Cecilia Wai Ping Li-Tsang, PhD1, Cheng Qi He, MD, PhD2, Amy Gee Wai Lo, MSc, MSocSc1, Sai Jun Ding, MA1, Xue Deng, BSc1, Yong Hong Yang, MD2 and Yu Ting Zhang, BSc2
From the 1Department of Rehabilitation Sciences, The Hong Kong Polytechnic University, Hung Hom, Kowloon, Hong Kong SAR and 2Department of Rehabilitation Medicine, West China Hospital, Sichuan University, Sichuan, China
OBJECTIVE: To determine the physical, functional and psychosocial rehabilitation needs of the injured survivors of the 2013 earthquake in Ya’an, China.
DESIGN: Cross-sectional survey.
METHODS: A total of 143 injured survivors (80 males, 63 females, mean age 41.4 years (standard deviation (SD) 20.2)) were recruited for the study. A questionnaire was designed to collect their demographic and environmental information. Manual muscle testing and active range of motion (AROM) were used to assess physical function. The Modified Barthel Index was used to assess activities of daily living (ADL) and the Post-Traumatic Stress Disorder – Self Rating Scale was used to assess psychological status. The rehabilitation needs of the injured survivors were identified based on the assessment results.
RESULTS: Physical problems of the back and lower limbs were more severe than those of the upper limbs, as measured by MMT and AROM. Various degrees of dependence in ADL were measured in 74.2% of subjects, and psychological distress was present in more than 50% of subjects. Rehabilitation training prescribed by local therapists included functional training (74.8%), exercises (49.0%), provision of splints (44.8%), etc. Psychological interventions were recommended to most of the patients. There were high levels of need for assistive devices, and home and community modifications.
CONCLUSION: There is a high level of need for early rehabilitation in hospital, followed by continued home and community rehabilitation services, particularly for injured survivors who are returning to villages with very limited resources.
Key words: natural disaster; earthquake; physical injuries; rehabilitation; needs assessment.
J Rehabil Med 2015; 47: 586–592
Correspondence address: Cecilia Wai Ping Li-Tsang, Department of Rehabilitation Sciences, The Hong Kong Polytechnic University, Kowloon, Hong Kong SAR, China. E-mail address: cecilia.li@polyu.edu.hk
Accepted Feb 18, 2015; Epub ahead of print Jun 16, 2015
INTRODUCTION
Large-scale disasters, such as earthquakes, result not only in significant loss of life, but also in large numbers of victims with various disabilities. Most victims have physical injuries, such as spinal cord injury, traumatic brain injury, limb amputation, fracture and soft tissue injury, as well as psychosocial problems, such as post-traumatic stress disorder (PTSD). Improvement in emergency rescue systems has greatly increased the survival of victims with severe and multiple-trauma injuries. However, these survivors have long-term impairments, and there is therefore a high level of need for immediate and long-term rehabilitation following a disaster. Inadequate short-term or long-term rehabilitation can result in medical complications of disabling injuries, lifetime disability, and other significant negative consequences to individuals and society (1). A comprehensive rehabilitation programme, combining institutional rehabilitation treatment and community-based rehabilitation, should be established to support survivors with disabilities following a disaster (2).
There is increasing awareness in society of the importance of rehabilitation after major natural disasters. Some studies have assessed the effectiveness of various rehabilitation programmes for different types of injuries after disasters such as the 2005 Pakistan earthquake, the 2008 Wenchuan earthquake and the 2010 Haiti earthquake. Studies from these major earthquakes have reported the effectiveness of rehabilitation in managing fractures (3–5), amputations (6, 7), spinal cord injury (8–12) and PTSD (13). A recent study reported that a combined medical and community-based rehabilitation programme provided to survivors of the Wenchuan earthquake was effective to improve their long-term physical function (14). However, early rehabilitation needs following acute medical management after disasters are seldom reported in the literature.
On 20 April 2013 an earthquake of magnitude 6.6 on the Richter scale occurred in Ya’an, Sichuan province, China, just 22 days before the fifth anniversary of the 2008 Wenchuan earthquake, which caused approximately 200 deaths and left more than 11,000 people with injuries (15). Based on experience from the Wenchuan earthquake, disaster responses to the Ya’an earthquake, including the immediate rescue of casualties, distribution of casualties to different regional hospitals, and provision of medical intervention, were all arranged in an orderly manner. More severe cases were sent to large hospitals with better and more comprehensive surgical, nursing and rehabilitation services. Less severe cases were treated in local hospitals, mainly by conservative management. The aim of this study was to understand further the patients’ rehabilitation needs, by assessing the physical, functional and psychological condition of the patients using standardized assessment tools within 3 months of admission to hospital. The assessment results, together with demographic resources, were used to identify the patients’ rehabilitation needs, and a rehabilitation programme was recommended.
METHODS
Sampling method
Patients who were injured from 420 Ya’an earthquake and admitted into 3 large regional hospitals in Sichuan province, were recruited using a convenience sampling method. Ethical approval was obtained from the hospital authorities prior to the study and assessments were conducted with the patients’ consent.
Assessment method
A questionnaire was designed to collect the patients’ demographic information. A standardized assessment protocol was used to assess their physical, functional and psychological status. Patients were also asked to provide information about their living environment (e.g. accessibility and availability of a barrier-free environment). Information such as diagnosis, types of injury and medical conditions was also obtained through the hospital information system or by querying the attending medical officers.
Physical assessment using manual muscle testing (MMT) was conducted on various body parts, including shoulder, elbow, wrist, finger joints, hip, knee and ankle. The active range of motion (AROM) of the various joints was also evaluated. The Modified Barthel Index (MBI) was used to assess activities of daily living (ADL), indicating the degree of independence of the patients (16). Eight self-care activities, including feeding, dressing and bathing, and 2 items related to their mobility (walking and going up or down stairs) were rated by the case therapists or medical doctors. For the Barthel scale, a total of 91–99 indicates minimal dependence, 75–90 mild dependence, 50–74 moderate dependence, 25–49 severe dependence, and 0–24 total dependence.
In addition, patients were asked to rate each of the 24 items of the Post-Traumatic Stress Disorder-Self Rating Scale (PTSD-SS) (17), ranging from 1 to 5 representing an increasing trend of severity. A total of less than 50 indicates a normal psychological condition, 50–59 represents mild abnormal symptoms, and 60 or above indicates moderate to severe abnormal symptoms.
Identification of rehabilitation needs
Based on the results of physical, functional and psychological assessments, and taking into account each patient’s living and environmental conditions, together with the treatments that they had received during their hospitalization, the rehabilitation needs of the patients, including their physical, psychosocial and community needs, were identified and recommendations made. Traditional Chinese rehabilitation techniques, such as acupuncture and Tui-Na, were also included in the list of interventions. Data were processed using IBM SPSS Statistic 20 and the results reported in a descriptive manner.
RESULTS
Demographic data
A total of 143 patients from 3 regional hospitals (West China Hospital (WC) = 104, Bayi Hospital (BY) = 19 and Chengdu No. 2 Hospital (C2) = 20) (80 males, 63 females) were recruited and assessed, all within 3 months of the earthquake. Their ages ranged from 6 to 87 years, with a mean age of 41.4 (standard deviation (SD) 20.2) years. The demographic characteristics of the patients are shown in Table I. Most participants were adults (76.2%) and the majority were farmers (40.6%). Approximately 40% of patients had primary education or below, while 13.3% had higher college education or above. Most survivors reported that their financial support came from personal income or savings (54.6%) or through family support (32.2%). Most patients were married (69.9%) and lived with their families (76.2%).
|
Table I. Participants’ demographic data |
||
|
Mean (SD) |
n (%) |
|
|
Age |
41.4 (20.2) |
|
|
< 18 years |
15 (10.5) |
|
|
18–64 years |
109 (76.2) |
|
|
≥ 65 years |
18 (12.6) |
|
|
Unknown |
1 (0.7) |
|
|
Gender |
||
|
Male |
80 (55.9) |
|
|
Female |
63 (44.1) |
|
|
Occupation |
||
|
Worker |
18 (12.6) |
|
|
Farmer |
58 (40.6) |
|
|
Student |
23 (16.1) |
|
|
Retired |
6 (4.2) |
|
|
Other |
37 (25.9) |
|
|
Unknown |
1 (0.7) |
|
|
Education level |
||
|
Below primary or primary school |
57 (39.9) |
|
|
Secondary school |
41 (28.7) |
|
|
High school |
20 (14.0) |
|
|
College or above |
19 (13.3) |
|
|
Unknown |
6 (4.2) |
|
|
Financial resources |
||
|
Personal income or savings |
78 (54.6) |
|
|
Family support |
46 (32.2) |
|
|
Social allowance |
7 (4.9) |
|
|
No resources |
3 (2.1) |
|
|
Unknown |
9 (6.3) |
|
|
Marital status |
||
|
Single |
42 (29.4) |
|
|
Married |
100 (69.9) |
|
|
Widowed |
1 (0.7) |
|
|
Living condition |
||
|
Independent |
11 (7.7) |
|
|
With family |
109 (76.2) |
|
Living environment
Table II describes the living conditions and environmental barriers faced by survivors. The majority lived in apartments (53.8%), mostly without a lift (74.1%), while 25.9% lived in houses and 2 patients lived in a portable dwelling. Nine patients (6%) reported that their home was no longer safe to live in due to severe damage by the earthquake, and another 9 patients (6%) reported that their housing facility had collapsed during the earthquake. Only a small percentage (7.7%) of survivors reported that they lived in a barrier-free environment, which was accessible to people with physical disabilities. Factors related to environmental barriers, such as the availability of a lift, accessibility, and types of flooring, toilet, and bathroom, were also surveyed (Table II).
|
Table II. Living conditions and environmental barriers of the victims |
|
|
Conditions |
n (%) |
|
Type of housing |
|
|
Apartment |
77 (53.8) |
|
House |
37 (25.9) |
|
Portable dwelling |
2 (1.4) |
|
Unknown |
27 (18.9) |
|
Damage to the house |
|
|
Undamaged |
20 (14.0) |
|
Unsafe to live in |
9 (6.3) |
|
Collapsed |
9 (6.3) |
|
Unknown |
105 (73.4) |
|
Barrier-free facilities |
|
|
Yes |
11 (7.7) |
|
No |
100 (69.9) |
|
Unknown |
32 (22.4) |
|
Availability of lift |
|
|
Yes |
7 (4.9) |
|
No |
106 (74.1) |
|
Unknown |
30 (21.0) |
|
Accessibility |
|
|
With stairs |
32 (22.4) |
|
Uneven road |
10 (7.0) |
|
Slope |
12 (8.4) |
|
Threshold |
11 (7.7) |
|
Multiple |
35 (24.5) |
|
Unknown |
43 (30.1) |
|
Floor type |
|
|
Wooden |
9 (6.3) |
|
Cement |
67 (46.9) |
|
Tile |
36 (25.2) |
|
Multiple |
6 (4.2) |
|
Other |
2 (1.4) |
|
Unknown |
23 (16.1) |
|
Toilet |
|
|
Squatting |
112 (78.3) |
|
Sitting |
7 (4.9) |
|
Both |
3 (2.1) |
|
Unknown |
21 (14.7) |
|
Bathroom |
|
|
Shower |
92 (64.3) |
|
Bathtub |
14 (9.8) |
|
Bath bench |
13 (9.1) |
|
Basin |
1 (0.7) |
|
Unknown |
23 (16.1) |
Physical assessments
Table III shows the clinical diagnosis, injured body parts, and cause of injuries in the survivors. The most common injures included lower limb fractures (51.7%) and spinal fractures (39.9%). It should be noted that some survivors obtained multiple injuries in various body parts, resulting in a total percentage greater than 100. The most commonly injured body parts were lower limb (53.8%), trunk (44.1%) and multiple areas (23.8%). Regarding the cause of injuries, it was not surprising that the main reasons were being hit by falling objects (30.1%) and falls (24.5%). Twenty-one patients (14.7%) were injured by jumping from a height because they were afraid of their house collapsing; some even jumped from a few floors up.
|
Table III. Types of injuries and causes of injury of the earthquake victims. (Total percentage exceeds 100% due to multiple injuries among some victims) |
|
|
n (%) |
|
|
Diagnosis |
|
|
Upper limb fracture |
25 (17.5) |
|
Lower limb fracture |
74 (51.7) |
|
Burn |
1 (0.7) |
|
Amputation |
4 (2.8) |
|
Traumatic brain injury |
6 (4.2) |
|
Spinal cord injury |
7 (4.9) |
|
Spinal fracture |
57 (39.9) |
|
Peripheral nerve injury |
2 (1.4) |
|
Other |
10 (7.0) |
|
Injured body parts |
|
|
Upper limb |
29 (20.3) |
|
Lower limb |
77 (53.8) |
|
Trunk |
63 (44.1) |
|
Head |
15 (10.5) |
|
Cause of injurya |
|
|
Jump from height |
21 (14.7) |
|
Hit by falling object |
43 (30.1) |
|
Fall |
35 (24.5) |
|
Other Unknown |
4 (2.8) 41 (28.7) |
|
aOne subject had 2 causes of injury: being hit by falling object and a fall. |
|
Physical functions
Table IV summarizes the results of MMT. Survivors with scores of 0–3 were classified as affected, and survivors with scores of 4–5 were graded as having normal muscle function. As shown in Table IV, the muscle functions of hip, knee and ankle were more severely affected compared with upper limbs. Some cases scored 0 in muscle contraction, indicating serious muscle dysfunction. Table V shows the AROM result for different joints. The ankle joint was the most seriously affected body part, with approximately 40% of patients unable to achieve full range of motion (ROM).
|
Table IV. Manual muscle testing (MMT) scores of survivors (n = 142; unknown = 1) |
||||||||
|
Body parts |
0 (zero) n (%) |
1 (trace) n (%) |
2 (poor) n (%) |
3 (fair) n (%) |
Affected Frequency (%) |
4 (good) Frequency (%) |
5 (normal) Frequency (%) |
Normal Frequency (%) |
|
Shoulder |
2 (1.4) |
0 (0.0) |
2 (1.4) |
3 (2.1) |
7 (5.9) |
10 (7.0) |
125 (88.0) |
135 (95.1) |
|
Elbow |
2 (1.4) |
0 (0.0) |
2 (1.4) |
3 (2.1) |
7 (5.9) |
15 (10.6) |
120 (84.5) |
135 (95.1) |
|
Wrist |
4 (2.8) |
1 (0.7) |
1 (0.7) |
4 (2.8) |
10 (7.0) |
9 (6.3) |
123 (86.6) |
132 (92.9) |
|
MCP |
3 (2.1) |
0 (0.0) |
1 (0.7) |
2 (1.4) |
6 (4.2) |
9 (6.3) |
127 (89.4) |
136 (95.8) |
|
PIP |
3 (2.1) |
1 (0.7) |
0 (0.0) |
2 (1.4) |
6 (4.2) |
9 (6.3) |
127 (89.4) |
136 (95.8) |
|
DIP |
3 (2.1) |
0 (0.0) |
0 (0.0) |
2 (1.4) |
5 (3.5) |
8 (5.6) |
129 (90.8) |
137 (96.5) |
|
Hip |
0 (0.0) |
1 (0.7) |
5 (3.5) |
14 (9.9) |
20 (14.1) |
38 (26.8) |
84 (59.2) |
122 (85.9) |
|
Knee |
0 (0.0) |
3 (2.1) |
4 (2.8) |
8 (5.6) |
15 (10.6) |
41 (28.9) |
86 (60.6) |
127 (89.4) |
|
Ankle |
2 (1.4) |
7 (4.9) |
9 (6.3) |
16 (11.3) |
34 (23.9) |
40 (28.2) |
68 (47.9) |
108 (76.1) |
|
MCP: Metacarpophalangeal joint; PIP: Proximal interphalangeal joint; DIP: Distal interphalangeal joint. |
||||||||
|
Table V. Active range of motion (ROM) of survivors |
|||
|
Body part |
No ROM n (%) |
Affected ROM n (%) |
Full ROM n (%) |
|
Shoulder |
2 (1.4) |
11 (7.7) |
130 (90.9) |
|
Elbow |
3 (2.1) |
10 (7.0) |
130 (90.9) |
|
Wrist |
8 (5.6) |
8 (5.6) |
127 (88.8) |
|
MCP |
3 (2.1) |
5 (3.5) |
135 (94.1) |
|
PIP |
3 (2.1) |
4 (2.1) |
136 (95.1) |
|
DIP |
3 (2.1) |
4 (2.1) |
136 (95.1) |
|
Hip |
2 (1.4) |
18 (12.6) |
123 (86.0) |
|
Knee |
4 (2.8) |
18 (12.6) |
121 (84.6) |
|
Ankle |
14 (9.8) |
44 (30.8) |
85 (59.4) |
|
MCP: Metacarpophalangeal joint; PIP: Proximal interphalangeal joint; DIP: Distal interphalangeal joint. |
|||
Functional and psychological assessments
The result of functional assessment using MBI is shown in Fig. 1. Seven patients were totally dependent in their ADL function, 23.1% were severely dependent, and 29.4% were moderately dependent. In total, 74.2% of victims had different degrees of dependence in their daily activities.
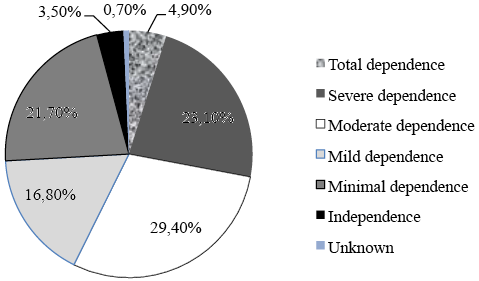
Fig. 1. Modified Barthel Index scores of survivors.
With regards to the psychological status of survivors, the PTSD-SS showed that more than half had various degrees of psychological symptoms. Moderate to severe PTSD symptoms were present in 26.6% of survivors (Fig. 2).
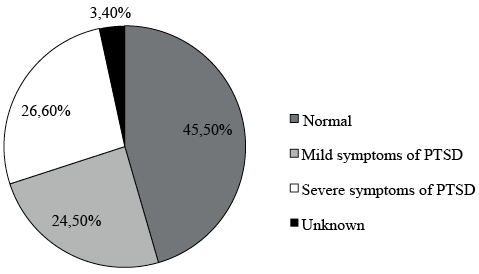
Fig. 2. Post-Traumatic Stress Disorder – Self Rating Scale (PTSD-SS) scores of survivors.
Treatments received and rehabilitation recommended by therapists
Most of the participating survivors had already received some form of rehabilitation during their hospitalization, including rehabilitation therapy (e.g. physiotherapy and occupational therapy), prosthesis and orthotics (P&O), and other forms of therapy. However, 10.5% had received no rehabilitation intervention from the hospital (Table VI).
|
Table VI. Treatments received during hospitalization |
|
|
Treatment |
n (%) |
|
Physiotherapy |
114 (79.7) |
|
Occupational therapy |
101 (70.6) |
|
Prosthesis and orthotics |
9 (6.3) |
|
No treatment received |
15 (10.5) |
|
A total of 96 patients received combined treatments of both occupational therapy and physiotherapy. |
|
Based on the physical, psychological and functional condition of the survivors, together with available resources and the environmental barriers the survivors encountered, further rehabilitation needs were identified and recommended by experienced therapists with the goal of providing a more in-depth, all-round and comprehensive programme. As shown in Table VII, many patients still needed rehabilitation services such as splints (44.8%), walking aids (46.9%), exercise therapy (49%) and functional training (74.8%). Psychological support, such as counselling (52.4%), emotional control training (25.2%) and stress management (35.7%), was suggested for those patients in need. Moreover, home and community modifications (45.5% and 40.6%, respectively) were recommended according to the physical needs and environmental restrictions of the patients.
|
Table VII. Rehabilitation needs identified by therapists |
||
|
Yes n (%) |
No n (%) |
|
|
Physical and functional needs |
||
|
Splints |
64 (44.8) |
79 (55.2) |
|
Pressure garment |
13 (9.1) |
130 (90.9) |
|
Bandage |
13 (9.1) |
130 (90.9) |
|
Walking aids |
67 (46.9) |
76 (53.1) |
|
Prosthesis |
5 (3.5) |
138 (93.50 |
|
Wheelchair use |
43 (30.1) |
100 (69.9) |
|
Aids |
42 (29.4) |
101 (70.6) |
|
Exercise therapy |
70 (49.0) |
73 (51.0) |
|
Electronic therapy |
18 (12.6) |
125 (87.4) |
|
Functional training |
107 (74.8) |
36 (25.2) |
|
Acupuncture |
3 (2.1) |
140 (97.9) |
|
Tui Na |
4 (2.8) |
139 (97.2) |
|
Other physical needs |
4 (2.8) |
139 (97.2) |
|
Psychological needs |
||
|
Counselling |
75 (52.4) |
68 (47.6) |
|
Support group |
24 (16.8) |
119 (83.2) |
|
Emotional control training |
36 (25.2) |
107 (74.8) |
|
Stress management |
51 (35.7) |
92 (64.3) |
|
Other psychosocial stress |
1 (0.7) |
142 (99.3) |
|
Community needs |
||
|
Home modification |
65 (45.5) |
78 (54.5) |
|
Community resource |
71 (49.7) |
72 (50.3) |
|
Community modification |
58 (40.6) |
85 (59.4) |
|
Follow-up |
96 (67.1) |
47 (32.9) |
|
Other community needs |
1 (0.7) |
142 (99.3) |
DISCUSSION
Medical rehabilitation is one of the essential emergency services in disasters and it is not restricted to intermediate and long-term care settings (18). In most developing countries, rehabilitation is often confined to the implementation of physical modalities and passive mobilization to relieve pain and minimize physical impairment. The rehabilitation programme is usually delivered after surgery or other medical treatments when patients have residual pain, limited ROM or muscle weakness. However, some patients may have also developed joint contracture and other complications. In major disasters, the main focus is on survival and rescuing injured victims, with inadequate assessment of rehabilitation needs and inadequate rehabilitation services in the early stage, particularly in developing countries where the rehabilitation concept has not yet been developed. This aim of this study was to determine the rehabilitation needs of injured victims after a major earthquake soon after their admission to hospital, and to determine their future rehabilitation needs.
In this study, 143 injured cases were recruited after a major earthquake in 3 large regional hospitals. The physical and psychosocial functioning of subjects were measured using standardized assessment tools within 3 months of injury. Demographic data was collected through a review of case records and interviews. Subjects’ living environments and environmental barriers were also surveyed in preparation for their discharge. It was evident that there were strong needs for hospital-based rehabilitation as well as community rehabilitation programmes. A previous study has assessed the rehabilitation needs of patients with spinal cord injury in the Haiti earthquake (11). This study has extended the sampled subjects to other types of disabilities.
The demographic data of the patients in this study showed that the majority of victims were adults in their 40s, with more males than females. This is similar to the data reported in 2008 Wenchuan earthquake (19). Disasters have been frequently occurring in low-resourced regions where disaster response plans do not include strategies for physical rehabilitation or specifically account for persons with new or pre-existing disabilities (1).
The most common injuries caused by earthquakes include fractures, limb amputations, spinal cord injuries, traumatic brain injury, soft tissue injuries, etc., with lower extremities being the most frequently traumatized areas (20). Lower limb fracture was found to be the most common type of injury. Due to the occurrence of multiple injuries, the incidence rate of fractures appeared to be higher among subjects in this study. For example, it was reported that more than 50% of the victims in the Bam earthquake had fractures (21), and the incidence of fractures among the patients treated in 14 hospitals after the Wenchuan earthquake was almost half of the total number of injuries (1,011 out of 2,148 patients) (22).
Physical assessments indicated that hip, knee and ankle had relatively poor performance in ROM and muscle strength. The knees and ankles were comparatively more severely affected. This was because lower limb fracture was the most common injury among the victims surveyed in this study, which often caused limitation of movements of the knees and ankles (3). Considering the high incidence of fractures and lower limb injuries, it is understandable that splints, walking aids, exercise programmes and wheelchairs would be needed for patients to improve their functional independence, as shown in Table VII. As shown in Fig. 1, the majority of patients were mildly to totally dependent in daily functional skills, suggesting that most of the earthquake survivors had decreased functional level and ADL. A previous study assessed the functional status of the patients with fractures sustained in the Wenchuan earthquake and found that more than two-thirds had reduced daily activities (3). There appeared to be a strong demand for functional training.
Although most patients received some form of rehabilitation during their hospitalization soon after acute medical treatment, in some hospitals, the variety and types of rehabilitation services were reported to be inadequate. Since the Wenchuan earthquake in 2008, we have witnessed significant improvement in rehabilitation services in China. However, the concept of early rehabilitation in hospitals remains unclear and is not practiced, resulting in complications arising before cases are transferred to the rehabilitation department. Through identifying the rehabilitation needs of Ya’an earthquake victims in this study, early rehabilitation intervention as well as continued rehabilitation management in the community was found to be essential. Medical intervention should be provided to victims as early as possible, including acute hospital care, immediate medical support, and traditional medicine intervention. Meanwhile, professional rehabilitation services, such as occupational therapy, physical therapy and psychological support, should also be provided to the survivors as early as possible, in order greatly to enhance their recovery outcomes.
The earthquake-affected area in this study is a mountainous region, where people have relatively low incomes compared with city-dwellers. As revealed by the survey, the majority of the earthquake victims were farmers (40.6%) with a low level of education (total 68.6% with primary or secondary school education). The local government did not include strategies for physical or community rehabilitation in the disaster response plans. There were patients with external fixtures on their injured limbs who were discharged home with no follow-up services. As many of the survivors lived in mountainous villages, community rehabilitation, including home visits, environmental modifications, and community adjustments, were important for them to achieve full recovery and re-integration into the community.
This study reflects the need for comprehensive hospital- and community-based rehabilitation services for earthquake survivors; such needs are usually not met in developing countries. As shown in Table II, investigation of the patients’ living environments revealed that most lived in relatively poor environments where access for people with disabilities remains inadequate, such as poor toileting and bathing facilities, reflecting the importance of community rehabilitation. Customized home or community modifications (such as modifications of home facilities and removal of stairs, slopes, etc.) together with a continuing community rehabilitation programme should be administered to enhance the patients’ recovery outcomes. A long-term community follow-up rehabilitation programme should also be provided to ensure good community training and support for the patients.
Psychological assessment revealed that approximately 51% of the surveyed earthquake survivors reported symptoms of PTSD, with 26.6% in a moderate to severe status (Fig. 2). A previous study of survivors conducted 18 months after the Pakistan earthquake showed that 46.6% still had PTSD (23). Young people seemed to be able to cope better with the psychological stress. Studies of the 2008 Wenchuan earthquake victims showed that 15.8% of the adolescents had PTSD 6 months after the earthquake (24), and victims who lived in heavily damaged areas (47.3%) were more likely to sustain PTSD than those living in moderately damaged areas (10.4%) (25). In our study, although we found no relationship between the severity of injuries and the incidence of PTSD, patients’ reports of PTSD symptoms were alarming. The effectiveness of psychological intervention for PTSD was confirmed in a recent study among Sichuan earthquake fracture victims (26). In our survey, psychosocial intervention had not yet been developed and integrated into the rehabilitation programme at the hospitals. Counselling, support groups, emotional and stress management should be considered as part of the rehabilitation programme. The high level of incidence of jumping (around 15%) shown in the current study further supported these aspects of rehabilitation. With the Wenchuan earthquake occurring only 5 years previously, many survivors were still affected by anxiety; thus, when another earthquake occurred, they were so afraid of dying that they chose to jump from a height instead of remaining inside the building. Taking this factor into account, together with demographic and environmental information, psychosocial rehabilitation is strongly recommended for these earthquake survivors and their families.
Study limitations
The current study had a few limitations. Firstly, although the rehabilitation needs of the patients were assessed by experienced therapists, due to limited resources and funds provided by the government, whether and how they received the corresponding services after discharge into the community or society was not investigated in this study. Despite the experiences from the Wenchuan earthquake and other disasters, the final success of rehabilitation still relied on many factors (27). Further research into the effectiveness of the community rehabilitation services programme is required. Furthermore, it should be noted that some data were missing, especially for those self-rating items or those related to personal information. Despite the strong need for evidence-based research on disaster rehabilitation, it is recommended that the burden on survivors should be taken into account when conducting assessments. The primary goal of assessment of rehabilitation needs is to collect data to support the care and needs of the survivors, and this should not be demanding for disaster victims (18).
Conclusion
This study assessed the physical, functional and psychosocial status of 143 survivors from the 420 Ya’an earthquake who were admitted to hospital, and surveyed their living environment. Although the scope of injuries was less severe than in the 512 Wenchuan earthquake in 2008, a significant number of survivors had residual physical and psychosocial disabilities. The results reflect the needs of patients for early physical rehabilitation and psychosocial intervention as well as functional training. In addition, due to their poor living environment, home or community modification is essential for these patients to achieve better recovery and re-integrate into society.
ACKNOWLEDGEMENTS
The authors are grateful for the support of the senior administration team of the 3 hospitals, including West China Hospital, Chengdu No. 2 Hospital and Bayi Hospital, where the research was conducted. The authors would also like to thank all the patients, therapists and doctors who participated in the study. This research was supported by donations from the Hong Kong Jockey Club.
REFERENCES
