | 1.00 | 0.00 | 0.89 | –1.10 |
| Local shopping | –1.01 | 0.17 | 1.33 | 3.40 | 1.16 | 1.80 |
| The domain of work/leisure |
| Social activities | –0.55 | 0.07 | 0.87 | –1.50 | 0.85 | –2.20 |
| Walking outside > 15 min | –2.09 | 0.08 | 0.94 | –0.60 | 1.02 | 0.20 |
| Hobby/sport | –0.10 | 0.07 | 1.19 | 2.10 | 1.24 | 3.20 |
| Car/bus travel | –0.60 | 0.07 | 1.00 | 0.00 | 1.04 | 0.60 |
| Outings | 0.21 | 0.08 | 0.77 | –2.80 | 0.76 | –3.20 |
| Gardening | 1.06 | 0.09 | 1.12 | 1.40 | 1.25 | 1.80 |
| Household/car maintenance | 1.37 | 0.10 | 0.87 | –1.50 | 0.90 | –0.60 |
| Reading books | 0.44 | 0.08 | 1.49 | 4.90 | 1.20 | 2.10 |
| Employment | 1.14 | 0.23 | 1.15 | 1.70 | 1.37 | 2.40 |
| SE: standard error; MNSQ: mean squares. |
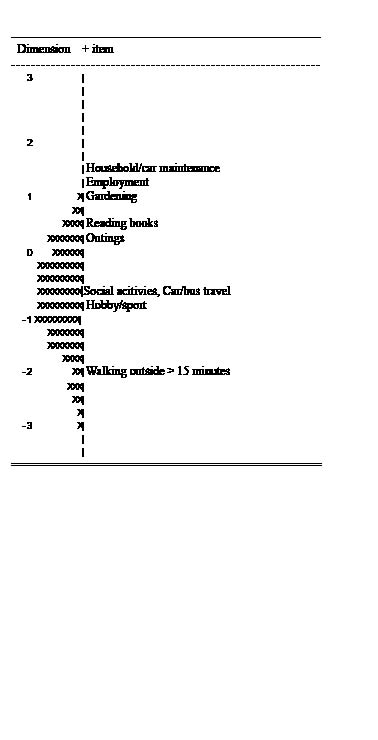
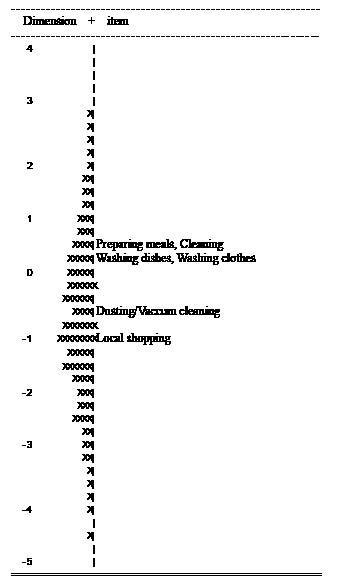
Targeting and item-difficulty hierarchy of the revised Frenchay Activities Index
The item-person map of dimensions 1 and 2 are presented in Figs 2 and 3. Item information is available in Table IV. The mean person-ability estimates were –0.76 (standard deviation (SD) 0.11) for dimension 1 and –0.77 (SD 0.05) for dimension 2. These values suggested that the test items were generally difficult for patients with stroke: 16.5% of participants scored 0, and 7.5% of them reported 3 in all tasks of the domain of domestic chores; 5.5% of participants scored 0, and 0.4% reported 3 in every task of work/leisure. No significant ceiling effects or significant floor effects were found.
Fig. 3. In the person-item map of work/leisure, the column of numbers to the left is logit. The symbol “X” to the left of the centre-line represents 2.6 participants. The most able people and the most difficult items are at the top, and vice versa.
The item difficulty order in the domain of domestic chores, from the most to the least difficulty, was preparing meals, cleaning, washing dishes, washing clothes, dusting/vacuum cleaning, and local shopping. For the domain of work/leisure, the most difficult item was household/car maintenance, followed by employment, gardening, reading books, outings, social activities, car/bus travel, hobby/sport, and walking outside for 15 min or longer.
Fig. 2. In the person-item map of domestic chores, the column of numbers to the left is logit. The symbol “X” to the left of the centre-line represents 2.6 participants. The most able people and the most difficult items are at the top, and vice versa.
Test reliability of the revised Frenchay Activities Index
The correlation coefficient between 2 domains of the FAI was 0.58. The overall separation reliability was 0.99, indicating that the FAI items separated participants into 4.24 statistically distinct ability levels (strata) (34) on the basis of their IADL performance. The Cronbach’s alpha of the domains of domestic chores and of work/leisure were 0.81 and 0.73. These values achieved an acceptable level of reliability (33).
Discussion
This study is the first to use the multidimensional Rasch model to validate the number of dimensions and the item difficulty hierarchy within each dimension of the FAI in patients with stroke. The 15-item FAI reflected 2 domains, domestic chores and work/leisure, without tasks cross-loaded into more than one domain, suggesting that the FAI can be divided into two subscales. We determined the initial 4-point scale should be revised to reflect frequencies of IADL performance in patients with stroke. Six items loaded on the domain of domestic chores, where local shopping was the least difficult and preparing meals was the most difficult task for stroke patients. The domain of work/leisure consisted of the rest of 9 FAI items, where walking outside for more than 15 minutes was the easiest and household/car maintenance was the most difficult task. The 2-factor solution was stable at pre- and post-treatment, but was influenced by the time after stroke (onset). Evidence from the present study supported that the targeting of the revised FAI is appropriate for patients with stroke. The subscales and the overall FAI were reliable, and the FAI can distinguish 4.24 distinct levels of IADL performance.
The property of dimensionality is fundamental to the construct validity of a measure and is particularly important when a total score is used for comparisons in rehabilitation interventions (35). This study found that the test structure of the FAI was represented by two factors, domestic chores and work/leisure, and supported the finding of Han et al. (17) in Japanese community-dwelling older residents. Compared with earlier factor analytic studies on the FAI in stroke patients (7, 13, 28), the present study, using the multidimensional Rasch model, does not require normally distributed data and provides unbiased estimates of the number of dimensions in the FAI. Moreover, this study examined which model reported in previous studies fit real data better. Because the multidimensional Rasch model performs better than the unidimensional Rasch model when the test structure is not theoretically unidimensional and enables researchers to test various measurement models of the factors underlying an assessment, the use of the multidimensional Rasch model would provide strong evidence regarding the construct validity of the FAI. We therefore concluded that the FAI may be divided into two subscales, and none of the items were overlapped in more than one subscale.
The original 4-point scale was not appropriate to reflect the performance of each ADL in patients with stroke. Data showed unequal frequencies of rating categories and disordered person measures. These findings, consistent with previous studies (12, 18), indicate that the ratings 1 and 2 were infrequent responses among the 4 rating categories. Therefore, the present study collapsed rating category 2 with the rating category 1. The revised 3-point scale functioned properly, without the disordering person measures, and differentiated participants by their IADL performance. In addition, the 3-point scale meets the need of simplicity for clinical administration and is thus recommended for use.
The test structure of the FAI was quite stable at pre- and post-treatments. This finding supports that a response to a FAI task indeed reflects a participant’s performance in extended ADL and is a useful measurement to assess change after rehabilitative intervention. In addition, this study found significant differential item functioning for two tasks related to time since stroke. Chronic patients (onset ≥ 12 months) reported more involvement in hobby/sport and car/bus travel compared with non-chronic patients (onset < 12 months). Fatigue, medical complications, social fears, and attitudinal barriers might limit abilities in mobility and engagement in ADL after stroke. However, stroke survivors living in the community for more than 1 year after stroke participated in a wider variety of community activities more frequently after intensive rehabilitation (36). Chronic patients might spend more time on leisure activities or work compared with patients with onset of less than 12 months.
All items of the FAI showed adequate item fit in the study. The item difficulty hierarchy suggested that tasks requiring higher levels of motor ability and cognitive capacity were rated more difficult compared with simple tasks. For example, compared with reading books, employment requires higher mobility and cognitive ability to commute between home and office, complete assigned work, effectively communicate with co-workers and supervisor, and comply with the norms of the work setting. Thus, employment was rated as more difficult than reading books in the present study. Items of the domestic chores domain were clustered between the range of the logit of 0 and 1, indicating these tasks were more capable of differentiating patients with moderate levels of IADL and would not be able to capture patients with high and low levels of IADL performance in domestic chores. The comprehensiveness of this domain might be improved by adding easier tasks, such as “telephoning” and “procuring and taking medicine as ordered”, and more difficult tasks, such as care of pets (37). The findings that the items of the domain of work/leisure spread out along the continuum of IADL performance suggest that the subscale provides a comprehensive understanding of work/leisure in stroke patients.
The FAI showed appropriate targeting for participants with stroke in terms of the closeness between the average person ability and the mean item difficulty, and acceptable reliability of the whole test and of two domains. The scale demonstrated acceptable ceiling and floor effects. Findings of the person reliability suggested that the FAI could divide stroke patients into at least 4 groups by the level of IADL performance.
Given the findings from previous construct validations and the present study, it is clear that the FAI assesses a multidimensional construct of IADL and all tasks contribute to the IADL construct. However, several factors (e.g. gender, age, educational level, living conditions, impairment in cognitive ability and mobility, and culture) may influence the performance in the FAI (38) and warrant consideration when interpreting the scores as well as the dimensionality of the FAI. Participants in the present study had stroke with mild to moderate upper extremity (UE) impairment, and they were capable of understanding and responding questionnaires. Thus, taking the findings of Han et al. (17) into account, it was suggested that the two subscale scores and a composite of the two subscale scores be used to indicate individual performance in IADL for the specific group of stroke patients or for non-stroke community-dwelling elderly people in Japan. Future studies may recruit other groups of stroke patients to validate our findings or pool data from international studies using the DIF analysis to examine whether the 2-factor model is stable across cultures. Then, researchers may provide a better rule for appropriate use of the FAI total score and subscale scores.
Caution should be exercised when generalizing the results of the present research beyond the scope of the study. Although Rasch model produces sample-free item parameters (39), data for the present study were drawn from participants with mild to moderate UE impairment in Taiwan, who were capable of understanding and responding to the FAI. Thus, the results of this study may not be generalized to stroke patients with severe UE dysfunction, stroke patients with cognitive impairment, or to patients from different cultures. Further validations of the FAI in stroke patients with various levels of severity in the motor or cognition deficits and from diverse cultures are warranted.
In conclusion, we showed that the FAI is a multidimensional scale that can be easily administered and is appropriately targeted for IADL performance in stroke patients. The FAI could be divided into two subscales to better represent IADL performance. The original 4-point scale may be revised into the 3-point scale. Chronic and non-chronic patients responded differently in two tasks of the FAI, possibly because of their differences in physical functions and social adjustment. From these findings, we conclude that the FAI is a useful instrument for determining extended daily life functions of stroke survivors during recovery or treatment course.
Acknowledgements
This work was supported in part by the National Health Research Institutes (NHRI-EX100-9920PI and NHRI-EX100-10010PI), the National Science Council (NSC 97-2314-B-002-008-MY3 and NSC 99-2314-B-182-014-MY3), and the Healthy Aging Research Center at Chang Gung University (EMRPD1A0891).
References