Mariusz Drużbicki, PhD1,2, Agnieszka Guzik, PhD1, Grzegorz Przysada, MD1,2, Andrzej Kwolek, MD1 and Agnieszka Brzozowska-Magoń1
From the 1Institute of Physiotherapy, University of Rzeszów and 2Clinical Rehabilitation Unit of the Regional Hospital No. 2, Rzeszów, Poland
OBJECTIVES: To evaluate the effects of gait training using a treadmill with and without visual biofeedback in patients in the late period after stroke, and to compare both training methods.
DESIGN: A randomized, controlled study.
SUBJECTS: Fifty people at least 6 months after stroke, randomly enrolled into groups with a rehabilitation programme of treadmill training with or without visual biofeedback.
METHODS: Spatio-temporal gait parameters, walking speed, walking distance, self-reliant mobility and functional capacity were evaluated during a programme of 10 sessions over 2 weeks.
RESULTS: Patients in both groups achieved statistically significant improvement. Participants in the intervention group revealed a significantly greater improvement in the shortening of the stance phase (p = 0.0045) and lengthening of the swing phase of the unaffected limb (p = 0.0042) and an increase in the unaffected limb cycle length (p = 0.0021). There were no significant differences between groups in other spatio-temporal parameters of gait or additionally assessed parameters.
CONCLUSION: Gait training using a treadmill resulted in improvements in the gait and functional capacity of patients. The use of biofeedback gives better results in improving gait cycle length, duration of gait phases and swing phase speed compared with exercise on a treadmill alone.
Key words: stroke; gait; rehabilitation; visual biofeedback.
J Rehabil Med 2015; 47: 00–00
Correspondence address: Mariusz Drużbicki, Institute of Physiotherapy, University of Rzeszów, ul. Warszawska 26 a, 35-205 Rzeszów, Poland. E-mail: mdruzb@univ.rzeszow.pl
Accepted Dec 10, 2014; Epub ahead of print Mar 6, 2015
INTRODUCTION
Patients with post-stroke hemiparesis develop a pathological gait pattern of residual selective movement control, spasticity and preserved pathological muscle reactions. Hemiparetic gait is characterized by a series of disturbances, including significant asymmetry of the duration of the gait phases, step length and lower limbs loading, demonstrated by overloading of the non-paretic limb. This results in a reduction in walking speed, which reduces efficiency and increases energy expenditure. Therefore, one of the most important needs in the rehabilitation of patients with hemiparesis after stroke is to recover gait function (1–4).
Recovering or acquiring new, compensating, motor skills lost after brain injury occurs during the motor learning process, which is supported by plasticity of other parts of the brain. Activation of the central nervous system allows the plastic adaptation of the neuromuscular system and is essential for recovery of normal functioning. To increase their effectiveness of action, new or existing physiotherapy strategies must take into account and apply the rules governing plasticity (5–7). In a systematic review Polese et al (8) found that treadmill training without body weight support allows for a greater increase in gait speed and walking distance than training without a treadmill. The effects were lasting and achievable for patients in the early and late period after stroke (8). Based on a review of 44 published studies involving 2,658 patients after stroke, Mehrholz stated that the use of a treadmill with or without partial body weight relief for gait learning does not increase the probability of recovery of independent gait, compared with training without a treadmill. He also stated that treadmill training significantly increases the speed and distance of gait in patients with independent gait, and that the achieved results were lasting (9). Introduction of additional visual and proprioceptive feedback to treadmill training improves walking speed and symmetry of the spatio-temporal parameters of gait in patients in the late period after stroke. However, further studies are needed to determine the actual impact of biofeedback on the therapy outcome (10). Biofeedback methods are used to replace impaired sensory information essential for proper analysis and planning of motion. They rely on the delivery of visual, auditory and proprioceptive information to the central nervous system (11, 12). Exercises on a treadmill with the use of biofeedback are one of the ways to improve locomotive ability. This improves gait parameters and produces good results during the early and late periods after stroke. The introduction of additional external auditory and visual information about proper gait pattern and its parameters, i.e. speed, step length and gait phase symmetry, to gait training on a treadmill allows the patient to not only improve symmetry of gait, but also balance, coordination and strength, as well as endurance of the relevant muscle groups (13–16). However, few research trials were conducted in randomized groups of patients after stroke (17).
This study aims to evaluate and to compare the effects of gait training using a treadmill with and without biofeedback in gait training in patients in the late period after stroke.
MATERIALS AND METHODS
Design
This study was a single-blind, randomized, control group investigation, conducted among patients treated at the Clinical Rehabilitation Unit with the Subunit of Early Neurolological Rehabilitation of the Regional Hospital No. 2 in Rzeszów, Poland. All qualified patients were fully informed about the study and signed informed consent prior to joining the programme. Prior to patient recruitment the study protocol was approved by the ethics committee of the Faculty of Medicine at the University of Rzeszów, Poland (number 5/11/2009) and National Science Centre, Poland (number N N404 249639).
Patients
The study included 50 patients in the late period after cerebral stroke (18 females, 32 males; mean age 62 years (range 38–79 years)). Inclusion criteria were: ischaemic stroke, time from stroke at least 6 months, time from the completion of the last treatment in the rehabilitation unit at least 6 months, independent walking (walking speed > 0.4 m/s), Brunnström recovery stage 3–4, muscle tone of a paretic lower limb (Ashworth ≤ 1 plus), and a level of disability according to the Rankin scale: 3. Stroke was confirmed by computed tomography (CT) or magnetic resonance imaging. Exclusion criteria were: unstable haemodynamic state, peripheral vascular disease, cognitive impairment (Mini Mental Scale < 20) and movement disorders significantly limiting and disrupting the ability to walk. Participants were randomly assigned to an intervention group (n = 25) or a control group (n = 25). Mean time from stroke was 43.8 months. Table I describes the characteristics of the groups.
Intervention
Patients were divided into 2 treatment groups:
• Group I (control group) received a programme with the treadmill training without visual biofeedback and basic physiotherapy consisting of 1.5-h sessions for 10 days (every day Monday to Friday for 2 weeks).
• Group II (intervention group) received a programme with the treadmill training with visual biofeedback and basic physiotherapy consisting of 1.5-h sessions for 10 days (every day Monday to Friday for 2 weeks).
Training was carried out using a Gait Trainer 2 treadmill produced by Biodex (Biodex, serial 0808501) with the function of real-time visualization of the location of foot placement (step length) and the area where the foot should be placed. Gait training using a treadmill with a visual biofeedback of step length, location where the feet should be placed, and an acoustic signal confirming the correct execution of the task was used in the training in intervention group, whereas training with a treadmill alone was used in the control group. In the first exercise, step length (task) and the walking speed at which the participant was able to walk maintaining the symmetry of step length were determined. In each subsequent training, step length and walking speed were increased only to a level at which the participant was able to perform the task without disturbances in gait rhythm, balance, and without signs of excessive fatigue. The same treadmill and exercise duration times (15–30 min) were used for both the intervention and control groups. At the monitor current walking speed, exercise time and distance were presented.
Basic physiotherapy. Before each treadmill training, patients participated in the same basic, self-conducted exercises for 30 min. This included balance exercises in the sitting and standing positions, active exercises, and breathing exercises. All participants trained in the same room and used the same accessories. After the basic exercises, each patient rested for approximately 20 min and began treadmill training. After completion of training on the treadmill and resting, every patient exercised for 15 min in a sitting position using the motorized pedal exerciser (Thera FitPlus, Medica Medizintechnik GmbH, Hochdorf, Germany).
Outcome measures
Primary outcome measure: spatio-temporal parameters of gait. Gait assessment was performed at the Laboratory of Biomechanics of the Institute of Physiotherapy, University of Rzeszów. It was based on a 3-dimensional gait analysis performed using the SMART system (6 cameras, 120 Hz) from BTS Bioengineering (BTS Bioengineering, Milan, Italy). Reference markers were placed according to the internal protocol of the system (Helen Hayes (Davis) Marker Placement) on the sacrum, pelvis (anterior posterior iliac spine), femur (lateral epicondyle, great trochanter and in lower one-third of the shank), fibula (lateral malleolus, lateral condyle end in lower one-third of the shank), foot (metatarsal head and heel) (18). The subjects walked at their comfortable speed and could use auxiliary equipment, such as canes and elbow crutches, during the evaluation. During one study 6 passes of the patient were registered and, subsequently, spatio-temporal parameters were calculated with use of Tracker and Analyzer programs (BTS Bioengineering), averaging the results to a single session. The analysis took into account: cadency (steps/min), gait speed (m/s), swing phase and stance phase (% of gait cycle) of the paretic and of the non-paretic limb and the length of the gait cycle (m).
Secondary outcomes: walking speed in a 10-m test, walking distance in a 2-min walk test, self-reliant mobility using the “Up and Go” test and efficiency in terms of activities of functional independence in the Barthel Index. During the assessment of gait speed (m/s) over 10 m, participants walked at a comfortable speed within their own orthopaedic capabilities (19). The result was the mean of the 2 trials. The 2-Minute Walk Test (m) was performed on the corridor where a 30-m distance was marked with 2 lines (20). Auxiliary lines were also designated every 5 m. The participants walked for 2 min between the 2 lines marking the 30-m distance. During the study, subjects walked at their desired speed and could use their own orthopaedic aids. During the “Up and Go” test, participants were asked to get up from a sitting position in a chair with a backrest of standard height, walk 3 m, turn around at a marked location, return to the chair and sit down unassisted (21). The subjects could perform the task at their desired speed and could use their own orthopaedic aids. Assessment of functional independence was performed using the 20-point version of the Barthel Index (22, 23). Evaluation of the execution of each activity was done by interviewing study participants.
Procedure and randomization
All the patients participated in a 12-day programme. All participants completed the treadmill training programme and performed additional supplementary exercises over 10 consecutive training sessions over a period of 2 weeks and they all participated in the control examination. No adverse events were reported throughout the study period.
On the first day, gait and functional capacity was assessed, followed by 10 days of the exercise programme. A final examination was performed on the last day of the programme. After the initial test, the day before the first training participants were randomly assigned to the intervention group or the control group. A simple computer-generated randomization sequence was made and an automated assignment system was used to ensure allocation concealment. Randomization was performed by a researcher not involved directly in the assessment and treatment of patients. Neither the physiotherapists who evaluated the patients nor those who conducted the basic physiotherapy knew about the patient allocation. The control-intervention group assignment was only known by the physiotherapist conducting the treadmill training (who was not participating in the study and basic physiotherapy), who had no influence on patients’ allocation.
Statistical analysis
The significance of treadmill exercises outcomes in each arm of the study was measured by the comparison of the results of examination before and after the training programme using Wilcoxon test.
Subsequent analyses compared the improvement of measured parameters in the intervention group and in the control group with Mann-Whitney U test. The improvement was measured as the change in the results of examination before and after the programme. The statistical analysis was conducted at a 95% confidence level.
A normal distribution of quantitative data was assessed by means of the Shapiro-Wilk test.
The significance of differences between these 2 groups was assessed with the non-parametric precise version for small samples. The significance threshold level α < 0.05 was assumed. All data were analysed using STATISTICA ver. 10.0 (StatSoft, Poland).
RESULTS
Participants characteristics
A total of 115 patients treated at the Clinical Department of Rehabilitation in Rzeszow in 2009–2011, who met the inclusion criteria, were selected out of 430 patients with a medical history of stroke treated in a rehabilitation ward. Eighty-five people agreed to participate in the programme after being contacted by telephone. Among them, 50 people were randomly selected using a computer programme and were then randomly assigned to either the intervention group or the control group. These 50 participants completed the study without any changes in allocation. The flow of the subjects through the study is shown in Fig. 1. The mean age of the participants was 62 years. Time from onset of stroke in both groups was characterized by a large range (mean 8–180 months). The mean time from stroke in the intervention group was 47.5 months and in the control group, 40 months. Demographic and clinical characteristics at baseline are shown in Table I. Characteristics of the participants in the intervention group and the control group did not differ significantly before the start of the programme.
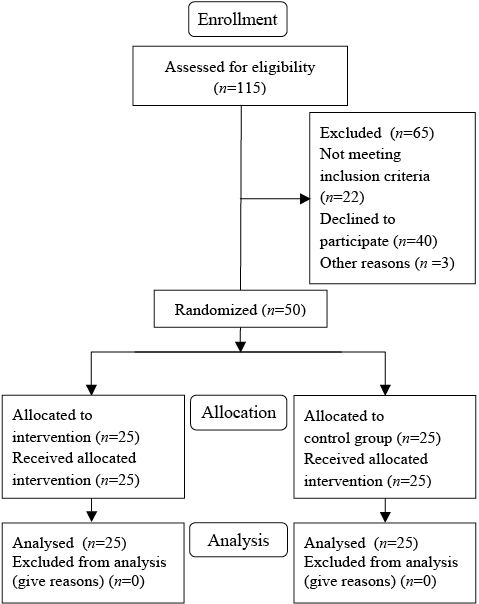
Fig. 1. Flow of participants through the trial.
|
Table I. Demographic characteristics and clinical assessment of participants at baseline |
||
|
Intervention group (n = 25) |
Control group (n = 25) |
|
|
Age, years, mean (SD), [range] |
59.8 (11.7) [38–77] |
61.9 (11.4) [42–79] |
|
Sex women/men, n (%) |
8 (32)/17 (68) |
10 (40)/15 (60) |
|
Time after stroke, months, mean (SD) [range] |
47.5 (43.0) [8–180] |
40.0 (41.5) [8–180] |
|
Side of paresis n (%) |
||
|
Left-sided hemiparesis |
21 (84) |
14 (56) |
|
Right-sided hemiparesis |
4 (16) |
11 (44) |
|
Cadence, steps/min, mean (SD) |
68.9 (10.6) |
67.5 (15.5) |
|
Velocity (m/s), mean (SD) |
0.45 (0.20) |
0.45 (0.11) |
|
STF p (% of cycle), mean (SD) |
66.0 (6.1) |
68.3 (7.2) |
|
STF np (% of cycle), mean (SD) |
74.5 (5.2) |
74.4 (5.1) |
|
SWF p (% of cycle), mean (SD) |
34.0 (6.1) |
31.7 (7.2) |
|
SWF np (% of cycle), mean (SD) |
25.5 (5.2) |
25.6 (5.2) |
|
LC p (m), mean (SD) |
0.68 (0.17) |
0.65 (0.12) |
|
LC np (m), mean (SD) |
0.66 (0.19) |
0.65 (0.13) |
|
10-m walk test (m/s), mean (SD) |
0.60 (0.2) |
0.58 (0.14) |
|
2-min test (m), mean (SD) |
78.9 (24.2) |
65.7 (31.3) |
|
“Up and Go” test (s), mean (SD) |
16.5 (7.7) |
18.6 (8.2) |
|
Barthel Index, median (IQR) |
17.0 (3.0) |
16.0 (2.0) |
|
SD: standard deviation; STF p: stance phase of the paretic limb; STF np: stance phase of non-paretic limb; SWF p: swing phase of paretic limb; SWF np: swing phase of non-paretic limb; LC p: length of the cycle of paretic limb; LC np: length of the cycle of non-paretic limb; IQR: interquartile range. |
||
Effect of gait training within each arm of the study
Primary outcome. Rehabilitation programme using a treadmill in the late period after stroke resulted in a significant improvement in gait and functional efficiency within both arms of the study. Analysis of the results of spatio-temporal tests performed at the beginning and end of the training programme showed significant improvement in all evaluated parameters (Table II). In the intervention group the mean stance phase duration on the non-paretic limb in the initial examination lasted 74.5% of the gait cycle (SD 5.2) and shortened to 67.1% (SD 5.0; p = 0.001). In the control group the mean stance phase duration on the non-paretic limb in the initial examination lasted 74.4% of the gait cycle (SD 5.1), and after the end of the programme shortened to 70.4% (SD 5.5; p = 0.001). In both groups the mean value of stance phase duration on the paretic limb was shortened: in the intervention group from 66.0% of the gait cycle (SD 6.1) to 62.7% (SD 2.9) (p = 0.0128), and in the control group from 68.3% of the gait cycle (SD 7.2) to 66.6% (SD 5.1; p = 0, 0199). The stance phase was reduced, while the duration of the swing phase was lengthened. Elongation of the swing phase of both limbs was demonstrated at the end of the programme in both the intervention group and the control group. In both groups, elongation of the gait cycle of both the paretic and the non-paretic limb was highly statistically significant (p < 0.0001).
|
Table II. Comparison of the studied parameters before and after the programme in the intervention group and in the control group |
|||||||
|
Intervention group |
Control group |
||||||
|
Pre- training Mean (SD) |
Post-training Mean (SD) |
p-value |
Pre-training Mean (SD) |
Post-training Mean (SD) |
p-value |
||
|
Primary outcomes |
|||||||
|
Cadence(steps/min) |
68.9 (10.6) |
78.0 (12.3) |
< 0.0001 |
67.5 (15.5) |
73.6 (16.8) |
< 0.0001 |
|
|
Velocity (m/s) |
0.45 (0.17) |
0.60 (0.18) |
< 0.0001 |
0.45 (0.11) |
0.57 (0.15) |
< 0.0001 |
|
|
STF (% of cycle), p |
66.0 (6.1) |
62.7 (2.9) |
0.0128 |
68.3 (7.2) |
66.6 (5.1) |
0.0199 |
|
|
STF (% of cycle), np |
74.5 (5.2) |
67.1 (5.0) |
0.001 |
74.4 (5.1) |
70.4 (5.5) |
0.001 |
|
|
SWF (% of cycle), p |
34.0 (6.1) |
37.3 (2.9) |
0.0128 |
31.7 (7.2) |
33.4 (5.1) |
0.001 |
|
|
SWF (% of cycle), np |
25.5 (5.2) |
32.9 (5.0) |
0.001 |
25.6 (5.1) |
29.6 (5.5) |
0.001 |
|
|
LC (%), p |
0.68 (0.17) |
0.80 (0.18) |
< 0.0001 |
0.65 (0.12) |
0.72 (0.14) |
< 0.0001 |
|
|
LC (%), np |
0.66 (0.19) |
0.81 (0.18) |
< 0.0001 |
0.65 (0.13) |
0.71 (0.14) |
< 0.0001 |
|
|
Secondary outcomes |
|||||||
|
10-m walk test (m/s) |
0.60 (0.20) |
0.78 (0.23) |
< 0.0001 |
0.58 (0.14) |
0.70 (0.19) |
0,0001 |
|
|
2-min test (m) |
78.9 (24.2) |
97.4 (26.7) |
< 0.0001 |
65.7 (31.3) |
82.4 (37.3) |
< 0.0001 |
|
|
“Up and Go” test (s) |
16.5 (7.7) |
12.0 (4.0) |
0,0001 |
18.6 (7.2) |
14.4 (6.6) |
< 0.0001 |
|
|
Barthel Index, median (IQR) |
17.0 (3.0) |
18.0 (1.0) |
0,0001 |
16.0 (2.0) |
17.0 (2.0) |
0,00001 |
|
|
SD: standard deviation; STF p: stance phase of the pateric limb; STF np: stance phase of non-paretic limb; SWF p: swing phase of the paretic limb; SWF np: swing phase of non-paretic limb; LC p: length of the cycle of paretic limb; LC np: length of the cycle of non-paretic limb; p: Wilcoxon test result (pre- to post- training); IQR: interquartile range. |
|||||||
Secondary outcome. In the intervention group the mean walking speed at initial examination was 0.6 m/s (SD 0.2) and increased in the final examination to 0.78 m/s (SD 0.23). Similarly, patients from the control group increased the mean value of comfortable walking speed from 0.58 m/s (SD 1.4) to 0.70 m/s (SD 1.9). The expected effect of treadmill training was the increase in walking distance, which was confirmed in both groups. In the intervention group the mean distance in the 2-min walk test increased from 78.9 m (SD 24.2) to 97.4 m (SD 26.7), and in the control group it increased from 65.7 m (SD 33.1) to 82.4 m (SD 37.3). After completing the programme, patients in the intervention group and in the control group showed improvement in the independence level assessed in the Up & Go test, as well as the self-service level (Table II).
Comparison of treadmill training and biofeedback with treadmill alone
The key question in the study was whether the use of biofeedback in training with a treadmill results in improvement in patients’ outcome. For this purpose the patients’ outcome measured as improvement in spatio-temporal parameters assessed at the beginning and at the end of the programme was assessed in both arms of the study. Statistically significant improvement of the outcomes of rehabilitation was observed in the intervention group vs control group in a range of spatio-temporal parameters (Table III). Significantly greater increase in the gait cycle length of the non-paretic limb was observed in the intervention group compared with the control group (mean values 0.14 m vs 0.07 m, respectively; p = 0.0021). A greater increase in the duration of the swing phase of the non-paretic lower limb was also shown in the intervention group compared with the control group (7.3% vs 4.0%; p = 0.0042). The intervention group also revealed a greater effect of rehabilitation in terms of the stance phase duration for the non-paretic limb (–7.3% vs –4.0%; p = 0.0045). The mean change value of the other spatio-temporal parameters analysed was higher in the intervention group, but the difference was not statistically significant. Patients in the intervention group shortened the stance phase of the affected limb by a mean of 3.3% and patients in the control group of 1.7% (p = 0.2092). The swing phase of the paretic limb has also been extended by 3.3% in the study group and by 1.7% in the control group (p = 0.2092). The length of the gait cycle of the paretic limb increased by 0.12 m in the study group and by 0.08 m in the control group (p = 0.0679). The shortened stance phase, extended swing phase and increased gait cycle of the affected limb were also observed in the intervention group; however, the differences were not statistically significant.
In additionally evaluated parameters in the intervention group a greater mean change between the results of the initial and final tests was demonstrated, but the differences were not statistically significant (Table III).
|
Table III. Change in the parameters tested after completion of the programe |
|||
|
Treatment effect – differences pre- vs post- training |
p-value |
||
|
Intervention Mean (95% CI) |
Control Mean (95% CI) |
||
|
Primary outcomes |
|||
|
Cadence (steps/min) |
9.1 (6.3 to 11.9) |
6.0 (4.0 to 8.1) |
0.0807 |
|
Velocity (m/s), |
0.15 (0.11 to 0.20) |
0.13 (0.09 to 0.17) |
0.2887 |
|
STF (% of cycle), p |
–3.3 (–5.6 to –0.9) |
–1.7 (–3.9 to 0.5) |
0.2092 |
|
STF (% of cycle), np |
–7.3 (–9.0 to –5.7) |
–4.0 (–5.5 to –2.5) |
0.0045 |
|
SWF (% of cycle), p |
3.3 (0.9 to 5.6) |
1.7 (–0.5 to 3.9) |
0.2092 |
|
SWF (% of cycle). np |
7.3 (5.7 to 9.0) |
4.0 (2.5 to 5.5) |
0.0042 |
|
LC (m), p |
0.12 (0.09 to 0.16) |
0.08 (0.05 to 0.10) |
0.0679 |
|
LC (m), np |
0.14 (0.10 to 0.19) |
0.07 (0.03 to 0.10) |
0.0021 |
|
Secondary outcomes |
|||
|
10-m walk test (m/s) |
0.18 (0.12 to 0.23) |
0.12 (0.08 to 0.16) |
0.1310 |
|
2-min test (m). |
18.6 (13.3 to 23.8) |
16.6 (11.8 to 21.5) |
0.5768 |
|
“Up and Go” test (s). |
–4.5 (–6.6 to –2.5) |
–4.2 (–5.2 to –3.2) |
0.4882 |
|
Barthel Index median, (25–75th quartiles) |
1.0 (1.0 to 2.0) |
1.0 (1.0 to 1.0) |
0.1261 |
|
95% CI: 95% confidence interval; STF p: stance phase of the pateric limb; STF np: stance phase of non-paretic limb; SWF p: swing phase of paretic limb; the SWF np: swing phase of non-paretic limb; LC p: length of the cycle of paretic limb; LC np: length of the cycle of non-paretic limb; p: Mann-Whitney U test result. |
|||
DISCUSSION
The aims of this study were to evaluate the effects of gait training using a treadmill in patients in the late period after stroke and to assess the usefulness of visual biofeedback. The effectiveness of training on a treadmill and the use of biofeedback methods are confirmed by many studies in people after stroke. Increased walking speed and improved quality of gait is obtained by increasing the loading time of the paretic limb. Introduction of additional external auditory and visual information about proper gait pattern and its parameters, i.e. speed, step length and symmetry of gait phases while using a treadmill, allows the patient not only to improve symmetry of gait, but also to stimulate balance, coordination and strength, as well as endurance of the relevant muscle groups (24–28). In addition, patient motivation to perform exercises is reinforced by visualizing the accuracy of the task on the screen and acoustic biofeedback. Cho et al. (29) showed that, with the improvement in gait function, activation of the primary somatosensory cortex shifted significantly from the normal hemisphere to the affected one in a group of patients who participated in 4-week training programme with visual biofeedback. Anderson et al. (30) report that biofeedback based on information about accuracy and errors in the patients’ performance of the tasks is very useful in the training of individual skills. The delivered external information allows patients to improve the movement. Also Roerdink et al. (31) showed in their study that adding external audio information to exercise on a treadmill resulted in improvement in symmetry and coordination of gait in patients with hemiparesis in the late period after stroke. The results suggest that training on a treadmill with visual biofeedback provides an effective way to change gait patterns and improve the frequency of steps, symmetry and coordination of gait in people after stroke; therefore, it can be used in the practice of physiotherapy. Schauer & Mauritz (32) reported that acoustic biofeedback training affects not only the improvement in gait symmetry, but also helps patients with hemiparesis after stroke to achieve greater speed and increase the length of the gait cycle. In our study, we demonstrated that the rehabilitation programme using a treadmill in the late period after stroke significantly affected the improvement in gait of the participants. When analysing results of clinical tests and spatio-temporal parameters, a marked improvement was found in all of the evaluated parameters within both intervention and control groups. This indicates that patients after stroke can improve mobility beyond the early period of recovery, and that applying the intensified gait re-education programme supplemented by training on a treadmill improves mobility in the late period after stroke. Similarly, Harris-Love et al. (33) showed that the use of re-education of gait training on a treadmill is justified because it affects the restoration of a symmetrical gait pattern. Exercise on a treadmill in patients in the late period after stroke resulted in a decrease in asymmetry of stance and swing phases duration between the paretic and unaffected limbs. Patients achieved elongation of the stance phase of the paretic limb with respect to the non-paretic limb. Bayat et al. (34) showed that patients with stroke who exercised on a treadmill revealed an increase in step length, which in turn led to an augmentation in their walking speed. In addition, treadmill training allows for individual adjustment of step frequency and walking speed, which is important in the rehabilitation of patients after cerebrovascular accidents.
Importantly, this study shows that the use of biofeedback in treadmill training significantly improves patients’ outcomes. The intervention group had a significantly greater increase in gait cycle length on the non-paretic side and duration of the swing phase of the non-paretic lower limb. Superior effects of rehabilitation in the intervention group were also related to the improved symmetry of duration of the stance phase. The objective of the gait learning on a treadmill with biofeedback was achieved. It was assumed that the real-time visualization of the feet placement and the area where they should be placed will influence normalization and improvement in spatio-temporal gait parameters. Patients from both groups shortened the swing phase of both paretic and non-paretic limbs, with simultaneous extension of the stance phase. In the group with biofeedback the change in spatio-temporal parameters of the non-paretic limb was higher than in the group without biofeedback; however, the difference between groups was not at a high significance level (p > 0.001). In the group with biofeedback, motor learning effect was significantly higher compared with the control group, but concerned non-paretic limb only. This fact can be explained by a too short duration of the programme, which may limit motor learning possibility in the late period after stroke, especially in the field of motor control of the paretic limb. It should be emphasized that the improvement in other parameters in the group with biofeedback was higher than in the group without biofeedback, but it was not statistically significant.
The results do not allow for an unequivocal answer to the question of whether the form of feedback used gave greater effects of gait learning compared with training on a treadmill without feedback. Treadmill training contributed to the normalization of spatio-temporal parameters of gait in both groups, mainly in the elongation phase of transfer and shortening phases. This, along with the simultaneous significant increase in walking speed, seems to be obvious. The important clinical effect of the programme was a significant increase in walking speed and distance, with improvement in the level of gait independence and self-reliance in both groups. The visual feedback used in gait training engaged the patient to concentrate on the exercise by providing additional information, and the provided real-time results provided motivation to train. This study showed that improvement in gait in the late period after stroke using a treadmill brings beneficial effects, and that visual feedback used during training is an important complement of the method. Slight differences demonstrated in favour of group exercising with biofeedback should be the subject of further studies with a longer treatment time.
Similarly, Ando et al. (35) showed that training on a treadmill with biofeedback improves the symmetry of gait in patients with hemiparesis in the late period after stroke. They obtained prolongation of the stance phase of the paretic limb in relation to the unaffected limb. Massaad et al. (36) indicated that training on a treadmill with biofeedback reduces energy expenditure of gait in patients with hemiparesis in the late period after stroke. The authors showed that, after training on a treadmill with biofeedback, the amplitude of sway of the body’s centre of mass decreased by 10%, particularly during loading of the non-paretic limb. Aiello et al. (37) also evaluated the effectiveness of gait training on a treadmill with visual biofeedback. Training consisted of 12 sessions on a treadmill supplemented by electromyography biofeedback. The authors observed improvement in gait, which was characterized by an increase in walking speed and loading time and a decrease in the knee joint’s extension moment of the paretic limb.
The limitation of this study is that the duration of the programme for each participant was only 2 weeks (10 sessions). The restriction was due to logistical reasons on the part of caregivers who, in many cases, had to take days off from work to prepare and accompany the family members participating in the programme. A longer duration of therapy would allow for better outcomes of motor training.
In conclusion, gait training using either a treadmill alone or a treadmill with visual biofeedback results in significant improvement in gait parameters and functional capacity in patients with hemiparesis in the late period after stroke. Our findings also indicate that use of a treadmill with visual biofeedback gives better results in terms of improving gait cycle length, duration of gait phases and swing phase speed compared with the effects of exercise on the treadmill without use of biofeedback. It is an effective complement to a rehabilitation programme.
REFERENCES
