Maria Hondras, DC, MPH, PhD1, Jan Hartvigsen, DC, PhD1,2, Corrie Myburgh, DC, PhD1 and Helle Johannessen, PhD3
From the 1Department of Sports Science and Clinical Biomechanics, Faculty of Health Sciences, University of Southern Denmark, 2Nordic Institute of Chiropractic and Clinical Biomechanics and 3Department of Public Health, Faculty of Health Sciences, University of Southern Denmark, Odense, Denmark
OBJECTIVE: To examine the perspectives of villagers in rural Botswana about the everyday life burden and impact of their musculoskeletal disorders.
METHODS: Ethnographic fieldwork for 8 months included 55 in-depth interviews with 34 villagers. Interviews were typically conducted in Setswana with an interpreter. Audio recordings were transcribed verbatim, with Setswana contextually translated into English. The theoretical lens included Bury’s biographical disruption, in which he distinguishes between “meaning as consequence” and “meaning as significance”.
RESULTS: Interviews revealed co-existing accounts for the consequences and significance of musculoskeletal burden related to 3 themes: (i) hard work for traditional lives; (ii) bearing the load of a rugged landscape; and, (iii) caring for others with disrupted lives. Physical labour with musculoskeletal symptoms had economic and subsistence consequences. The loss of independence and social identity to fulfil traditional roles held meaning as significance. Outmigration for wage labour and other shifts in family structure compounded everyday musculoskeletal burden.
CONCLUSION: Uncovering burden is an important first step to address musculoskeletal care needs in developing country settings. Community-engaged partnerships are needed to develop rehabilitation programmes to ease the burden of musculoskeletal disorders in rural Botswana.
Key words: Botswana; burden of illness; chronic pain; disability; joints; musculoskeletal system; qualitative research; rehabilitation.
J Rehabil Med 2016; 48: 00–00
Correspondence address: Maria Hondras, Department of Sports Science and Clinical Biomechanics, University of Southern Denmark, Campusvej 55, DK-5230 Odense M, Denmark. E-mail: mhondras@health.sdu.dk
Accepted Feb 18, 2016; Epub ahead of print Apr 5, 2016
INTRODUCTION
There is no denying the enormous global burden resulting from more than 1.7 billion people with musculoskeletal (MSK) disorders (1), particularly in low- and middle-income countries (LMICs) (2). Recent initiatives call for LMICs to refocus healthcare strategies to target noncommunicable diseases (3, 4). Notwithstanding the burden of cardiovascular disease, cancer and diabetes, the burden of MSK conditions has important consequences for individuals and society (5), such as the loss of independence, ability to work, and resulting direct and indirect costs of care (6). While global burden of disease estimates are one perspective of public health burden, these estimates do not provide conceptual clarity about burden nor translate into practical strategies for individuals and communities seeking to improve their MSK health and quality of life.
In their systematic review, Froud and colleagues (7) emphasize the importance of adding dimension to measuring what is important to people with chronic non-specific low back pain. Indeed, the everyday burdens experienced by persons with MSK disorders are not well represented in the literature, especially in LMIC settings (2). Shifting the focus for MSK burden to the perspective of individual lives provides a potentially rich source of data to understand what burden feels like, how one lives with burden, and how this burden might be relieved.
In 2009, World Spine Care (WSC) was established as a nongovernmental organization (NGO) to improve lives in underserved communities (8). In 2012, WSC opened its first 2 clinics in the Botswana Central District. WSC programmes aim to develop low-cost models of primary spine care, educate local healthcare workers and patients, and conduct research. Two co-authors (MH, JH) serve on the WSC research team to provide the NGO with empirical work about MSK conditions in local contexts. Our team designed a focused ethnography to examine the meaning of MSK burden in villager lives and propose sustainable rehabilitation programmes alongside the temporal relationship of establishing spine care centres in the country.
Focused ethnography emphasizes an anthropological approach to research while limiting the scope and duration of fieldwork to a specific programme-relevant research problem (9). Similar to the work by Elliot et al. (10) in Sierra Leone for surgically treatable conditions, including MSK conditions, the qualitative data presented here aims to encourage programme development that addresses the burden of MSK conditions in Botswana and other LMICs.
The aim of this focused ethnography is to examine the burden of living with and caring for people living with Muscle, Bone and Joint (MuBoJo) conditions among rural Batswana (the people of Botswana, multiple Tswana persons). In this article we examine villager perspectives of the everyday life burden and impact of their MSK conditions. We draw on Bury’s theoretical perspective of “biographical disruption” (11) and the distinction Bury (12), and others (13, 14) make for “meaning as significance” and “meaning as consequence” to understand the lived experiences and context for MSK burden among rural Batswana.
METHODS
Ethnographic material was generated during 8 months in Botswana. Two visits in late 2011 and early 2013 allowed MH to: establish relationships with government officials and village dikgosi (chiefs); position herself as a NGO researcher as opposed to a member of the clinical care team; and, train local Batswana to assist with the project. Primary data collection ensued from October 2013 to March 2014. The community context and methods for this qualitative study are described elsewhere (15).
Participant recruitment and data collection
Respecting village chiefs’ mode of communication, MH and an interpreter introduced the project at 4 kgotla (traditional village meeting place) gatherings scheduled over several months. This purposive sampling strategy (16) engaged villagers regardless of age, gender, social status or physical condition. The 34 participants (25 women) ranged in age from 20 to 97 years, with a median age of 57 years. Initial in-depth interviews averaged 60 min; follow-up interviews were conducted with 10 participants. In total, 55 interviews resulted in more than 50 h of audio recordings.
MH engaged in non-participant observations and informal interviews in community settings. Participant observations included work routines in villager compounds, at the lands, and at cattle posts to better understand what villagers were doing, thinking and saying (17) in relation to MSK health. These data enhanced interview content and some observations led to in-depth interviews.
MH conducted in-depth interviews in settings convenient for participants, most often in outdoor living areas or open and closed spaces at the kgotlas, clinic facilities and health posts. Interviews were audio-recorded and typically conducted with 1 of 2 study interpreters. MH or an outside professional vendor prepared verbatim transcripts of English spoken during interviews. MH reviewed and corrected vendor-prepared transcripts and inserted placeholders for spoken Setswana before passing documents to Motswana (a single Tswana person) study personnel for verbatim Setswana transcription and contextual English translation. For the latter, 2 of 5 Motswana transcriptionists prepared 91% of transcripts.
Data analysis and interpretation
We used abductive reasoning for data analysis and interpretation (18). Abduction in qualitative analysis is a combination of inductive and deductive thinking with logical underpinnings ((19) citing (20)). More recent applications distinguish abduction from data-based inductive analysis and theory-derived deductive analysis demonstrating the continuous reflexive and dialectic exchange between theories, analytical concepts and empirical findings (21, 22).
Initial stages included close reading of interview transcripts, field-notes and memoranda by the first author to generate substantive concepts that made sense of the data for how respondents described the impact MSK troubles has on their daily lives, broadly clustered into the domains: MSK cause; activities of daily living (ADLs); care for others; home including village home, cattle posts, and at the lands; occupation; and social determinants of health. Secondary, tertiary and subsequent readings used constant comparison (23) to identify similarities and differences in these domains within and across cases, with frequent returns to the raw data to review concepts and reflect on patterns and connections with the data in an inductive manner. Participant biographies conveyed consistent messages related to hard work in a particular environment with or without extended family and social networks.
Subsequent review of the literature incorporated theoretical perspectives in a deductive manner allowing further refinement about how Batswana perceive the burden and impact of MSK troubles. We used Bury’s theory of biographical disruption (11) to examine the meaning of MSK burden in villager lives, in which he asserts that “illness, and especially chronic illness, is precisely that kind of experience where the structures of everyday life and the forms of knowledge which underpin them are disrupted” (11). Bury later (12) delineates the conceptual distinction between meaning as consequence and meaning as significance for chronic illness sufferers. Bury and others (13, 24) use these concepts to examine the impact chronic illness has “on the individual’s sense of self and lived reality” (24). “Meaning as consequence refers to the impact of chronic illness and disability on the individual’s daily life while meaning as significance refers to the social connotations of specific illnesses and functional limitations” ((24) citing (12)).
Data quality
Methodological details to gather data in 2 languages for analysis are reported elsewhere (15), including the methods to: prepare forward- and back-translations of consent documents and recruitment materials in Setswana and English, conduct interviews with interpreters, transcribe and translate interviews, and work with these data for analysis.
To enhance credibility and trustworthiness of the analysis, MH consulted with key informants (including interpreters, transcriptionists, dikgosi, health education assistants and nurses) during fieldwork to examine her understanding of the cultural context for observations and interviews about MSK conditions. Upon returning from the field, MH regularly reviewed and discussed analysis and interpretation with co-authors and professional colleagues experienced in qualitative data analysis.
We aimed for transferability by developing an early familiarity with village culture (25), providing detailed contextual relationships about fieldwork (15), and generating thematic concepts about MSK burden among rural Batswana. For qualitative research about chronic illness, Conrad purports that “generalizability is in terms of concepts rather than in terms of samples (or data per se)” (26). Thus, the reader will need to consider whether the thematic concepts we created about the villagers interviewed who have MSK conditions differ from villagers in other rural Botswana communities or other LMIC settings.
Ethical considerations
The Botswana Ministry of Health, Health Research and Development Committee granted ethics approval (HRDC 00735) for this study and, as is customary in Botswana, the dikgosi from the 3 main wards granted permission to conduct the study in their village. All participants provided written informed consent before the first interview. Women are addressed as Mma and men as Rra in Botswana; this convention, along with sequential letters of the English alphabet, is used in the findings as participant pseudonyms.
RESULTS
Villagers resoundingly linked the perceived cause of their MSK troubles to hard work in everyday activities and typically described MSK symptoms with an insidious onset as opposed to any single, remembered biographical shift or disruption. Varying degrees of hardship contributed to co-existing accounts for the significance and consequences of chronic MSK conditions. Thus, the analysis of our findings for everyday MSK burden weaves meaning as consequence and meaning as significance constructs into 3 themes: (i) hard work for traditional lives; (ii) bearing the load of a rugged landscape; and, (iii) caring for others with disrupted lives (Fig. 1). While meaning as consequence predominates in villager accounts, meaning as significance is implied for the loss of independence and shifts in social identity.
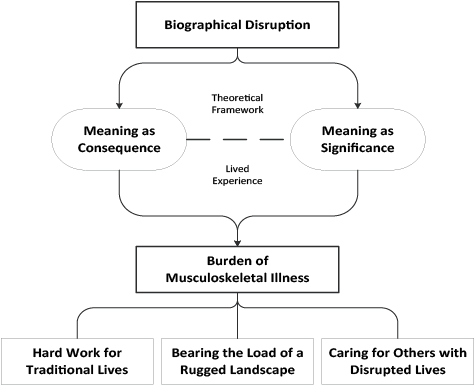
Fig. 1. Conceptual model for the burden of musculoskeletal illness in rural Botswana.
Hard work for traditional lives
When asked about the cause of MSK troubles, most villagers initially responded “Ah! I don’t know”. However, with prompts such as “according to your assumptions, what causes the troubles?” work demands for everyday activities prevailed. For many daily traditional duties, such as sweeping the yard or kgotla floor, weeding, harvesting crops, and moulding bricks, villagers sustain distinctive postures, bent at the waist beyond 90°, often with knees locked in extension, while performing their task.
Rra C described penetrating and stabbing “waist pains” (depicted in the low back and bilateral sacroiliac regions) along with upper and lower extremity pains that, at times, were perceived as being “attacked by cramps and feeling exhausted”. After some thought, he too described how traditional chores aggravate his MSK pains:
“Chopping (trees) and this and that.. or maybe firming up my kraals (livestock enclosures). But most of the time it’s provoked by working because I do hard labour. I construct brickwork, I shore up the kraals.” [Rra C, age 56 years]
Mma L cited physical work, bodily positions and vibrations associated with transport during work for the government sponsored drought relief programme (Ipelegeng) as the source and exacerbation of her MSK pains:
“We women always carry heavy things, use the wheelbarrows, carry firewood, sometimes we put the firewood in the wheelbarrows and then push… it becomes heavy. Sometimes we brew beer and stir in the drums… Yes, you bend a lot when you’re making [the brew] since you have to stir and stir so many times… and I think it’s the works we do, like clearing the yard and even loading the stones [for Ipelegeng]. I suspect it is caused by the fact that as we go, the tractor shakes us like this [demonstrates shaking her torso, upper body and head] now worsening the pains.” [Mma L, age 47 years]
Villagers revealed a great deal about their lives as they described perceptions of pain and perceived causes for MSK troubles as significant in their lives. Physical work held economic and subsistence consequences that contributed to meaning as significance with a loss of independence for many villagers. For example, Mma A now relies on others for income and sustenance:
“What I think is these pains were caused by working too much as I survive by my hands. I usually cut grass, get hired by others; some even buy grass from me. Yes madam, I used to cut grass. Construct houses. Now, all those, it’s impossible to do them because of these pains on me. I pounded sorghum with mortar and ate it. Now I can’t pound because of these pains on me. It has been two years since I haven’t worked with the soil [to construct thatched houses], not pounding [harvested grain], not going for grass cutting/harvesting. My child, only one of them is working… she throws me a bit of maize meal… a bit of sugar to go sip (some tea).” [Mma A, age 58 years]
Economic survival and physical labour were consistently linked to MSK pains as sources of biographical disruption that held consequences for villagers’ ability to participate in everyday routines that shaped their lives.
“When the pain starts, this (work) at the lands is the routine and it’s burdensome. A! I am someone who lives by manual work, madam. I plough… with difficulty… because if we don’t plough, what (will we have) to eat?” [Mma O, age 72 years]
Juxtaposed with the burdensome features of physical labour and MSK troubles, a few villagers talked about how physical work was perceived as exercise helping to reduce their pains, such that the pain “gets silent.” Others revealed challenges and hardship working through or with the pain, as these villagers explain:
“Yes it becomes very painful and limits me to work, but I work anyway. I won’t have any choice but it is not really comfortable… things like building.” [Rra C, age 56 years]
“(the pain) gets provoked even though I just keep on trying. Yes, Madam, I weed, I collect soil… I just force the situation.” [Mma H, age 83 years]
The foregoing excerpts suggest that the burden of MSK troubles reflects meaning as consequence in terms of the impact on everyday life. While meaning as significance is only implied for the loss of independence to perform socially accepted traditional duties, these examples also illustrate the importance for understanding the sociocultural value of hard work for traditional lives that MSK pain interrupts on a daily basis. Moreover, while labour-intensive lives with chronic pain has important productivity consequences, rehabilitation activities aimed at improving MSK health during traditional duties may resonate with villagers. Next, we turn to the impact the environment has for MSK burden.
Bearing the load of a rugged landscape
The cultural norm for most villagers is to live in compounds with permanent structures or yards and to maintain temporary dwellings at the lands (agricultural fields) and cattle posts. Without running water and electricity in many homes and most temporary shelters, villagers must collect water to drink, as well as water and firewood for bathing and cooking. Water sources are scarce in a rocky landscape desiccated by high temperatures and drought. During rainy seasons, many sandy roads are impassable. Some participants specifically linked fetching water to their MSK pains:
“I bend down, take it [water container] and put it in the wheelbarrow; then I take the other one put it on top… [each container is] 20 litres… It’s just that I would be going through the sand.. and it [right arm] gets painful and feels numb. And it spreads through this whole [right] arm feeling numb and painful.” [Mma R, age 42 years]
Walking is the primary mode of transport in and around the village. Many participants cited walking as an aggravating factor for their MSK troubles with some variation of “Yes, I can walk, it’s just that it is difficult”. Mma E routinely walks 10 km from her village home to the lands because she cannot afford taxi or bus rides. “Ah, these ones (legs)… maybe its when I have walked from Otse on foot to Lephepe. So when I come back that’s when my legs feel painful,” she said. Another participant speculated:
“I don’t know whether maybe it’s walking a lot because I reach over there at the cattle post… it’s a bit distant [20 km]. Actually, I also walk carrying something on my back.. Yes when I carry a lot, even the baby I don’t know whether it’s the pressure from that.. the weight from it.. [and] when at the cattle post.. we usually fetch water, we fetch it far! We actually carry a lot of stuff that’s kind of heavy and take it to whichever cattle post we stay at.” [Mma F, age 32 years]
While a few accounts related MSK troubles to road traffic or donkey cart accidents, most traumatic incidents included carrying loads while walking and navigating the landscape that held everyday mobility and food preparation consequences:
“Yes since we are people whom you would say you are going to fetch some firewood, yes so I was tripped by a small wood and I fell. Yes, sometimes you can just fall and you will always wonder what could make an elder fall? But if I don’t fetch firewood, what can we eat?” [Mma Q, age 66 years]
Here again, bearing the load in a rugged landscape emphasized meaning as consequence for the burden of MSK symptoms. However, in 1 account, the functional limitations of waist (low back) and knee pain along with the prospect of traversing rugged terrain held meaning as significance for Mma K’s social identity:
“I am failing to walk. Others will be saying [I] am too lazy to walk. Even when there is a kgotla meeting like yesterday, being said that there was a meeting, I was just here. I didn’t go anywhere. Ai! Madam! It is painful, even walking is difficult. There are no paths with no pits and rocks. I could not attend the important meeting.” [Mma K, age 77 years]
For additional accounts where MSK burden influences shifts in social identity, or meaning as significance, we present 3 villagers who care for others.
Caring for others with disrupted lives: Shifts in social identity
Ageing, HIV, AIDS and other co-morbid conditions intertwined with traditional lives that included caring for others, economic survival, psychosocial stress and environmental factors – all yielded multiple biographical disruptions that compounded the everyday burden of MSK troubles. These factors were not delivered in a linear manner, but were embedded in their stories. While meaning as consequence prevails with descriptions aligned to the preceding themes (hard work for traditional lives and bearing the environmental load), the 3 examples provided next also portray how MSK burden holds meaning as significance with shifts in social identity.
At age 55 years, Mma M is the primary caregiver for her husband whose life was disrupted when he was injured in the South African mines in the 1980s, “he has pains in the legs and waist; he does nothing; he should be here [at the interview] too, but he just sits and does nothing”. Mma M also cares for 3 grandchildren at home, “their [two] mothers were massacred by the [AIDS] virus”. She initially described MSK pains in her waist, knees, neck and shoulders along with headaches and offered age as a potential source, remarking, “I don’t know whether it’s growing up. Because it also has its own impact”.
Mma M then described everyday activities, in which she sweeps the yard, cleans community centres, weeds and harvests the lands. As the rains destroyed their home last year, her family shares a 1-room dwelling as temporary housing. Her family is unable to pay others to construct a home. Her MSK pains limit her abilities, yet she spoke with pride and spirit about what can happen if she “just works through (MSK) troubles”. When asked, “what do you want to do that you can no longer do because of your pains?” she remarked:
“Ah! It’s to construct mud houses since we Batswana, it is a custom to have a mud house. I just have wishes of making it and if I may happen to mould the bricks, still it’s impossible to lift them up. The arms were the ones that were painful… yes, if I attempt to do something heavy. And also making a lelwapa (low wall structure near traditional hut/house) is something that I envy and wish to do a lot. And to weed, yes, so that sorghum (crops) can be in a good condition.”
While the consequences of Mma M’s pains echo the theme of hard work for traditional lives, she also perceived the potential for a shift in her social identity:
“Yes, Madam, it’s just that we have a Setswana [sic] tradition we believe in that you should always have the house that you made by your own hands, the one you clean and looks appealing to the people. But I cannot manage, which means now people will be looking and saying “she is lazy”.” [Mma M, age 55 years]
The multiple biographical disruptions and psychosocial stress for bearing the societal load of day-to-day existence were not unique to Mma M. In another account, Mma T told us about her 4 children who work in Gaborone and Francistown, yet they do not contribute to the maintenance and care of their village home or family members. Nine years ago, Mma T left her paid job in Gaborone and returned to the village to care for her mother. She talked about her struggle to care for her, now, 92-year-old mother, compounded with caring for her 42-year-old daughter and 7-year-old granddaughter for the past 3 years.
“I have some stress because I am caring for my mother alone. I have a child who used to help but she is also sick, she has high blood [pressure] and the [AIDS] virus. [crying] For my mother, I bath her, I cook for her, I give her medications at the right time… When she wakes up she will just sit like this. I am the one to help her sit [and] change positions. Now, my daughter too only lies in bed, I must care for her.” [Mma T, age 68 years]
Mma T was tearful and cried during much of the interview as she described persistent waist (low back) aches, (upper) backache, and painful knees bilaterally. Her knees especially give her trouble, as she maintains traditional chores at her village home, weeds at the lands, and cares for her mother and daughter. Another precipitating event occurred the week before the interview, as she recounted being forced to repair her roof before the rains:
“I did some hard work… thatching… it was so windy that the wind was going against us with the sheaves in our hands, pushing us the opposite direction in the sense that by the time we finished, the knees, shoulders, backs were painful. After that I cooked, after that to bath my mum and daughter [sobbing], and I have realized that the pains are like this because of overworking.” [Mma T, age 68 years]
While outmigration for economic survival is common for the middle generation, the villagers left behind often feel the burden of the absence of their adult children. Mma V, age 83 years, suffers from bilateral knee pain diagnosed as “severe arthritis.” With the departure of her house helper for the Christmas holiday, Mma V was left to care for her bedridden husband of 93 years. Her children work in “the cities” and:
“They do not help, not with money and not with caring for the old man! And they must work the lands! I cannot do that. You see? And I can’t just leave him (her husband) without bathing him. I said this task is big! It involves bathing, taking off his nappies, lifting him. So now I am saying to you, because I am old, even these pains that come to me, I might die. I have grown too old.” [Mma V, age 83 years]
DISCUSSION
Through our ethnographic approach to studying MSK burden in Botswana, we found that physical labour, harsh living conditions, and caring for the very young and very old by rural villagers who also are advancing in age, contributed to co-existing accounts of the consequences and significance of the everyday burden of MSK. These findings are in contrast to earlier epidemiological evidence, which suggested that physical labour might be protective for low-back pain in low-income countries (27). Our findings are in line with studies that depict MSK debility from extensive work demands in subsistence communities (2) and that report that activities such as collecting and carrying water and farming (28, 29) contribute to an increased prevalence or risk for MSK conditions.
Most villagers responded to questions about their muscles, bones and joints as if no one had ever asked them about their pains. Although respondents eventually postulated causes for their MSK troubles, we found no evidence that they sought the diagnostic or existential meaning of symptoms, often inseparable searches from sufferers who might ask “what is the name for this condition?” or “why me?” and “why now?” (11, 30, 31). Rather, MSK troubles were attributed to the hard work associated with their everyday lives. Thus, while the temporal sequence related to the onset and diagnosis of MSK conditions was not born out by villager accounts, “the changed relationship between body, self and society” (32) was evident for villagers who identified that MSK troubles impact their ability to perform traditional work to earn income and for subsistence.
Our interpretive lens applied Bury’s seminal work about the biographical disruption of chronic illness (11), and his later distinction between “meaning as consequence” and “meaning as significance” (12). Although we did not diagnose respondents with particular medical conditions or disabilities, villagers’ stories conveyed MSK troubles as the source of a myriad of consequences in their everyday lives, whereby the “perceived character” of functional limitations held significance for the “cultural competence” (12) to enact everyday traditional duties for survival and pride in their lives.
Villagers typically described MSK symptoms with an insidious onset as opposed to any single, remembered biographical shift or disruption. Traditional chores along with environmental factors were disclosed as aggravating factors for MSK troubles, yet many villagers continued daily routines working with pain. Most participants relied “on subsistence farming, helping out on other people’s farms for food or money, or brewing traditional alcohol for sale” (33). Many maintained dwellings without electricity or running water. Villagers take pride in fulfilling traditional duties such as sweeping their yards on a daily basis; weeding the lands so crops can prosper; harvesting crops; building and re-building dwellings in the village, at the lands and at cattle posts that do not survive the harsh climate; and, chopping trees, gathering firewood, fetching water for basic necessities. Labour-intensive lives exacerbate the meanings and consequences of physical ailments. When MSK troubles alter, limit or prevent these activities, villagers endure shifts in social identity that contribute to poor quality of life.
Added to these hardships are the multiple biographical disruptions that underpin valued roles as caregivers and receivers of care. The responsibility to care for others manifested in several accounts and was perceived to exacerbate MSK symptoms. Caring for others – the old, very old, the young and very young – adds to the burden experience and alters the social identity for Batswana, many of whom also are living with HIV, AIDS and other co-morbid conditions, along with progressively worsening MSK symptoms. Several villagers became emotional as they described their struggles to care for orphaned children, adult children and elderly family members, principally due to outmigration of other family members seeking wage work or due to incapacitating illness or death. Everyday muscle, bone and joint pains along with the psychological and emotional needs of the people who give and receive care and the lack of MSK specialists in country alter a most basic, yet universal, value: that Batswana need to be needed, that they have a purpose in life.
Others have argued that Bury’s work with relatively young individuals with rheumatoid arthritis may not be applicable to older adults’ illness experiences. Pound et al. (34) examined older, working class stroke survivors and, while stroke had considerable impact on activities of daily living, some respondents “already accustomed to hardship, illness and death” did not experience stroke onset “as an extraordinary event in their lives”. For our respondents, it is conceivable that accumulated life experiences with poverty, outmigration, HIV and AIDS mediated the perceived significance of MSK disorders, yet the consequences for MSK troubles appear to be substantial for Motswana lives.
Similarly, respondents in Sanders et al.’s (13) study of older adults with osteoarthritis viewed their symptoms “as a normal and integral part of their biography”, yet also described how symptoms disrupted their daily lives. Although our respondents did not articulate their MSK experiences as a “normal” part of ageing, given the recurring languaging of “traditional duties” it is plausible villagers have accepted MSK troubles as integral to the physical labour and varying degrees of hardship in their lives.
Broad constructs of restricted activities and carer burden are not included in the burden of disease estimates (2). This, alongside many MSK conditions classified in alternate categories for burden of disease, probably leads to an underestimate of the full burden from MSK disorders, currently estimated as 20% of all disability in developing countries (2). More than 20 years ago, Ingstad and colleagues (35) foreshadowed dramatic changes to the viability of rural households in Botswana, predicting that outmigration for career opportunities along with devastating effects from the AIDS epidemic would claim the lives of a substantial number of the middle generation, impacting the already heavy burden of care for elderly women. More recently, Shaibu (33) reported profound consequences for grandmothers caring for orphan grandchildren in Botswana. Similar to our findings, poor health, including MSK aches and pains, and the lack of social support and caregiving from extended family members limited grandmothers’ ability to engage in manual labour, earn income or participate in subsistence farming.
Our study contributes to the physical medicine and rehabilitation literature by explicating the everyday burdens of MSK disorders in local context. Our findings “illustrate the importance of understanding an individual’s social reality” (31) that is grounded in traditional activities when considering clinical and epidemiological parameters by which to account for the burden and prognosis of MSK conditions in people’s lives in LMIC settings. This work also has practical implications for assessing what really matters to patients with adequate outcome measures (36) and designing and sustaining effective preventive and therapeutic rehabilitation programmes, using real-life activities (37) to improve MSK health and quality of life. This foundational research effort resonates with Willems’ commentary (38) reflecting on quality of life studies for people with disabilities, in which he remarks, “If you really want to know about the quality of the lives people with (chronic diseases or) disabilities lead, listen to them! Don’t start measuring them!”
Strengths and limitations
Similar to clinical trial and systematic review protocols, yet unlike many ethnographic studies, we published a detailed account of the project context and methods in an open access publication (15), allowing clinicians and other researchers to better understand the extensive preparatory work required for qualitative studies abroad such as this. We made 3 data collection trips to Botswana over 3 years, during which we cultivated collaborative relationships and trust with villagers and village ward chiefs. This rapport-building process gave the villagers repeated opportunities to speak informally with the researcher before engaging in formal interviews in which many spoke about the intimate details and hopes for their everyday lives. Our team also worked with local Batswana who participated in the project as translators, interpreters and transcriptionists. These collaborations allowed us to learn from villagers who did not speak English, contribute financially to the local economy, and develop research skills in community members to promote the long-term sustainability of the NGO spine care clinic.
A limitation of this study is that we did not have Motswana investigators. Although there are few MSK specialists in Botswana, enlisting the collaboration of frontline primary care providers, most often nurses and traditional healers, who are raised, trained and apprenticed in Botswana, will strengthen investigative teams. In addition, it is possible that significant social connotations for MSK burden were lost in translation and that these concepts are more meaningful than we interpreted. Thus, attaining fluency in Setswana will reduce systematic errors in our ethnographic interpretations (39). However, given the large number of expatriate physicians in the healthcare sector, the cadre of NGO volunteers who serve short terms of service without learning Setswana, and the few numbers of physical medicine and rehabilitation specialists in country (40), we believe that our contribution to understanding the burden of MSK conditions in the local context is valuable.
Conclusion
Villagers in rural Botswana perceive the hardships of everyday life as the source of their MSK troubles. The meaning as consequence for MSK conditions encompasses increasing difficulties with cultivating subsistence for one’s self and one’s family, often compromising the care of orphans and elderly for which an individual has supportive obligations. This reduced capacity or lack of ability to carry out traditional chores expected of the person with MSK conditions, leads to meaning as significance including social degradation and the fear of not being acknowledged as a full and able member of society. Data from this study have the potential to inform government and NGO initiatives where we partner with community members to develop research, educational and care pathways delivered by villagers for villagers to improve MSK health.
ACKNOWLEDGEMENTS
Re a leboga to the villager participants who shared their stories with us and to the Batswana who served as translators, interpreters and transcriptionists. Special thanks also to Dr Stacie Salsbury for her critical assessment of the project and insightful comments to early manuscript drafts. This study was funded by the Danish Foundation for Chiropractic Research and Postgraduate Education (grant number 11/102) and the University of Southern Denmark, Faculty of Health Sciences. During her doctoral programme, MH also received support from World Spine Care, Palmer College of Chiropractic and the NCMIC Foundation.
REFERENCES
