Ling Li, MD1,2,3*, Jan D. Reinhardt, PhD4,5,6,7*, Xia Zhang, MD, PhD1,3,5, Andrew Pennycott, PhD8, Zhengen Zhao, MD9, Zeng Xianmin, MD10 and Jianan Li, MD1,5
From the 1Department of Physical and Rehabilitation Medicine, First Affiliated Hospital of Nanjing Medical University, Nanjing, 2Department of Physical and Rehabilitation Medicine, Xuzhou Central Hospital, Xuzhou, 3Caring For Children Foundation, Hong Kong, 4Institute for Disaster Management and Reconstruction, Medical Faculties of Sichuan University Chengdu, and Hong Kong Polytechnical University, Hong Kong, China, 5Committee for Rehabilitation Disaster Relief of the International Society of Physical and Rehabilitation Medicine, Geneva, 6Swiss Paraplegic Research, Nottwil, Switzerland, 7Department of Health Sciences and Health Policy, University of Lucerne, Lucerne, 8Sensory-Motor Systems Laboratory, Department Health Sciences and Technology, ETH Zurich, Switzerland, 9Rehabilitation Medicine, Mianzhu County People’s Hospital, Mianzhu and 10Rehabilitation Medicine, Shifang County People’s Hospital, Shifang, China. *These authors contributed equally.
OBJECTIVES: To examine the development and determinants of long-term outcomes for earthquake victims with amputations, including physical function, pain, quality of life and life satisfaction.
DESIGN: Prospective cohort study with 2–3 measurement points.
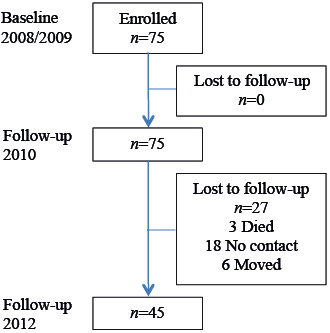
SUBJECTS: A total of 72 people who underwent amputations following the 2008 Sichuan Earthquake and resided in Mianzhu County, Sichuan Province, China were enrolled in the study. Of these, 27 people were lost to follow-up.
METHODS: Data on pain (visual analogue scale) and physical function (Barthel Index) were collected at 3 measurement points (2009, 2010 and 2012), and data on quality of life (Medical Outcomes Short-Form 36) and life satisfaction (Life Satisfaction Questionnaire-11) were collected at 2 measurement points (2010 and 2012). Data were analysed with mixed effects regression.
RESULTS: Pain severity declined significantly and physical function increased by 2012. Quality of life and life satisfaction remained relatively stable between 2010 and 2012, while quality of life was significantly lower than reference values from the general population. Illiteracy and lower extremity amputations were associated with lower quality of life and life satisfaction in several domains.
CONCLUSION: While amputees’ functioning and pain were improved over time, quality of life and life satisfaction did not change. Illiterate earthquake survivors and those with lower extremity amputations are at particular risk of low quality of life and life satisfaction, and may require additional attention in future earthquake rehabilitation programs.
Key words: amputation; natural disaster; earthquake; physical function; pain; quality of life; mental health; physical health; life satisfaction; rehabilitation.
J Rehabil Med 2015; 47: 00–00
Correspondence address: Jianan Li, Department of Rehabilitation Medicine, The First Affiliated Hospital of Nanjing Medical University, No. 300 Guangzhou Road, Nanjing, 210029, China. E-mail: lijianan@carm.org.cn
Accepted Dec 10, 2014; Epub ahead of print Mar 6, 2015
INTRODUCTION
The 2008 Sichuan Earthquake reached a level of 8.0 on the Richter scale and affected more than 45 million people. A total of 87,476 people died and 374,643 were injured as a result of this catastrophic event (1). In Mianzhu County alone, one of the most severely affected regions, an area of 1,245 km2 was destroyed and 5 million people were affected in total. A rehabilitation services model comprising institutional as well as community-based components was set up in Mianzhu County in order to meet the victims’ rehabilitation needs (1).
Amputations are a common medical intervention following a major earthquake (2) and have featured prominently following earthquakes in Marmara, Turkey (3), Kashmir (4), Haiti (5) and in the 2008 Sichuan earthquake (6) discussed in this paper. Amputation is a severely disabling condition that imposes a variety of physical and psychological challenges including alterations in lifestyle, changes in self-concept, decreased quality of life (QoL), impairments in physical functioning, and sensory effects such as phantom pain, phantom sensation and stump pain (7, 8).
Although survivors’ quality of life post-earthquake has been studied previously in specific groups, such as children (9) and those who suffered from spinal cord injury, after such an event (10), QoL and life satisfaction (LS) of amputees from the Sichuan earthquake have not yet been investigated in detail. Moreover, although previous research has analysed the determinants of outcomes such as QoL, mobility and activities of daily (ADL) living for groups including spinal cord injured patients and fracture victims (1, 11, 12), little is yet known concerning the determinants of these outcomes in earthquake victims with amputations. Knowledge concerning these determinants is, nevertheless, important for identifying vulnerable groups and entry points for interventions.
This study aims to examine the development and determinants of long-term outcomes of earthquake victims with amputations, including physical function, pain, QoL and LS.
METHODS
Design
A prospective cohort study with 2–3 measurement points.
Participants
Seventy-two patients with amputations residing in Mianzhu County, Sichuan Province, China admitted for rehabilitation at Mianzhu County Hospital were enrolled in this study. Twenty-seven patients were lost to follow-up (37.5%): 3 patients died and attempts to contact a further 24 patients were unsuccessful. A total of 45 patients (62.5%) completed all the assessments (see Fig. 1).
Inclusion criteria were: (i) having an amputation caused by the earthquake without the presence of a co-existing injury to the central nervous system (traumatic brain injury or spinal cord injury) or internal organs; (ii) having sufficient cognitive function and comprehension of Mandarin to answer the questionnaires accurately; (iii) having received therapy in the rehabilitation centre for earthquake survivors in Mianzhu.
This research was approved by the ethics committee of Nanjing Medical University. Informed consent was obtained from all participants.
Interventions
Institution-based rehabilitation of earthquake victims who underwent amputations in Mianzhu County involved measures to prevent joint contracture, desensitization, shaping of the residual limbs, joint mobilization, muscle strength training, physical therapy, occupational therapy and psychotherapy.
Measures
Physical function, pain, QoL and LS were assessed in this investigation. Physical function and pain were assessed before admission to rehabilitation and at 2 follow-up occasions. QoL and life satisfaction were measured at follow-up only.
Physical function was measured with the Barthel Index (BI) (13, 14), which is a general 10-item measure of independence in activities of daily living. The index varies between 0 and 100 points, with higher scores indicating greater levels of independence. The visual analogue scale (VAS) (15) was used to assess the degree of chronic pain. The scale ranges from 0 (no pain) to 10 (worst pain).
QoL was measured by the Medical Outcomes Study Short-Form 36 (SF-36) (16). The SF-36 comprises 36 categories, 35 of which are grouped into 8 multi-item scales: physical functioning (PF, 10 items), role physical (RP, 4 items), bodily pain (BP, 2 items), general health (GH, 5 items), vitality (VT, 4 items), social functioning (SF, 2 items), role emotional (RE, 3 items) and mental health (MH, 5 items). The remaining item concerns the experience of change in general health during the previous year. The scores for the 8 scales range from 0 (worst QoL) to 100 (best QoL).
Life satisfaction was measured via the Life Satisfaction Questionnaire-11 (LiSat-11) (17). This is an extension of LiSat-9 comprising patients’ assessments regarding overall satisfaction with life in addition to satisfaction in 10 domains: vocation, economy, leisure, contacts, sexual life, activities of daily living, family life, relationships with partners, somatic health and psychological health. The responses were made on a 6-point Likert scale (18): 1 = very dissatisfied, 2 = dissatisfied, 3 = rather dissatisfied, 4 = rather satisfied, 5 = satisfied, 6 = very satisfied.
Validated Chinese versions of the BI (19), VAS (20), SF-36 (21) and LiSat-11 (22) were used to assess physical function, pain, QoL and LS, respectively.
Independent variables included demographic information on gender, marital status, educational level, employment status and annual family income, as well as the level of amputation (hand, elbow, foot or knee).
Procedure
The research team received lists of amputees from local government and Mianzhu County Hospital. The patients were then contacted by telephone to arrange face-to-face interviews.
Outcomes were collected in August 2010 and July 2012 by trained rehabilitation volunteers who had at least 2 years clinical experience. Additional data for BI and VAS from a baseline evaluation in 2009 before the start of institutional rehabilitation were available, but corresponding SF-36 and LiSat-11 data from 2009 were not. Data were entered separately by 2 coders who then cross-checked their results.
Statistical analysis
All computations were made with Stata 12. Descriptive statistics and a comparison of unadjusted scores were provided for outcomes between the time-points (for complete cases only) as well as a comparison between SF-36 scores of the study population and reference values from the general population of Sichuan Province (23). Friedman tests and Bonferroni corrected Wilcoxon signed-rank post-hoc tests were used for comparison of unadjusted VAS and BI scores between time-points. Wilcoxon signed-rank tests were used for comparison of unadjusted SF-36 scores between time-points and with the general population reference values (tested against general population against medians).
Potential determinants of the outcomes were analysed via mixed effect models in order to account for unobserved heterogeneity due to clustering of the measurements by subject. This type of model requires data in long format, in which the cases are measurement points rather than subjects. This allows the outcome to be modelled as a dependent variable at different time-points (24). To account for a known ceiling effect of the BI and ceiling and floor effects of the VAS, a longitudinal Tobit model was computed for BI and VAS, as demonstrated and recommended by Twisk & Rijmen (25) in addition to Zhang et al. (1). This type of model estimates a latent variable that can assume values above and below the scale’s ceiling and floor, respectively. Linear mixed models introducing random intercepts for the subjects were used for all the other outcomes. The model structure allows the inclusion of respondents with missing data. It has been assumed that data were missing at random, such that the probability of missing outcome data at one measurement may be dependent on the measured independent variables or outcomes at previous occasions, but not on the unobserved value of the missing outcome.
All models included the following 8 predictors: gender (reference: female), age, educational level (reference: literate), marital status (reference: unmarried), income (reference: middle to high income), unemployment (reference: employed, in education or retired), type of amputation (reference: lower extremity), and time-point (reference: 2009/baseline for BI and VAS, 2010 for all other outcomes). In the cases of BI and VAS, contrasts were employed to determine whether significant changes had occurred between 2010 and 2012. In order to account for multiple testing, all p-values were Bonferroni-corrected.
RESULTS
Data on demographics and amputation levels of the study population are provided in Table I.
|
Table I. Demographics and injury characteristics of the study population |
|||
|
Variables |
Complete cases n (%) |
Dropouts n (%) |
p-value of χ2/t-tests |
|
Age |
|||
|
< 20 years |
10 (22.22) |
3 (11.11) |
|
|
20–34 years |
4 (8.89) |
2 (7.41) |
|
|
35–49 years |
16 (35.56) |
3 (11.11) |
|
|
50–64 years |
12 (26.67) |
7 (25.93) |
|
|
≥ 65 |
3 (6.67) |
12 (44.44) |
|
|
Mean+SD |
45 (43.5+18.36) |
27 (58.11+22.88) |
< 0.001 |
|
Gender |
0.951 |
||
|
Male |
22 (48.89) |
13 (48.15) |
|
|
Female |
23 (51.11) |
14 (51.85) |
|
|
Marital status (%) |
0.360 |
||
|
Married |
29 (64.44) |
17 (62.96) |
|
|
Single |
12 (26.67) |
5 (18.52) |
|
|
Divorced |
1 (2.22) |
0 (0) |
|
|
Widowed |
3 (6.67) |
5 (18.52) |
|
|
Education |
0.031 |
||
|
Illiterate |
12 (26.67) |
14 (51.85) |
|
|
Literate |
33 (73.33) |
13 (48.15) |
|
|
Employment |
0.017 |
||
|
Back to work |
7 (15.56) |
3 (11.11) |
|
|
New job |
2 (4.44) |
1 (3.70) |
|
|
At school |
6 (13.33) |
3 (11.11) |
|
|
Retired |
8 (17.78) |
15 (55.56) |
|
|
Unemployed |
22 (48.89) |
5 (18.52) |
|
|
Annual family income |
0.106 |
||
|
< mean level |
33 (73.33) |
25 (95.59) |
|
|
= mean level |
4 (8.89) |
0 (0) |
|
|
> mean level |
8 (17.78) |
2 (7.41) |
|
|
Type of amputation |
0.141 |
||
|
Hand |
5 (11.11) |
6 (22.22) |
|
|
Below-elbow |
1 (2.22) |
3 (11.11) |
|
|
Above-elbow |
3 (6.67) |
1 (3.70) |
|
|
Foot |
3 (6.67) |
4 (14.81) |
|
|
Below-knee |
22 (48.89) |
6 (22.22) |
|
|
Above-knee |
11 (24.44) |
7 (25.93) |
|
|
SD: standard deviation. |
|||
Most patients were between 35 and 64 years old and married. The male-female distribution was almost even. More than one-third of the study population was illiterate, in contrast to the 12.04% rate in the Sichuan general population (26). Most patients were retired or unemployed and the vast majority of the victims had an income under the Sichuan average. The most frequent amputations were below the knee. Dropouts significantly differed from complete cases in age, employment status and education. More than half of the dropouts were illiterate.
Fig. 2 shows the unadjusted medians and interquartile range (IQRs) of the BI and VAS. BI scores significantly increased from a median of 85 (IQR 75–95) in 2009 to 100 (IQR 95–100) in 2012 (Friedman = 66.2, p = 0.016) and VAS scores significantly decreased from a median of 4 (IQR 2–6) in 2009 to 3 (IQR 0–5) in 2010 and 2 (IQR 0–3) in 2012 (Friedman = 97.07, p < 0.001). However, no significant improvement in BI took place between 2010 and 2012 (p = 0.063), while changes in VAS were significant between all time-points according to Bonferroni-corrected Wilcoxon signed-rank post-hoc tests.
In 2009, 60 persons (83.3%) reported experiencing pain. At the study end-point, 27 persons (60%) reported the presence of pain, of whom 22 (81%) had residual limb pain and 4 had phantom limb pain (15%). One subject reported both residual and phantom pain.
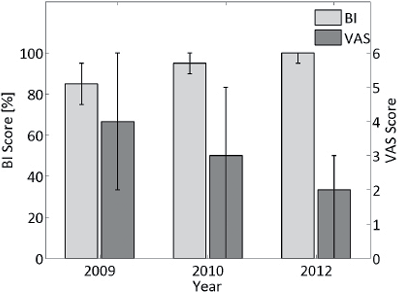
Table II shows the determinants of physical function and pain severity. In addition to the time-point (the year 2010 and 2012 vs baseline), age is a significant determinant of physical function and pain severity, decreasing the former outcome and increasing the latter. In accordance with the unadjusted results, BI scores were significantly increased, whereas VAS scores significantly decreased between baseline and follow-up in the fully adjusted Tobit models. Bonferroni-corrected post-hoc tests showed that, while no significant improvement in BI took place between 2010 and 2012, improvement in VAS was significant during this period.
|
Table II. Significant determinants of Barthel Index (BI) and visual analogue scale (VAS) from multivariate longitudinal Tobit regressions |
|||||
|
Dependent variables |
Independent variables |
||||
|
Variables |
Coefficient |
Standard error |
Beta |
p-value |
|
|
BI |
Age |
–0.233 |
0.101 |
–2.31 |
0.021 |
|
Year 2010 |
13.007 |
1.866 |
6.97 |
> 0.001 |
|
|
Year 2012 |
21.589 |
2.636 |
8.19 |
> 0.001 |
|
|
VAS |
Age |
0.049 |
0.019 |
2.61 |
0.009 |
|
Year 2010 |
–1.202 |
0.287 |
–4.19 |
> 0.001 |
|
|
Year 2012 |
–2.691 |
0.359 |
–7.49 |
> 0.001 |
|
Unadjusted QoL scores, assessed via the SF-36, are shown in Fig. 3. No significant change in any of the SF-36 scales took place between 2010 and 2012. Only the change in the role physical score between 2010 and 2012 is close to reaching significance (2010 median and IQR: 31.25, 25–62.5; 2012 median and IQR: 56.25, 37.5–75, p = 0.057). Scores in all SF-36 domains were significantly lower than those of the general population.
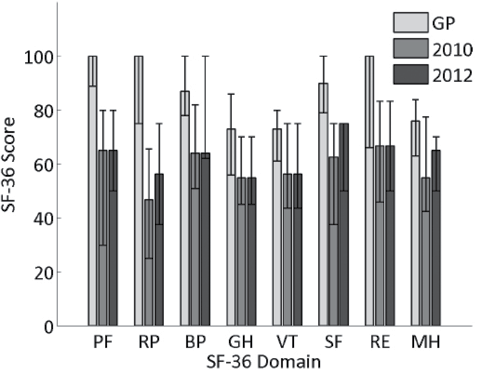
Fig. 3. Medians and interquartile ranges of Medical Outcomes Short-Form 36 (SF-36) subscales across time-points and compared with the general population (GP). PF: Physical Function; RP: Role Physical; BP: Bodily Pain; GH: General Health; VT: Vitality; SF: Social Function; RE: Role Emotional; MH: Mental Health.
Table III shows the significant determinants of the different QoL and LS sub-scales. Physical function decreases with increasing age and is greater in married persons and those with upper extremity amputations. Furthermore, males reported better QoL concerning bodily pain. A trend for greater pain with increased age is evident (the factor just missed the level of significance with p = 0.06). Higher rates of literacy are associated with better physical health (as reflected by the SF-36 physical function and role-physical scores) and mental health status (shown in the SF-36 social functioning, role-emotional and mental health results). Moreover, literacy is predictive of higher satisfaction with self-care and ADL. Patients with upper extremity amputations show higher SF-36 scores related to physical function and mental health than those with lower extremity amputations and are also more satisfied with leisure activities. Higher age is associated with decreased satisfaction with leisure activities and relationships, while being male is associated with higher satisfaction with somatic health. Married persons reported higher satisfaction with ADL and sexual life, and the lower income group were less satisfied with their economic situation.
|
Table III. Significant determinants of Medical Outcomes Short-Form 36 (SF-36) and Life Satisfaction Questionnaire 11 (LiSat-11) from multivariate linear mixed effects regressions |
|||||
|
Dependent variables |
Independent variables |
||||
|
Variables |
Coefficient |
Standard error |
Beta |
p-value |
|
|
SF-36 |
|||||
|
Physical function |
Age |
–0.455 |
0.148 |
–3.07 |
0.002 |
|
Married |
13.255 |
6.098 |
2.17 |
0.030 |
|
|
Illiterate |
–15.120 |
5.989 |
–2.52 |
0.012 |
|
|
Upper extremity |
17.028 |
5.538 |
3.07 |
0.002 |
|
|
Role-physical |
Illiterate |
–11.004 |
5.571 |
–1.98 |
0.048 |
|
Bodily pain |
Male |
11.140 |
5.344 |
2.08 |
0.037 |
|
Social functioning |
Illiterate |
–12.939 |
6.222 |
–2.08 |
0.038 |
|
Role-emotional |
Illiterate |
–15.367 |
6.139 |
–2.50 |
0.012 |
|
Mental health |
Illiterate |
–11.191 |
4.820 |
–2.32 |
0.020 |
|
Upper extremity |
12.598 |
4.455 |
2.83 |
0.005 |
|
|
LiSat-11 |
|||||
|
Somatic health |
Male |
0.564 |
0.256 |
2.21 |
0.027 |
|
ADL |
Married |
0.672 |
0.262 |
2.56 |
0.010 |
|
Illiterate |
–0.926 |
0.255 |
–3.63 |
0.000 |
|
|
Leisure |
Age |
–0.019 |
0.007 |
–2.62 |
0.009 |
|
Upper extremity |
0.542 |
0.263 |
2.06 |
0.040 |
|
|
Economy |
Low income |
–0.709 |
0.278 |
–2.55 |
0.011 |
|
Sexual life |
Married |
2.687 |
1.050 |
2.56 |
0.011 |
|
Partner relationship |
Age |
–0.023 |
0.012 |
–1.97 |
0.049 |
DISCUSSION
Using data from several time-points, physical functioning, social functioning, QoL and LS outcomes for earthquake victims with amputations have been examined. The results highlight improvements in functional independence and a reduction in pain severity during the post-earthquake period. These findings are in contrast with results from a study of 199 amputees from the 2010 Haiti earthquake demonstrating significant decrease in satisfaction with functional status and increased presence of pain during a 2-year period after the earthquake (27). As sample compositions are comparable in terms of levels of amputation and demographics, those differences may be either due to distinct rehabilitation treatment approaches or environmental factors, such as housing conditions and supports (27). The levels of functional independence and pain were higher and lower, respectively, compared with victims with spinal cord injuries from the 2008 Sichuan earthquake (11, 28). However, in spite of improved functional status and pain, significant improvements in QoL and LS scores were not apparent in the period between 2010 and 2012. Furthermore, patients’ QoL at the study end-point was lower than that of the general population across all SF-36 domains. As expected, age was associated with lower levels of physical functioning in this study, in agreement with other research (29).
The results of this study highlight that education and the amputation site play major roles in the QoL and LS of amputees. Illiterate victims usually have less knowledge concerning how to avoid injury during an earthquake and may also be slow in adjusting to the impairment and accepting the new lifestyle imposed by an amputation. Moreover, patients with better education could have more advanced skills with regard to self-management and mobilization of support, higher chances of finding employment and better coping strategies (30). Higher levels of education have also been shown to be associated with higher QoL (31). In addition, an inverse relationship between educational level and post-traumatic morbidity has been previously noted (32). Increased risks of depression (33) and post-traumatic stress (34) at lower educational levels have also been highlighted.
The finding of this study, that patients with upper limb amputations (as opposed to lower extremity amputations, which are thought to be given priority over upper extremity amputations following other earthquakes (35)) report better QoL and LS, corroborates an earlier study of a population of 539 people with a major limb amputation using a sex and age adjusted model (36). Physical mobility is a strong predictor of QoL after amputations (37). Difficulties in returning to normal levels of ambulation (potentially related to inaccessible environments) may restrict participation in different activities (38), thus potentially adversely impacting QoL to a greater extent than upper extremity amputations.
Future rehabilitation measures after earthquakes could pay additional attention to illiterate amputees and those with lower extremity amputations. It is suggested that language-independent educational modules are developed and more attention paid to ease of ambulation in home environments and communities.
There are various limitations pertaining to this study that potentially limit the ability to generalize its findings. Of particular importance are the small sample size and the fact that the participants were included only from the Mianzhu region of the earthquake zone. Nevertheless, this region is fairly representative, since it includes both urban and rural areas, and the amputation levels and injury severity in this study are comparable to other epidemiological investigations from the Sichuan (39) and Haiti (27) earthquakes. Another limitation is lack of the baseline data regarding QoL and LS, such that potential improvement due to institutional rehabilitation could not be determined. Non-response at follow-up was an additional problem, particularly in older and illiterate patients. Therefore, there may have been some degree of selection bias. For example, patients with worse outcomes may have been more likely to drop out.
Illiterate earthquake survivors and those with lower extremity amputations are at particular risk of low QoL and LS, and may require additional attention in future earthquake rehabilitation programs.
ACKNOWLEDGEMENTS
The authors acknowledge the support of the Hong Kong Caring for Children Foundation, the Chinese Association of Rehabilitation Medicine, the Nanjing Medical University, Handicap International, Sichuan Province and Mianzhu County Government, Mianzhu County People’s Hospital, and the Hong Kong Rehabilitation Society. The authors would like to thank all earthquake victims who participated in this study and the rehabilitation volunteers who helped to collect the data.
The authors declare no conflicts of interest.
REFERENCES
