Andrea D. Furlan, MD, PhD1,2,3, Samah Hassan, MD, MSc3, Ida-Maisie Famiyeh, BScPhm4, Wendy Wang, BSc (Hons)1 and Jaspreet Dhanju, MD1
From the 1Musculoskeletal Program, Toronto Rehabilitation Institute, University Health Network, 2Division of Physiatry, Department of Medicine, 3Institute of Medical Sciences and 4Faculty of Pharmacy, University of Toronto, Toronto, Canada
OBJECTIVE: To determine: (i) the prevalence of opioid-naïve patients discharged on opioids from a musculoskeletal rehabilitation inpatient unit; (ii) the prevalence of opioid use 6 months after discharge; and (iii) the efficacy of the Opioid Risk Tool in identifying long-term opioid use.
DESIGN: Prospective study.
PARTICIPANTS: Sixty-four opioid-naïve patients who were exposed to opioids during admission and who were discharged on an opioid.
METHODS: Potentially eligible patients’ charts were reviewed. Participants were interviewed during admission to obtain the opioid risk score and contacted 6 months after discharge via a semi-structured telephone interview.
RESULTS: Twenty-eight percent of opioid-naïve patients, who were discharged on opioids were still using opioids 6 months after discharge from rehabilitation. There was a trend for higher Opioid Risk Tool scores in those still using opioids than in individuals who were not using opioids at 6 months (p = 0.053).
CONCLUSION: Patients who are prescribed opioids during a hospital admission should be screened for risk of opioid misuse. This data suggests that the Opioid Risk Tool could identify a patient’s potential for becoming a long-term user of opioids.
Key words: chronic opioid therapy; musculoskeletal rehabilitation; chronic pain; post-operative pain; opioid; prospective study.
J Rehabil Med 2016; 48: 00–00
Correspondence address: Andrea Furlan, Toronto Rehabilitation Institute- UHN, 550 University Avenue, Room 7-141-1, Toronto ON Canada M5G 2A2. E-mail: Andrea.furlan@uhn.ca
Accepted Feb 10, 2016; Epub ahead of print Mar 22, 2016
INTRODUCTION
Acute trauma, total joint replacement, and multiple fractures are among the most disabling and costly musculoskeletal conditions (1). If managed inadequately, they may reduce work productivity and increase unemployment rates of a large proportion of the working population (2, 3). Nevertheless, with appropriate physical rehabilitation, many patients can restore some or all of the physical, sensory and mental capabilities that may be lost due to injury, illness or disease, and retain their productive lives (4, 5). Therefore, these conditions are usually referred to physical rehabilitation centres.
Unfortunately, rehabilitation therapy can be stalled by pain (6). The pain experienced during rehabilitation can be extreme and enough to discourage patients from complying with their rehabilitation interventions (7). Therefore, the use of opioid analgesics, although undesirable, is considered essential to reduce pain, improve function, prepare the patient’s reintegration into the community and reduce the length of hospital stay (6, 8).
In Canada, physicians have begun prescribing opioids at unprecedented rates for acute and chronic pain conditions, with an increased prescription rate of oxycodone of over 500% between 1997 and 2006 (9). Although very effective to treat acute pain conditions, opioids have significant risks of addiction, overdose and potential for misuse (9, 10). Therefore, it is important that patients are properly screened for risks and monitored closely over the course of their rehabilitation.
Various screening tools have been developed to assess the potential vulnerability for patients to develop aberrant behaviours. One method of determining a participant’s potential for displaying aberrant behaviours is by administration of a risk stratification tool, such as the Opioid Risk Tool (ORT) (8). The ORT entails 5 self-reported items used to predict the probability of a patient displaying aberrant behaviours when prescribed opioids for pain control. The ORT is generally recognized by clinicians as a quick way of assessing patient’s potential for developing drug-related aberrant behaviours. However, there has been criticism of the validity of the ORT in predicting these risks with accuracy (11). There are other tools that have been developed to predict risks of opioid-related aberrant behaviours (The Screener and Opioid Assessment for Patients with Pain (SOAPP)® (12, 13), and all of these tools agree that patients with a past history of substance use disorder are at higher risk of developing aberrant behaviours after long-term use of opioids; however, several studies have demonstrated that opioid-naïve patients may also display aberrant behaviours and become addicted to prescription opioids (14, 15).Therefore, despite many endeavours to make risk assessment in clinical practice, there is relatively little empirical data about the measures’ ability to assess and predict risk among opioid-naïve patients.
It is expected that opioid-naïve patients with no past history of chronic pain who were prescribed opioids during a short admission to hospital should not be using these potent medications for a prolonged period. Most specifically, a few months after discharge following acute trauma or musculoskeletal rehabilitation, patients should no longer be taking opioids, as healing is expected to have completed, the injury has resolved and patients should have returned to their baseline level of functioning and pain tolerance. If patients are still using opioids at this time, it is possible that they have developed chronic pain, opioid dependence, or became addicted to these medications. Following discharge from musculoskeletal rehabilitation, patients are usually followed by their primary care clinician who may have little training in tapering opioids, to assess risks of opioid misuse or to diagnose a substance use disorder.
The objective of this study was to include opioid-naïve patients with no past history of chronic pain in a musculoskeletal inpatient rehabilitation unit to determine: (i) the proportion of patients discharged on opioids; (ii) the prevalence of ongoing opioid use 6 months after discharge; and (iii) whether the ORT scores were able to predict users and non-users of opioids at 6 months post-discharge.
METHODS
After obtaining approval from the Ethics Review Board at Toronto Rehabilitation Institute, patients admitted to the Musculoskeletal Rehabilitation Unit of the Toronto Rehabilitation Institute were prospectively recruited. This unit receives patients mostly from orthopaedic wards within our hospital (University Health Network) or from other hospitals. The recruitment period occurred from October 2011 to September 2013.The inclusion ctiteria were: age 18 years or older, fluency in English, with neither a diagnosis of chronic pain nor past history of opioid treatment prior to admission, with oral opioid therapy during admission for acute pain managment, and with opioid prescription at discharge for pain managment to be obtained from the community pharmacy.
Initial contact with potential participants
The hospital staff involved in the circle of care of a potential participant were asked to approach potential participants to determine if they were willing to talk to a member of the research team.
Baseline data
For those individuals who agreed to be approached, a researcher explained the study, obtained consent and applied the ORT. The ORT was completed by the patients themselves, with the option of obtaining assistance from the researcher.
Chart reviews
Data from the participants’ charts were extracted regarding demographics, previous history of chronic pain, pre-admission opioid use, reason for admission, type of surgery or intervention, current opioids and dosage during hospital stay, and medications at discharge.
Six-month telephone interview
Those patients who were discharged on opioids and were not opioid users prior to admission, were contacted 6 months after discharge via a semi-structured telephone interview. At the 6-month interview, participants were asked to answer questions regarding their pain and opioid medication usage, including duration, type and dosage.
Data analyses
Descriptive statistics and prevalence rates were calculated in Microsoft Excel®.
RESULTS
Demographics
The staff approached 362 potential patients, of whom, 135 (37%) consented to participate (Fig. 1). Of those who consented, 34 (25%) were chronic users of opioids, while 101 (75%) were opioid naïve. Of the opioid-naïve patients, 37 (37%) were not discharged on opioids, leaving 64 (63%) patients who were discharged on opioids. The 64 eligible patients (opioid naïve, no past history of chronic pain and discharged on opioids) were 26 (41%) males and 38 (59%) females, with a mean age (standard deviation; SD) of 71 (14) years (age range 24–89 years). Of 64 eligible participants, 20 (31%) dropped out of the study, for many reasons, leaving a final total of 44 (25 females and 19 males) participants (Fig. 1).
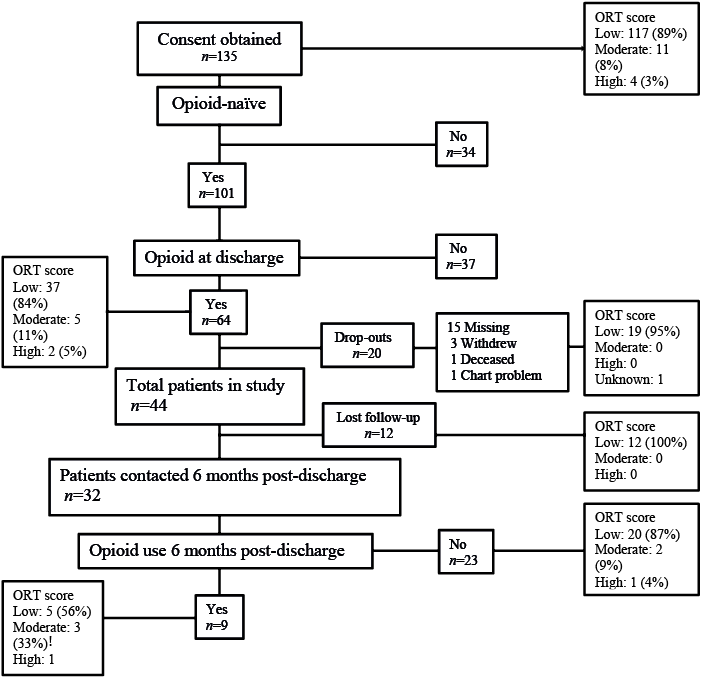
Fig. 1. Patients’ disposition and scores on the Opioid Risk Tool (ORT).
The 44 participants were admitted to the Toronto Rehabilitation Institute – Musculoskeletal Program for various reasons: fractures, trauma and joint replacements (Table I), and the mean (SD) duration of hospital stay was 39 (51.4) days. The mean (SD) age for the 44 participants was 69.1 (13.9) years. Of the 44 participants, 37 (84%) scored low, 5 (14%) scored moderate and 2 (5%) scored high on the ORT (Table II). At discharge, the opioid medications prescribed to the 44 patients were: hydromorphone, oxycodone, codeine, and tramadol (Table III); with a daily morphine equivalent dose at discharge ranging from 5 to 360 mg, with a mean (SD) of 82.1 (72.4) mg.
|
Table I. Diagnosis for participants |
|
|
Diagnoses |
Participants n = 44 n (%) |
|
Knee replacement |
16 (36) |
|
Hip fracture |
15 (34) |
|
Trauma/multiple fractures |
6 (14) |
|
Complex medical condition |
3 (7) |
|
Hip replacement |
3 (7) |
|
Acetabular fracture |
1 (2) |
|
Table II. Opioid Risk Tool results |
||
|
|
Total 44 patients |
|
|
Male n = 19 n (%) |
Female n = 25 n (%) |
|
|
Are you aware of any family history of substance abuse? By family I mean 1st degree relatives, so this includes your mother, father, siblings, and children. Substance abuse can include alcohol abuse, illegal drug abuse, and/or prescription drug abuse. |
||
|
Alcohol |
6 (32) |
4 (16) |
|
Illegal drugs |
1 (5) |
0 |
|
Prescription drugs |
0 |
1 (4) |
|
Have you ever had any history of alcohol abuse, illegal drug abuse, or prescription drug abuse yourself? |
||
|
Alcohol |
2 (11) |
2 (8) |
|
Illegal drugs |
0 |
0 |
|
Prescription drugs |
1 (5) |
1 (4) |
|
Age (if 16–45) |
1 (5) |
2 (8) |
|
Were you sexually abused as a child prior to the age of 12? ONLY TO BE COMPLETED BY FEMALE PARTICIPANTS |
|
1 (4) |
|
Have you ever been diagnosed with or treated for any of the following conditions? |
||
|
Attention deficit disorder Obsessive compulsive disorder Schizophrenia Bipolar disorder |
2 (11) |
0 |
|
Depression |
5 (26) |
2 (8) |
|
Total score |
|
|
|
High (≥ 8) |
1 (5) |
1 (4) |
|
Moderate (4 to 7) |
4 (21) |
1 (4) |
|
Low (0 to 3) |
14 (74) |
23 (92) |
|
Table III. Opioid use in patients |
|
|
Opioid type at discharge |
Participants n = 44 n (%) |
|
Hydromorphone |
26 (59) |
|
Oxycodone (SA) + acetaminophen |
11 (25) |
|
Oxycodone 10 mg (SA) |
1 (2) |
|
Oxycodone 20 mg (LA) |
2 (5) |
|
Codeine 30 mg (LA) |
1 (2) |
|
Tramadol |
1 (2) |
|
Codeine 15 mg + acetaminophen |
1 (2) |
|
Codeine 30 mg + acetaminophen |
1 (2) |
|
LA: long-acting; SA: short-acting. |
|
Six months post-discharge, all 44 participants were contacted via telephone to determine the persistent use of opioids post-discharge. Thirty-two patients (73%) responded. Twenty-three of the 32 (72%) participants had stopped using opioid medications, while 9 (28%) were still using opioids: 6 females (67%) and 3 males (33%).
Five (56%) patients were admitted for hip fracture, 2 (22%) for total knee replacement, and 2 (22%) for trauma and multiple fractures. The mean (SD) age was 70.4 (11.9) years, age range 52–86 years. Six (66%) of the 9 patients still using opioids had leftovers from their original opioid prescription, while 3 (33%) had no leftovers. Eight (88%) used hydromorphone, and 1 (11%) used codeine, with a daily morphine equivalent dose ranging from 5 to 108 mg, mean (SD) dose 53.3 (32.0) mg.
Among the 9 participants who were using opioids at 6 months post-discharge, 5 (56%) scored low, 3 (33%) scored moderate, and 1 (11%) participant scored high (Fig. 1). In contrast, among the 23 participants who stopped using opioids 6 months post-discharge; 20 (87%) patients scored low, 2 (9%) scored moderate and 1 (4%) scored high. Although there was a trend showing that 87% of participants who stopped using opioids 6 months post-discharge scored low on the ORT, 44% of those who continued using opioids scored moderate and high on the ORT.
DISCUSSION
Over recent years there has been growing concern about prescribing opioids at discharge from hospitals or rehabilitation centres after major surgery and trauma. Although very effective to treat acute pain, opioids comprise a number of serious adverse events; including misuse, abuse and/or addiction, as well as the possibility of inappropriately prolonged opioid use, and diversion (11, 16). Therefore, various screening tools have been developed to assess the potential vulnerability of patients to develop aberrant behaviours. Most, if not all, of these tools have agreed that patients with a past history of drug abuse are at higher risk of developing aberrant behaviours after long-term opioid use; however, several studies have recently demonstrated that opioid-naïve patients may also display aberrant behaviours and become addicted to prescription opioids (17).
In this study, we found that, among patients who were admitted to Toronto Rehabilitation Institute, out of 101 who were opioid naïve, and had no history of chronic pain prior to a rehabilitation admission, 64 (63%) were prescribed opioids at discharge,
We were interested in studying the proportion of new cases of long-term opioids generated at our rehabilitation hospital. Of the followed patients (n = 32) in our study, we found that 9 (28%) were using opioids at 6 months post-discharge, which gives an approximate prevalence of 14% for long-term opioid use among those who were opioid naïve and had no chronic pain prior to admission (n = 64). This figure is a very conservative measure because it assumes that all losses to follow-up in our sample were not using opioids at 6 months. Each year there are approximately 1,000 admissions to our musculoskeletal inpatient beds at the Toronto Rehabilitation Institute. If these numbers are accurate, we are discharging to our community 140 new cases of long-term opioid users per year. We expect that the primary care physicians seeing these patients would be responsible for tapering these opioids, finding other alternatives to manage their pain, and making appropriate referrals back to the rehabilitation physician for proper management of chronic pain if this was the case.
It is concerning that patients who continued using opioids for 6 months post-discharge had a 44% chance of scoring moderate and high on the ORT, while those who had stopped using opioids within 6 months period post-discharge had a 13% chance of scoring moderate and high on the ORT.
These results are consistent with those of other studies investigating the risk of prolonged opioid use among opioid-naïve patients. Alam et al. conducted a retrospective study of opioid-naïve patients aged 66 years or older who had short-stay operations, such as cataract surgery, laparoscopic cholecystectomy transurethral resection of the prostate or varicose vein stripping, and were prescribed an opioid within their hospital stay and at discharge (18). Alam et al. found that more than 10% of patients prescribed an opioid after surgery were still taking an opioid 1 year later: Similarly, Singh & Lewallen (19) found that 2.3% of patients who had undergone primary total hip arthroplasty and were alive at the time of the 2- or 5-year follow-up reported continuing use of opioids at 2 years,
In 2014, Clarke et al. (15) conducted a population cohort study with 39,140 opioid-naïve patients aged 66 years or older who had major elective surgery in Ontario, Canada. The main outcome measure was prolonged opioid use after discharge for more than 90 days after surgery. They found that 49.2% of the patients were discharged with an opioid prescription, and 3.1% continued to receive opioids for more than 90 days after surgery.
All these studies, including ours, while still limited in the number of participants and loss to follow-up, suggest that post-surgical and/or rehabilitation discharge opioid prescribing intended for short-term management of acute pain can result in unintended initiation of long-term opioid use in some patients, Moreover, our study showed that ORT might be a promising tool to predict the risk of prolonged opioid use post-discharge; however, this needs to be confirmed in larger samples.
While our study was limited by the small sample size and high rate of loss to follow-up, the main strengths of the study are the detailed risk assessment during hospital admission and the personal telephone interview at 6 months follow-up. The results of this study are relevant to rehabilitation units where there is a high rate of opioid prescription during admission. This study highlights the concerns of opioid prescription at discharge and the possibility of long-term use of opioids post-discharge. Patients prescribed an opioid at the time of discharge are at risk from potential serious side-effects, including death, abuse and addiction, even among opioid-naïve patients. Therefore, physicians, nurses and pharmacists need to be aware of the risks associated with discharging patients with a prescription of opioids. There should be an assessment made of the risks of opioid abuse and diversion in any patient started on opioids for management of their acute pain, especially in those being discharged from hospital who may require continuing management of their pain. Where the risk of prolonged use is assessed as being high, follow-up may be required and limitations placed on the availability of opioids by prescription. Primary care clinicians need to be trained on how to taper opioids, to identify the incidence of chronic pain and offer alternatives to manage chronic pain, which may or may not include opioids, and also to identify high-risk patients and those who are misusing or abusing opioids. We hope that by raising attention to this important topic further research will take place to provide more evidence and recommendations for opioid prescription at discharge from hospitals.
The authors have no conflicts of interest to declare.
REFERENCES
