Rationale: The gap in knowledge translation from research to clinical practice is under scrutiny in stroke rehabilitation. One possible reason for this gap may be a poor understanding of clinicians’ practice style traits and how they influence practice behaviours.
OBJECTIVES: To identify the prevalence of practice style traits in physical therapists and occupational therapists working in stroke rehabilitation and, to explore associations between these traits and practice behaviours, where practice behaviours are defined as the clinicians’ reasons for choosing assessments and interventions used in practice. The influence of more traditional personal and organizational factors on practice behaviours was also explored.
DESIGN: Cross-sectional survey of a representative random sample of 243 clinicians (117 occupational therapists and 126 physical therapists) working across the continuum of stroke care in Ontario, Canada.
METHODS: A telephone-administered validated clinical practice survey elicited information in 4 areas: practice style traits using the validated Practice Style Questionnaire, therapists’ reasons for choosing assessments and interventions (practice behaviours), personal factors and organizational factors.
RESULTS: For both disciplines, the most prevalent trait was pragmatist and the least prevalent was seeker. Seekers were the most likely to use evidence-based reasons for choosing assessments, but this finding did not reach significance (χ2 = 5.430, df = 3; p = 0.14). The most typical reason for choosing an intervention was that the clinician had learned it during professional training, an interesting finding given that approximately half of clinicians had more than 10 years of experience. Of the 21 potential explanatory variables examined, few explained clinicians’ reasons for choosing assessments or interventions.
CONCLUSION: While understanding practice traits is not going to be the single solution to closing the knowledge translation gap, it may help to guide best practice implementation strategies.
Key words: stroke, practice styles, evidence-based practice, knowledge translation, assessment, interventions.
J Rehabil Med 2007; 39: 685–692
Correspondence address: Nicol Korner-Bitensky, School of Physical and Occupational Therapy, McGill University, 3630 Promenades Sir-William-Osler, Montreal, Quebec, H3G 1Y5, Canada. E-mail: nicol.korner-bitensky@mcgill.ca
Submitted January 11, 2007; accepted May 7, 2007.
INTRODUCTION
There is growing pressure on rehabilitation professionals to stay current with best practices (1, 2). New assessment tools and intervention strategies are introduced in rapid succession with the expectation that they will be incorporated into everyday practice. This is especially true for stroke, one of the most prevalent conditions treated by rehabilitation professionals and one with an extensive body of scientific literature (3).
Regrettably, there is widespread recognition that gaps exist in knowledge exchange between researchers and clinicians (4). In an effort to close these gaps, numerous studies have focused on investigating the effectiveness of various education and knowledge translation (KT) strategies (5). In a comprehensive paper, Grimshaw et al. (5) examined 41 systematic reviews and found that, while some KT strategies such as the use of an opinion leader hold promise, no intervention is highly effective for inducing practice change.
Researchers have typically focused on understanding the traditional personal and organizational factors that influence successful KT (6). For example, Jette et al. (7) surveyed 488 physical therapists (PTs) and found that age, professional training, as well as familiarity and confidence in search strategies, database use and critical appraisal skills, were associated with self-perceived use of evidence-based practice (EBP). Specifically, younger clinicians were more confident in their search and critical appraisal skills, as were those with higher academic degrees. Dickinson et al. (8) led a 3-year longitudinal project exploring the integration of EBP in a mental health organization. Health professionals identified personal factors including poor motivation, lack of confidence, lack of knowledge about EBP, and organizational factors, such as limited access to learning resources, poor teamwork, insufficient time, and staff transfers, as barriers to EBP.
Unfortunately, human traits remain a poorly understood determinant of KT. This recognition has resulted in intensified efforts to identify the intrinsic characteristics of health professionals. For instance, Green et al. (9) suggest that each clinician differs in what they consider to be credible sources of evidence (i.e. the value of evidence vs experience), the weight they assign to practical concerns (i.e. the importance of managing workload vs patient satisfaction), and their willingness to diverge from group norms (i.e. issues of non-conformity). They postulate that all of these underlying factors may together influence how a clinician responds to new evidence and whether this will ultimately change their practice patterns.
Wyszewianski & Green (10) have developed a framework for classifying 4 clinician traits (seeker, receptive, traditionalist and pragmatist) by using a validated Practice Style Questionnaire (see methods section for psychometric properties of the questionnaire). Generally speaking, the seeker guides his or her intervention practices using published data, rather than personal experience or authority. This individual actively reads professional journals, frequently uses electronic resources for learning, and is willing to diverge from traditional practice if evidence-based sources support this change. The receptive is also evidence-oriented and is inclined to change practice, but is more likely to rely on the clinical judgment of respected authorities. His or her practice may differ from local medical culture, given that there is enough evidence to support change. The traditionalist views clinical experience and respected authorities as the most reliable basis for practice. Finally, the pragmatist focuses on practicality and is likely to change practice according to workload demands, patient flow and patient satisfaction, rather than on scientific validity. Wyszewianski & Green (10) point out that these human traits are inherent to how one responds to new information and therefore should be differentiated from states that can change from moment to moment.
Identifying clinicians’ practice styles may have important implications if the argument holds that an understanding of these traits enables customization of KT strategies. Certainly one could imagine that an interdisciplinary team consisting of only individuals who are seekers would function very differently from a team consisting of only pragmatics. It is probable that neither team would function optimally. At their most rudimentary, the seekers might constantly seek change to the point of clinical chaos, whereas a team consisting of only pragmatics might well dig in their heels against change to the point of stagnation. Also, it is highly probably that the KT strategies used to encourage change in these 2 teams would need to be different. Work by Greco & Eisenberg (11) indicates that a combination of both knowledge-oriented strategies, such as seminars and conferences, and behaviour-oriented strategies including incentives for EBP and removing barriers to change, is required to change practice patterns. It is highly plausible that the relative role and importance of each of these strategies will vary according to an individual’s practice style trait.
To date, this intriguing line of inquiry has never been applied in the stroke rehabilitation field. Thus, as a first step, it would be interesting to identify the prevalence of practice style traits amongst stroke rehabilitation professionals, and whether these traits are at all associated with specific practice behaviours. For example, one could postulate that a seeker would be more likely to actively seek new assessments and interventions by independently searching the scientific literature while a pragmatic clinician might be more inclined to make assessment and intervention choices based on resource availability within the worksite, or the practicalities of time. Understanding the general distribution of practice styles among stroke rehabilitation clinicians is a first step towards the next logical inquiry aimed at exploring the effect of matching KT strategies to clinician traits.
There is no literature that has examined practice style traits in stroke rehabilitation professionals and the association of these traits with practice behaviours. Thus, the global objective of this study was to identify the prevalence of practice style traits in PTs and occupational therapists (OTs) working in stroke rehabilitation, and, to explore associations between these traits and practice behaviours, where practice behaviours are defined as the clinicians’ reasons for choosing assessments and interventions used in their daily practice. In addition, we explored the influence of more traditional personal and organizational factors on practice behaviours.
Methods and procedures
Research design
This was a cross-sectional telephone survey of a representative random sample of PTs and OTs working across the continuum of stroke care in Ontario, Canada. Clinicians were interviewed in 2004–2005. Research ethics approval was attained from the Faculty of Medicine, McGill University, Montreal, Quebec.
Sample size considerations
Previous work by our team, on a sample of 100 PTs working in low back pain, suggested that one of the main outcomes of interest – practice style traits – would have a prevalence of pragmatic clinicians of approximately 50% (12). Using a 2-sided confidence interval of 95% and a desired precision of 6%, approximately 267 therapists were required to allow stable estimates (13) of prevalence. This sample size was also sufficient to allow logistic regression analyses to be performed based on 21 potential explanatory variables.
Study population
The goal was to accrue a representative random sample of OTs and PTs working across the continuum of stroke care (acute care, rehabilitation, community-based settings) in Ontario, Canada. Contact lists from the College of Occupational Therapists of Ontario and the College of Physiotherapists of Ontario were used to identify individuals working in adult neurology. Given that practising therapists are required to register with a provincial Order, these lists provide a valid sampling frame.
Clinicians were eligible if they: were registered with the provincial Order; had provided stroke rehabilitation for ≥ 3 months during the year and treated ≥ 2 adult patients with a primary diagnosis of stroke per month; worked in a setting for ≥ 6 months in the past year; spoke English or French; and, provided informed consent.
Clinical practice survey
A validated clinical practice survey (12) was used to elicit information in 4 areas: practice style traits of therapists (Table I) as determined by the Practice Style Questionnaire (10), therapists’ reasons for choosing assessments and interventions (practice behaviours), personal factors, and organizational factors.
Practice Style Questionnaire. Green et al. (9) hypothesized that clinicians’ practice traits are represented by 3 underlying theoretical factors: (i) the value placed on evidence vs experience; (ii) willingness to diverge from group norms in practice (non-conformity); and (iii) the weight they assign to practical concerns of managing workload and patient satisfaction (practicality). Based on these factors, a series of items were generated each rated on a 5-point Likert scale that ranged from strongly agree = 5, to strongly disagree = 1. Once the items were refined for clarity with a group of practitioners, 3 iterations of the questionnaire were created and tested on 1287 physicians (106, 1120 and 61, respectively). To refine the questionnaire at each iteration, and to examine how the items correlated with each other, factor analysis was performed using principal-components analysis. The hypothesized 3-factor model was found to have the best fit, producing the same 3 underlying factors that were originally theorized (9). The internal consistencies (as measured by Cronbach’s alpha) for the 3 factors ranged from 0.68 to 0.79. The final iteration of the questionnaire includes 17 items with scores for the items within each factor summed to generate 3 sub-total scores of 30, 30 and 25; the total possible score is 85. A classification scheme using cut-off sub-total scores for the 3 factors is used to categorize clinicians into the 4 practice traits, seeker, receptive, traditionalist and pragmatist, and a fifth category, other, which indicates that a clinician is not trait classifiable (Table I). Some examples of items for each factor are: “Clinical experience is more important than randomized controlled trials” (evidence vs experience factor), “I am comfor practicing in ways different than other doctors” (non-conformity factor) and “I follow practice guidelines if they are not too much hassle” (practicality factor). Trait classification is based on cut-off scores for each factor. For example, a sub-total score ≥ 22 out of 30 for the evidence vs experience factor indicates the individual relies heavily on evidence, and is classified as a seeker. A sub-total score > 14 out of 25 for the practicality factor indicates that the individual is quite concerned with maintaining their workload and patient satisfaction, thus they are classified as a pragmatist (9).
| Table I. Prevalence of practice style traits among occupational therapists (OTs) and physical therapists (PTs) (n = 243) |
| Practice style trait | OTs (n = 117) | PTs (n = 126) |
| n (%) | 95% CI | n (%) | 95% CI |
| Seeker (n = 16) | 2 (1.71) | –0.64–4.04 | 14 (11.11) | 5.54–16.46 |
| Receptive (n = 37) | 20 (17.09) | 10.19–23.81 | 17 (13.49) | 7.53–19.45 |
| Traditionalist (n = 26) | 13 (11.11) | 5.33–16.67 | 13 (10.32) | 4.01–15.63 |
| Pragmatist (n = 134) | 66 (56.41) | 47.01–64.99 | 68 (53.97) | 45.30–62.70 |
| Others* (n = 30) | 16 (13.66) | 7.71–20.29 | 14 (11.11) | 5.54–16.46 |
| *Clinicians who were unclassifiable as per the Practice Style Questionnaire (10). CI: confidence interval. |
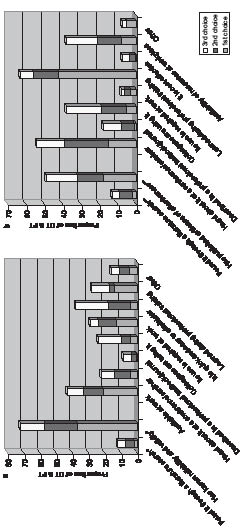
Reasons for choosing assessments and interventions. The closed-ended lists of therapists’ reasons for choosing assessments and interventions (described in Figs 1a and b) were compiled based on an extensive literature review of EBP behaviours and consultation with researchers working in the area of EBP and clinicians working in stroke rehabilitation.
Fig 1. Clinicians´ top three reasons for choosing an assessment (a) and an intervention (b). Defined as an evidence-based *assessment chooser, **intervention chooser. OT: occupational therapists; PT: physical therapists.
Personal and organizational factors. Personal and organizational factors that potentially affect KT were also identified from the scientific literature and included in the clinical practice survey (described in Tables II and III). Experts in KT, rehabilitation research and educational methodology reviewed these lists for completeness and clarity. The clinical practice survey was pilot-tested on a convenience sample of 5 clinicians to ensure ease of flow and clarity of questions (12).
Data collection
As the validity of this study depended on high response rates, a specific interview guideline was used to achieve maximal participation: the Total Design Method (14). This guideline has been shown to achieve high recruitment rates, ranging from 87% to 95%, for various respondents including patients, families and clinicians. It details the optimal format for asking questions, the process for choosing the mode of administration, and the optimal timing of contact with the respondent. This method also describes the rigorous training procedures to be used in terms of styles of interaction, introductory statements and the development of a personalized contact.
Well-trained interviewers traced potential participants and once contacted, the clinician was screened for eligibility. Those who agreed to participate were scheduled for a 25-min telephone interview to respond to the validated clinical practice survey (12). The list of potential reasons for choosing assessments and interventions were forwarded to therapists 24–48 h before the interview, so that it could be referred to during the interview. To reduce contamination, participants were asked to refrain from discussing the survey with colleagues and attempts were made to perform all interviews within a site in relatively close succession.
Data management and analyses
After each clinician interview, the interviewer checked the completeness of the survey and the data were entered into a computerized database and verified against the original survey. Analyses were performed using SPSS 14.0 Inc. 2006.
Descriptive statistics were used to calculate the prevalence of practice style traits according to discipline. Next, we calculated the prevalence of clinicians’ reasons for their stroke-related assessment and intervention choices, again by discipline. Then, reasons for stroke-related assessment choices (as described in Fig. 1a) were dichotomized to produce a variable “evidence-based assessment chooser” (yes/no) defined as a clinician who based his or her choice of assessment tools on either: “it has known reliability and validity” or “found it during a literature search”. Likewise, clinicians’ reasons for their intervention choices (as described in Fig. 1b) were dichotomized such that an “evidence-based intervention chooser” was defined as a therapist who based his/her choice of interventions on either: “it has evidence of effectiveness” or “found it during a literature search”. These classifications were based on consultation with researchers in KT regarding those reasons which would reflect an EBP manner of deciding on assessment and intervention use.
To explore the association between potential explanatory variables (practice styles, personal factors and organizational factors) and a clinician described as being an evidence-based assessment chooser or evidence-based intervention chooser, univariate analyses (t-tests and cross-tabulations) were performed (Tables II and III). As numerous comparisons were performed (i.e. 19 categorical and 2 continuous explanatory variables), the threshold for significance was set at 0.01.
Two multivariate analyses using logistic regression were also conducted to investigate the contribution of potential explanatory variables that were associated with being an “evidence-based assessment chooser” (yes/no) or an “evidence-based intervention chooser” (yes/no). Modelling was attempted using stepwise backward elimination on all 21 explanatory variables, or forward modelling, where necessary.
RESULTS
This study is part of a larger cross-Canada survey completed in 2004–05 on a random sample of clinicians from all 10 provinces. A sample of 1072 OTs were contacted, of which 290 were ineligible, 71 were untraceable and 48 (6.8%) refused, with the remaining 663 OT participating. For PTs, 1024 were contacted, 171 were ineligible, 99 were untraceable and 98 (12.9%) refused, resulting in 656 participants. Here we present the findings from the sub-study of practice style traits conducted on 117 OTs and 126 PTs that were randomly sampled from Ontario. The sample, largely women, had a mean age of 38 years and 41 years for OTs and PTs, respectively. Forty-seven percent of these clinicians had more than 10 years of experience with a stroke clientele.
Information on practice style prevalence by discipline (OT and PT) is presented in Table I. All but 30 clinicians (12.3%) were classifiable into one of the 4 traits. For both disciplines, the most prevalent practice style was pragmatist and the least prevalent was seeker. The distribution of practice traits by discipline was similar, with the exception of a slightly higher prevalence of seekers in PTs.
The top 3 reasons for choosing stroke-related assessments and interventions are shown in Figs 1a and 1b, for OTs and PTs combined. The most prevalent reason for choosing an assessment was “it has known reliability and validity”. The most prevalent reason for choosing a treatment intervention was “I learned it during my professional training”. While this study did not set out to compare disciplines, the data suggest that there were important differences. OTs were more likely than PTs (32% vs 10%) to choose assessment tools that were available at work, and less likely (34% vs 50%) to rely on interventions that they learned during their professional training.
Table II presents the association between the potential explanatory variables (practice traits, personal factors, and organizational factors) and being an evidence-based assessment chooser (74%, n = 179). Seekers were the most likely to be evidence-based assessment choosers at 87.5%, vs 78.4% of receptives, 57.7% of traditionalists, and 73.9% of pragmatists (X2 = 5.430, df = 3; p = 0.14). One variable, funds for continuing education, was significantly associated (p = 0.01) with being an evidence-based assessment chooser: Clinicians working at sites that provided funds for continuing education were more likely to rely on scientific evidence when choosing assessment tools (89%) compared with those working at sites that did not provide funds (77%) (Table II). Other factors such as younger age, having a specialty certification, presence of student placements, and working in a site that is supportive of ongoing learning approached significance (p-values ranging from 0.02 to 0.04). Multivariate analyses found that 3 variables – working in a site supportive of ongoing learning, having specialty certification, and work environment (acute, rehabilitation or community), explained only 8.4% of the variability in the outcome evidence-based assessment chooser.
| Table II. Potential explanatory variables associated with being an evidence-based assessment chooser (EBAC) (n = 243) |
| Personal factors | EBAC = Yes (n = 179) | EBAC = No (n = 64) | ANOVA (F) | p-value |
| Age (years); mean (SD) | 38.99 (± 8.70) | 41.73 (± 10.14) | 4.222 | 0.04 |
| Time spent on continuing education (h/month); mean (SD) | 7.05 (± 6.70) | 6.21 (± 7.48) | 0.686 | 0.41 |
| | n (%) | n (%) | χ2 | p-value |
| Gender Female (n = 226) | 167 (93.30) | 59 (92.19) | 0.089 | 0.77 |
| Discipline Occupational therapy (n = 117) Physical therapy (n = 126) | 85 (47.49) 94 (52.51) | 32 (50.00) 32 (50.00) | 0.119 | 0.73 |
| Degree Diploma (n = 28) Bachelors (n = 202) Masters (n = 13) | 16 (8.94) 152 (84.92) 11 (6.15) | 12 (18.75) 50 (78.13) 2 (3.13) | 5.004 | 0.08 |
| Experience with stroke clientele (n = 3 missing) < 1 year (n = 6) 1–3 years (n = 41) 4–10 years (n = 80) > 10 years (n = 113) | 5 (2.84) 35 (19.89) 56 (31.82) 80 (45.45) | 1 (1.56) 6 (9.38) 24 (37.50) 33 (51.56) | 4.169 | 0.24 |
| Work schedule Full-time (n = 174) | 130 (72.63) | 44 (68.75) | 0.348 | 0.56 |
| Specialty certification (n = 1 missing) Yes (n = 118) | 95 (53.37) | 23 (35.94) | 5.726 | 0.02 |
| Teaching at university Yes (n = 38) | 32 (17.88) | 6 (9.38) | 2.583 | 0.11 |
| Practice style trait (n = 30 other) Seeker (n = 16) Receptive (n = 37) Traditionalist (n = 26) Pragmatist (n = 134) | 14 (8.92) 29 (18.47) 15 (9.55) 99 (63.06) | 2 (3.57) 8 (14.29) 11 (19.64) 35 (62.50) | 5.430 | 0.14 |
| Organizational factors | | | | |
| Work environment (n = 1 missing) Acute care (n = 60) Rehabilitation (n = 73) Community (n = 109) | 44 (24.72) 59 (33.15) 75 (42.14) | 16 (25.00) 14 (21.88) 34 (53.13) | 3.246 | 0.20 |
| Location of site (n = 1 missing) Urban (n = 167) Suburban (n = 40) Rural (n = 35) | 126 (70.39) 25 (13.97) 28 (15.64) | 41 (65.08) 15 (23.81) 7 (11.11) | 3.584 | 0.17 |
| Academic affiliation (n = 1 missing) Teaching (n = 136) | 107 (59.78) | 29 (46.03) | 3.576 | 0.06 |
| Presence of stroke unit/team (n = 2 missing) Yes (n = 84) | 68 (37.99) | 16 (25.81) | 3.010 | 0.08 |
| Number of stroke admissions per month (n = 4 missing) 0–10 (n = 149) 11–20 (n = 62) 21–30 (n = 13) 31–40 (n = 6) > 40 (n = 9) | 112 (63.64) 44 (25.00) 11 (6.25) 2 (1.14) 7 (3.98) | 37 (58.73) 18 (28.57) 2 (3.18) 4 (6.35) 2 (3.18) | 6.315 | 0.18 |
| Student placements (n = 1 missing) Yes (n = 220) | 167 (93.30) | 53 (84.13) | 4.740 | 0.03 |
| Research conducted at site (n = 1 missing) Yes (n = 96) No (n = 132) Don’t know (n = 14) | 73 (40.78) 97 (54.19) 9 (5.03) | 23 (36.51) 35 (55.56) 5 (7.94) | 0.912 | 0.63 |
| Site supportive of ongoing learning Yes (n = 232) | 174 (97.21) | 58 (90.63) | 4.725 | 0.03 |
| Access to new information on site Yes (n = 218) | 161 (89.94) | 57 (89.06) | 0.040 | 0.84 |
| Time allocated for learning on site (n = 1 missing) Yes (n = 106) | 76 (42.70) | 30 (46.88) | 0.334 | 0.56 |
| Funds for continuing education Yes (n = 209) | 160 (89.39) | 49 (76.56) | 6.442 | 0.01 |
| SD: standard deviation; ANOVA: analysis of variance. |
Table III indicates that none of the potential explanatory variables (practice traits, personal factors and organizational factors) were significantly associated with being an evidence-based intervention chooser (56%, n = 135). However some variables, such as teaching at the university level, being in an urban setting, presence of a stroke unit/team, presence of student placements, and working in a site supportive of ongoing learning, approached significance (p-values ranging from 0.03 to 0.05). Multivariate analyses found only one variable that remained in the model – presence of a stroke unit/team – that explained only 2.1% of the variability in clinicians choosing or not choosing evidence-based interventions.
| Table III. Potential explanatory variables associated with being an evidence-based intervention chooser (EBIC) (n = 243) |
| Personal factors | EBIC = Yes (n = 135) | EBIC = No (n = 108) | ANOVA (F) | p-value |
| Age, years (mean (SD)) | 37.29 (± 8.93) | 40.22 (± 9.43) | 51.854 | 0.432 |
| Time spent on continuing education (h/month); mean (SD) | 7.14 (± 6.77) | 6.43 (± 7.09) | 30.976 | 0.422 |
| | n (%) | n (%) | χ2 | p-value |
| Gender Female (n = 226) | 123 (91.11) | 103 (95.40) | 1.673 | 0.20 |
| Discipline Occupational therapy (n = 117) Physical therapy (n = 126) | 69 (51.11) 66 (48.89) | 48 (44.44) 60 (55.56) | 1.068 | 0.30 |
| Degree Diploma (n = 28) Bachelors (n = 202) Masters (n = 13) | 15 (11.11) 112 (82.96) 8 (5.93) | 13 (12.04) 90 (83.33) 5 (4.63) | 0.234 | 0.89 |
| Experience with stroke clientele (n = 3 missing) < 1 year (n = 6) 1–3 years (n = 41) 4–10 years (n = 80) > 10 years (n = 113) | 2 (1.50) 22 (16.54) 45 (33.83) 64 (48.12) | 4 (3.74) 19 (17.76) 35 (32.71) 49 (45.79) | 1.326 | 0.72 |
| Work schedule Full-time (n = 174) | 95 (70.37) | 79 (73.15) | 0.228 | 0.63 |
| Specialty certification (n = 1 missing) Yes (n = 118) | 72 (53.73) | 46 (42.59) | 2.970 | 0.09 |
| Teaching at university Yes (n = 38) | 27 (20.00) | 11 (10.19) | 4.381 | 0.04 |
| Practice style trait (n = 30 other) Seeker (n = 16) Receptive (n = 37) Traditionalist (n = 26) Pragmatist (n = 134) | 10 (8.48) 22 (18.64) 13 (11.02) 73 (61.86) | 6 (6.32) 15 (15.79) 13 (13.68) 61 (64.21) | 0.926 | 0.82 |
| Organizational factors | | | | |
| Work environment (n = 1 missing) Acute care (n = 60) Rehabilitation (n = 73) Community (n = 109) | 33 (24.44) 43 (31.85) 59 (43.70) | 27 (25.23) 30 (28.04) 50 (46.73) | 0.424 | 0.81 |
| Location of site (n = 1 missing) Urban (n = 167) Suburban (n = 40) Rural (n = 35) | 100 (74.07) 15 (11.11) 20 (14.82) | 67 (62.62) 25 (23.36) 15 (14.02) | 6.584 | 0.04 |
| Academic affiliation (n = 1 missing) Teaching (n = 136) | 82 (60.74) | 53 (49.53) | 2.559 | 0.11 |
| Presence of stroke unit/team (n = 2 missing) Yes (n = 84) No (n = 157) | 55 (40.74) 80 (59.26) | 29 (27.36) 77 (72.64) | 4.683 | 0.03 |
| Number of stroke admissions per month (n = 4 missing) 0–10 (n = 149) 11–20 (n = 62) 21–30 (n = 13) 31–40 (n = 6) > 40 (n = 9) | 79 (59.40) 38 (28.57) 7 (5.26) 5 (3.76) 4 (3.01) | 70 (66.04) 24 (22.64) 6 (5.66) 1 (0.94) 5 (4.72) | 3.555 | 0.47 |
| Student placements (n = 1 missing) Yes (n = 220) No (n = 22) | 127 (94.07) 8 (5.93) | 93 (86.92) 14 (13.08) | 3.701 | 0.05 |
| Research conducted at site (n = 1 missing) Yes (n = 96) No (n = 132) Don’t know (n = 14) | 58 (42.96) 69 (51.11) 8 (5.93) | 38 (35.51) 63 (58.88) 6 (5.61) | 1.506 | 0.47 |
| Site supportive of ongoing learning Yes (n = 232) | 132 (97.78) | 100 (92.59) | 3.733 | 0.05 |
| Access to new information on site Yes (n = 218) | 123 (91.11) | 95 (87.96) | 0.644 | 0.42 |
| Time allocated for learning on site (n = 1 missing) Yes (n = 106) | 58 (43.28) | 48 (44.44) | 0.033 | 0.86 |
| Funds for continuing education Yes (n = 209) | 114 (84.44) | 95 (87.96) | 0.617 | 0.43 |
DISCUSSION
Findings from this study indicate that more than half of clinicians surveyed were classified as pragmatists, a trait associated with an approach to changing practice based on workload demands, patient flow, and patient satisfaction, as opposed to scientific validity. This finding is certainly an eye-opener given that those of us working in research or academia are often shocked by the apparent gap between research discoveries and clinical implementation of new assessments and interventions. This study’s findings make it clear that one reason for this gap may be our false assumption that most health professionals are evidence seekers. Indeed the low prevalence of seekers, similar to the 3% reported in physician studies (9,12), suggests that KT strategies geared primarily toward individuals who read professional journals, frequently use electronic resources for learning, and are willing to diverge from traditional practice (15), are likely to be ineffective. Conversely, if the high prevalence of pragmatists seen in this sample is generalizable to the population of OTs and PTs working in stroke rehabilitation, it behoves the research community to focus on developing KT strategies that will be effective for this much larger audience.
While this study does not directly examine the effects of practice style traits on healthcare teams, it does suggest a hypothesis that would be interesting to study in the future. It seems highly probable that almost all healthcare teams consist of individuals with all 4 traits. On first reflection, it may appear that this is rather bad news in an age where EBP requires strong seeker-type behaviours to keep abreast of the rapidly changing literature. However, it is also probable that an interdisciplinary team consisting of members with all 4 traits is likely to be highly efficient if these traits are recognized and respected. For example, an interdisciplinary stroke team may have a maximum of 1 or 2 seekers. A good portion of individuals will likely be receptives, indicating that they are willing to change their behaviours if sound evidence is presented to them. In other words, they will not go out and do the active searching, but are willing to consider evidence and change practice based on it. Now, the high prevalence of pragmatists may at first appear to be a major stumbling block to effecting change. Yet, pragmatists are likely to be the very people who will keep the entire ward running smoothly and who are likely to be dedicated, not necessarily to change, but once the change occurs, to keep things running smoothly once again. Finally, traditionalists who view clinical experience and respected authorities as the most reliable basis for practice decisions are likely to buy into clinical change if the seeker within the team is perceived to be a respected clinician or is able to provide support for the change in practice. Thus, the point may be, not to consider that one trait is somehow superior to another, but to recognize that the richness of a healthcare team is based upon its heterogeneity and is indeed strengthened by the mixture of traits. By understanding the distribution of practice style traits among clinicians, perhaps we can devise a more effective plan of promoting evidence-based practice and continuing education for clinicians. The Ottawa Model of Research Use (OMRU) framework promotes an evidence-based approach to the transfer and use of evidence in clinical settings (16). It emphasizes the importance of tailoring KT strategies to address key barriers and facilitators related to the therapist (i.e. characteristics of potential adopters, which can include their practice styles), in order to achieve successful dissemination. Once the practice style traits of clinicians are assessed, KT strategies could be tailored and executed to meet the individualistic needs of these clinicians.
This study was conducted in Ontario, where a Coordinated Stroke Strategy (17) promoting evidence-based stroke rehabilitation among all health professionals was in place at the time of the study. We thus expected that the actual care provided for individuals who experience a stroke in Ontario would be based on best practice guidelines and would reflect evidence-based approaches for choosing assessments and interventions. Indeed, clinicians reported that the most prevalent reason for choosing an assessment was based on its published evidence for reliability and validity. In contrast, the manner in which interventions were chosen was less likely to be evidence-based, with the majority of clinicians relying on their professional training to guide their treatment plans. This is an interesting finding given that approximately half of the respondents had more than 10 years of experience with stroke, such that it was unlikely that their professional training, unless consistently upgraded, was reflective of EBP. It is also noteworthy that until recently, unlike physicians, OTs and PTs did not have any professional requirements for continuing education credits. Recent policy changes by the licensing bodies in many Canadian provinces now require a clinician to maintain a portfolio that includes information on continuing education courses taken each year.
Interestingly, of the 4 traits, clinicians classified as seekers were the most likely group to be evidence-based assessment choosers. Although this finding fell short of statistical significance, potentially due to sample size limitations, the trend in the hypothesized direction warrants further exploration with a larger sample. Future studies would do well to build sample size calculations based on estimates of the prevalence of seekers in the single digits, which, while necessitating larger sample sizes, will permit more thorough investigation of the practice behaviours of this group.
When it came to other potential explanatory variables associated with being an evidence-based assessment chooser, the study found that clinicians working at sites that provided funds for continuing education were more likely to rely on evidence when choosing assessment tools, such that removing financial barriers to continuing education seemed to be an effective behaviour-oriented strategy for promoting EBP behaviour (11). However, overall, of the long list of potential explanatory variables examined, there was little that explained clinicians’ reasons for choosing assessments or interventions.
Limitations
The Practice Style Questionnaire was at times unpopular with clinicians who found some of the questions quite irksome. Debriefing of the interviewers in an attempt to better understand the problems with the questionnaire revealed that some clinicians perceived the items to be disagreeable and somewhat threatening. When designing this study we were concerned that there would be a potential for social desirability bias with clinicians responding more towards acceptable EBP behaviours. However, the low prevalence of seekers suggests otherwise. In addition, the low prevalence of seekers seen here and elsewhere (9, 12) suggests that, in future studies, a large sample size would be needed to provide stable estimates of all 4 traits.
In conclusion, the challenge for researchers and heathcare professionals is to establish KT strategies that allow efficient and effective use of evidence-based knowledge. A better understanding of practice style traits may be one part of the unsolved puzzle. Empowering clinicians, not only through understanding their own practice style trait, but also through understanding the traits of others, may well be an important first step. As our healthcare system moves towards interdisciplinary healthcare provision, organizations will benefit from reflecting on how their teams are put together. Currently, we would venture that most group formation is done out of necessity or function, without consideration of how the individual parts effectively constitute a whole. While understanding practice traits is clearly not going to be the single solution to closing the KT gap, it may help to build the bridge that is so badly needed for best practice implementation.
Acknowledgements
N. Korner-Bitensky was funded by a senior career award from the Fond de la Recherche en Santé du Québec (FRSQ). A. Menon-Nair was funded by a doctoral award from the CIHR program (Innovations in Patient Safety and Knowledge Translation) at the Faculty of Medicine, University of Toronto, and A. Thomas by a doctoral award from the Fonds Québécois de la Recherche sur la Société et la Culture (FQRSC). This project was funded by the Canadian Stroke Network, the Réseau Provincial de Recherche en Adaptation Réadaptation (REPAR), and the Centre de Recherche Interdisciplinaire en Réadaptation du Montréal Métropolitain (CRIR). We acknowledge the support of Dr J. Lamoureux for statistical analysis, our large and dedicated team of interviewers, and the clinicians who participated. We also acknowledge the investigators who worked on this project for their collaboration: S. Wood-Dauphinee, R. Teasell, J. Hanley, J. Desrosiers, F. Malouin, M. Harrison, F. Kaizer, P. Duncan and E. Kehayia.
Conflict of interest: None declared.
REFERENCES
1. Canadian Physiotherapy Association [cited 2006 November]. Available from: http://www.physiotherapy.ca/public.asp?WCE = C = 11|K = 223245|RefreshS = Container|RefreshT = 223245|A = Body
2. Canadian Association for Occupational Therapists, 2006, [cited 2006 November]. Available from: http://www.caot.ca/default.asp?ChangeID = 163&pageID = 153
3. Heart and Stroke Foundation of Canada. 2002, [cited 2005 July]. Available from: http://ww2.heartandstroke.ca/Page.asp?PageID = 1081&SubCategoryID = 124&Src = stroke&Type = Article
4. Davis D, Evans M, Jadad A, Perrier L, Rath D, Ryan D, et al. The case for knowledge translation: shortening the journey from evidence to effect. BMJ 2003; 327: 33–35.
5. Grimshaw JM, Shirran L, Thomas R, Mowatt G, Fraser C, Bero L, et al. Changing provider behavior: an overview of systematic reviews of interventions. Med Care 2001; 39 Suppl 2: II2-45.
6. Grimshaw JM, Eccles MP, Walker AE, Thomas RE. Changing physicians’ behavior: what works and thoughts on getting more things to work. J Contin Educ Health Prof 2002; 22: 237–243.
7. Jette DU, Bacon K, Batty C, Carlson M, Ferland A, Hemingway RD, et al. Evidence-based practice: beliefs, attitudes, knowledge, and behaviors of physical therapists. Phys Ther 2003; 83: 786–805.
8. Dickinson D, Duffy A, Champion S. The process of implementing evidence-based practice- the curate’s egg. J Psychiatr Ment Health Nurs 2004; 11: 117–119.
9. Green LA, Gorenflo DW, Wyszewianski L. Validating an instrument for selecting interventions to change physician practice patterns: a Michigan Consortium for Family Practice Research study. J Fam Pract 2002; 51: 938–942.
10. Wyszewlanski L, Green LA. Strategies for changing clinicians’ practice patterns: a new perspective. J Fam Pract 2000; 49: 461–464.
11. Greco PJ, Eisenberg JM. Changing physicians’ practices. N Engl J Med 1993; 329: 1271–1273.
12. Mikhail C, Korner-Bitensky N, Rossignol M, Dumas JP. Physical therapists’ use of interventions with high evidence of effectiveness in the management of a hypothetical typical patient with acute low back pain. Phys Ther 2005; 85: 1151–1167.
13. Cochran WG, editor. Sampling techniques. 3rd edn. New York: John Wiley; 1977.
14. Dillman D, editor. Mail and internet surveys: the Tailored Design Method. New York: John Wiley; 2000.
15. Davis D, O’Brien MAT, Freemantle N, Wolf FM, Mazmanian P, Taylor-Vaisey A. Impact of formal continuing education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health outcomes? JAMA 1999; 282: 867–874.
16. Logan J, Graham ID. Toward a comprehensive interdisciplinary model of health care research use. Science Communication 1998; 20: 227–246.
17. Coordinated Stroke Strategy. Heart and Stroke Foundation of Ontario. 1998, [cited 2006 November]. Available from: http://www.lhsc.on.ca/rss/regional.htm