Kylee J. Lockwood, MPH1, 2, Nicholas F. Taylor, PhD1, 2 and Katherine E. Harding, PhD2
From the 1School of Allied Health, La Trobe University and 2Allied Health Clinical Research Office, Eastern Health, Melbourne, Australia
OBJECTIVE: To determine the effectiveness of pre-discharge home assessment visits by occupational therapists in assisting hospitalized patients from a range of settings to return to community living.
DATA SOURCES: Electronic databases MEDLINE, CINAHL, Embase, PsychINFO, Cochrane Central Register of Controlled Trials and OTseeker were searched until February 2014.
STUDY SELECTION: Quantitative and qualitative studies were included if they evaluated pre-discharge home assessment visits by an occupational therapist. Of 1,778 potentially relevant articles, 14 studies met the inclusion criteria.
DATA EXTRACTION: After data extraction, study quality was assessed using check-lists.
DATA SYNTHESIS: Pre-discharge home assessment visits reduced the risk of falling (risk ratio 0.68, 95% confidence interval (95% CI) 0.49–0.94) and increased participation levels (standardized mean difference 0.49; 95% CI 0.01–0.98) in geriatric and mixed rehabilitation settings. The risk of readmission to hospital was also reduced (risk ratio 0.47, 95% CI 0.33–0.66), but not for patients following stroke. There was no effect on activity or quality of life. Patients and carers perceived that home assessment visits were beneficial and were satisfied with the process.
CONCLUSION: There is low-to-moderate quality evidence that pre-discharge home assessment visits reduce patients’ risk of falling and increase participation. The risk of readmission to hospital is also reduced, but not for patients following stroke.
Key words: home visit; occupational therapy; patient discharge; review.
J Rehabil Med 2015; 47: 289–299
Correspondence address: Kylee Lockwood, School of Allied Health, La Trobe University, Melbourne, Australia. E-mail: K.Lockwood@latrobe.edu.au
Accepted Nov 5, 2014; Epub ahead of print Mar 16, 2015
Introduction
Healthcare services are under continuing pressure to use resources efficiently and effectively. Demand for inpatient beds continues to grow, and so preventing admissions and reducing length of stay are priorities (1). Occupational therapists often perform home assessment visits with patients prior to discharge from hospital to determine when and if a hospitalized person should return to their own home. Pre-discharge home assessment visits involve taking patients to their home for a short period of time and assessing their ability to perform occupations of daily living within their own environment (2). Pre-discharge home assessment visits are conducted across a wide range of hospital settings and diagnostic groups. They are most often a single visit prior to discharge from hospital to assess and practise transfers, mobility and activities of daily living. They also involve provision of education, advice and recommendations on equipment and home adaptations. A pre-discharge home assessment visit often differs from an access or environmental visit where the primary aim is to determine the need for equipment or environmental modifications and the occupational therapist attends the property without the patient (3). This is also distinct from a preventive home visit for community-dwelling people, which aims to increase autonomy through prevention activities (4). There has been increasing pressure to reduce the number of home assessment visits completed at some health services, given that it is a time-consuming and costly intervention (5). As a result, it is important that clinicians and health service managers are clear about when and for whom a home assessment visit should be completed and whether home visits assist patients to return to community living.
Three systematic reviews have been published investigating the effectiveness of occupational therapy home assessment visits. The first systematic review, by Patterson & Mulley in 1999 (6), identified 5 published studies, with none being randomized controlled trials (RCTs), and concluded that the effectiveness of pre-discharge home assessment visits was uncertain. A systematic review by Barras in 2005 (7) included both pre-discharge and post-discharge home visits and again reported that they had not been studied in enough detail to assess effectiveness adequately. The author suggested that home visits may influence quality of life, number of falls and patient autonomy; however, this was based on limited data. A review of qualitative studies by Atwal et al. in 2012 (8) investigated the users’ perspectives of the effectiveness of home assessment visits, but also found a limited body of research with only 3 included studies. In addition, Shepperd et al. (9) investigated the effectiveness of all aspects of discharge planning, including home assessment visits. They concluded that a structured discharge plan tailored to the individual patient, which may or may not include a home assessment visit, probably brings about a reduction in hospital length of stay and readmission rates, and an increase in patient satisfaction; however, the impact on health outcomes was uncertain. Therefore, there remains uncertainty about the effectiveness of pre-discharge home assessment visits. We are not aware of any review to date that has focused on pre-discharge home assessment visits, including both quantitative and qualitative studies and a meta-analysis for the synthesis of quantitative data.
The aim of this review was to determine the effect of pre-discharge home assessment visits across a range of hospital settings and diagnostic groups on outcomes associated with return to community living. The outcome of community living reflects the main aims of a home assessment visit, which are to maximize a person’s functioning in their own environment and prevent adverse events.
MethodS
The Prepared Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) were used as a reference to guide reporting in this review (10). Methods of analysis and inclusion criteria were specified in advance and documented in a protocol registered on PROSPERO (registration no. CRD42013004195).
Data sources
Electronic databases MEDLINE, CINAHL, Embase, PsychINFO, Cochrane Central Register of Controlled Trials and OTseeker were searched from the earliest available date until February 2014. Reference lists of included articles were manually scanned and citations of all included articles were tracked using Google Scholar to locate additional articles not identified by database searching. The search strategy was based on 3 key concepts: hospitalized patients, home assessment visits and occupational therapy (Table I).
|
Table I. Search strategy as applied in MEDLINE |
|
|
Search strategy |
|
|
1 |
inpatient*.mp. |
|
2 |
rehabilitation.mp. |
|
3 |
acute care.mp. |
|
4 |
subacute care.mp. |
|
5 |
hospital*.mp. |
|
6 |
1 OR 2 OR 3 OR 4 OR 5 |
|
7 |
home visit*.mp. |
|
8 |
home assessment*.mp. |
|
9 |
home environment.mp. |
|
10 |
home evaluation.mp. |
|
11 |
home modification*.mp |
|
12 |
home safety.mp |
|
13 |
discharge plan*.mp |
|
14 |
7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 |
|
15 |
occupational therapy |
|
16 |
occupational therapist* |
|
17 |
15 OR 16 |
|
18 |
6 AND 14 AND 17 |
Eligibility criteria
Studies were eligible for inclusion in this review if the participants were hospitalized patients. This included patients who were admitted to acute or subacute (rehabilitation) care. Studies relating to patients who were not hospitalized or who were residing in permanent institutional care were excluded as they do not meet one of the primary aims of a pre-discharge home assessment visit, which is to facilitate discharge home. There were no age restrictions for inclusion in the review.
The intervention was defined as a home visit conducted by an occupational therapist for the purpose of assessment and discharge planning prior to the patient’s discharge from hospital. Therefore programmes providing therapeutic home visits in which multiple therapy sessions or training were conducted in the home as well as home visits conducted by other health professionals without the presence of an occupational therapist were excluded. The primary outcome of interest was return to community living. Any outcome that reflected successful return to community living was included, such as falls, readmissions, quality of life, and the activity and participation domains of the International Classification of Functioning, Disability and Health (11). Activity focuses on what a person can do in a standard environment (their level of capacity) and participation focuses on what a person can do in their usual environment (their level of performance). Patient and carer perspectives on specific experiences of a home assessment visit and how it impacted on return to community living were included. However, therapists’ opinions and perceptions about the value and purpose of pre-discharge home assessment visits were excluded. Although therapists’ opinions are valuable, they predominantly contribute to the understanding of the purpose and the process of the home assessment visit, whereas the primary aim of this review was to understand the contribution that these visits make to the outcome of returning to community living.
Since the aim of the review was to determine the effect of pre-discharge home assessment visits on outcomes associated with return to community living, studies were included with any research design that could address the research question. Therefore qualitative and quantitative research designs were included.
Study selection
The title and abstract of the papers identified in the initial search were assessed by 2 reviewers independently (KL, KH) and those that clearly did not meet the criteria were excluded. Full-text copies of studies that could not be clearly included or excluded from the title and abstract were reviewed and any disagreements were resolved by consensus. If consensus could not be reached, a third reviewer was consulted to arbitrate (NT). Cohen’s kappa (κ) (12) was used to assess the agreement between the 2 reviewers.
Risk of bias and data extraction
All studies were appraised for methodological quality and risk of bias by 2 reviewers independently (KL, KH). Results were discussed until consensus was reached. Papers were not included or excluded on the basis of the score; however, quality was considered during interpretation of results.
Different tools were used for quantitative and qualitative studies. The Downs and Black (13) checklist was used for quantitative studies and the McMaster Critical Review form (14) for qualitative studies.
The Downs and Black checklist can be used for randomized and non-randomized studies and comprises 27 questions divided into 5 subsections. The subsections include: reporting (10 items), external validity (3 items), internal validity bias (7 items), internal validity confounding (6 items) and power (1 item). The question relating to power was scored out of 5, but was modified so that a score of 5 represented a clearly powered study, a score of 3 was marginally powered, and a score of 0 meant the study was not sufficiently powered (15). The quantitative studies were given a maximum score of 32 points.
The McMaster Critical Review form was used for qualitative studies and comprises 8 subsections, including study purpose, literature, study design, sampling, data collection, data analyses, overall rigour and conclusions and implications. This checklist has guidelines for appraisal and has demonstrated acceptable levels of inter-rater reliability (14, 16).
A customized data extraction form was developed. The following information was collected for each study: study objectives, study design, recruitment procedures, population, setting, participants’ characteristics (number, age, gender, living situation), intervention (description, who attended), outcomes used (primary and secondary outcomes, outcome measures used), adverse events, results and conclusion.
Data synthesis
Data were initially analysed using a process of descriptive synthesis. The data were extracted and organized into tables to compare the characteristics and results of the included studies. In addition, standardized mean differences (SMDs), otherwise known as effect sizes, and 95% confidence intervals (95% CI) were calculated for continuous data from post-intervention means and standard deviations (SDs) for quantitative studies in which sufficient data could be retrieved. If standard deviations were not reported, the standard error was converted to standard deviation or estimated from interquartile ranges if these data were provided (17). For dichotomous data, the risk ratio (RR) and 95% CI for each individual study were calculated.
Meta-analyses were performed with a random effects model using inverse variance analysis with the software Review Manager (18). The random effects method incorporates heterogeneity into the analysis, resulting in a wider confidence interval and a more conservative claim of statistical significance (17). Data were considered clinically homogenous if a similar outcome was assessed on hospitalized patients after a home assessment visit completed by an occupational therapist. For continuous data, the strength of the SMD was determined descriptively according to Cohen (19), with 0.2 regarded as small, 0.5 as moderate, and 0.8 as large. For dichotomous data, meta-analyses were expressed as risk ratios. The statistical heterogeneity of studies combined in meta-analyses was assessed by calculating I2, which described the total statistical variation across the studies as a percentage with values of greater than 50% indicating moderate to high statistical heterogeneity (17). A sensitivity analysis was performed for any meta-analysis where I2 was greater than 50%, excluding studies judged to be contributing to heterogeneity. When studies could not be combined in meta-analysis, a narrative format was used to report individual study results.
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was applied to each meta-analysis to determine the quality of evidence across the included studies (20). Randomized controlled trials were considered high quality and at low risk of bias. The quality of evidence was downgraded by 1 level if: (i) the majority of studies in the meta-analysis were of poor methodological quality (< 20 on Downs and Black checklist), (ii) there was greater than low levels of statistical heterogeneity between the studies (I2≥ 25%) (21), (iii) there were large confidence intervals (> 0.8). This resulted in 4 levels of quality of evidence: high, moderate, low and very low. The reasons for downgrading were documented.
Results
Study selection
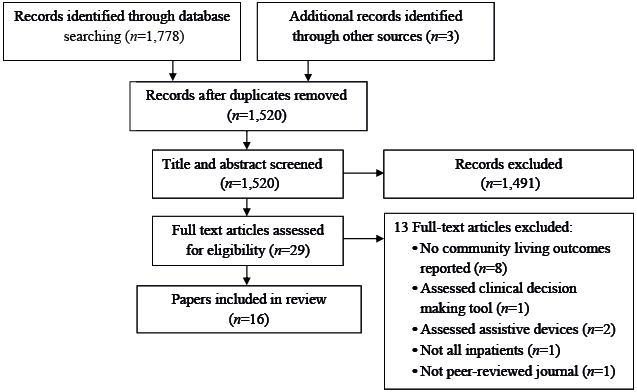
The electronic database search yielded 1,778 records. Three additional studies were identified through reference checking and citation tracking (22–24). After duplicates were removed, 1520 remained and were screened on title and abstract. Agreement between the reviewers on which studies met the selection criteria was good (κ = 0.79; 95% CI 0.64–0.93). Full-text copies of 29 papers were assessed for eligibility and a further 13 were excluded, resulting in a final yield of 16 papers (Fig. 1). The level of agreement when considering full-text articles was good (κ = 0.75; 95% CI 0.50–1.00). Two papers provided data about the same cohort study (25, 26) and 2 papers reported data about different outcomes of the same randomized controlled trial (24, 27). To avoid duplication and overlap of reporting of data in these studies, the paper with the most relevant and complete data was used in relation to specific outcome measures. Therefore this resulted in a final yield of 14 studies from 16 papers.
Risk of bias within studies
The mean score on the Downs and Black checklist across all quantitative studies was 20, ranging from 3 to 27 (Table II). No study blinded participants or therapists to the intervention they received, which was not unexpected given the nature of the intervention. Three studies had blinded assessors (2, 3, 23) and 3 had allocation concealment (2, 3, 23). Of the 3 qualitative studies, sampling, data collection methods and data analysis were clearly described in 2 studies (28, 29). None of the qualitative studies adequately described the study design or theoretical framework used. The agreement between reviewers when rating individual items for quality was good (κ=0.64; 95% CI 0.57–0.72).
|
Table II. Methodological quality of included quantitative studies |
||||||
|
Study details |
Reporting (maximum = 11) |
External validity (maximum = 3) |
Internal validity |
Power (maximum = 5) |
Total (maximum = 32) |
|
|
Bias (maximum = 7) |
Confounding (maximum = 6) |
|||||
|
Barras, 2008 (25) |
7 |
3 |
4 |
3 |
3 |
20 |
|
Bore, 1994 (35) |
1 |
0 |
2 |
0 |
0 |
3 |
|
Drummond et al., 2013 (3) |
10 |
2 |
5 |
5 |
3 |
25 |
|
Hagsten et al., 2004 (27) |
8 |
2 |
4 |
4 |
5 |
23 |
|
Hagsten et al., 2006 (24) |
9 |
1 |
3 |
4 |
5 |
22 |
|
Johnston et al., 2010 (26) |
10 |
1 |
5 |
3 |
3 |
21 |
|
Lannin et al., 2007 (2) |
10 |
2 |
5 |
5 |
3 |
25 |
|
Luker & Grimmer-Somers, 2009 (31) |
9 |
3 |
4 |
2 |
0 |
18 |
|
Nikolaus & Bach, 2003 (23) |
10 |
2 |
5 |
5 |
5 |
27 |
|
Pardessus et al., 2002 (30) |
9 |
0 |
5 |
4 |
3 |
21 |
|
Renforth et al., 2004 (32) |
7 |
3 |
4 |
4 |
3 |
21 |
|
Rosenblatt et al., 1986 (22) |
7 |
2 |
2 |
3 |
0 |
14 |
|
Whitaker & Hornby, 1986 (33) |
7 |
3 |
2 |
4 |
0 |
16 |
Study characteristics
Table III summarizes the characteristics of included studies. Of the 14 studies that were included in the final review 5 were RCTs, 6 were observational studies (1 cohort study, 4 retrospective chart audits and 1 survey) and 3 were qualitative. The length of follow-up varied from 1 month (3) to 12 months (23, 30).
The sample sizes of the included studies ranged from 10 (2) to 400 (25). Six studies were conducted in acute hospitals and 8 studies in rehabilitation or intermediate care settings. The studies predominantly comprised of a mixed cohort of adults, but 2 focussed on patients following hip fracture (22, 27) and 2 following stroke (3, 31). Older adults were the subject of 8 of the studies and mean ages across all studies ranged from 72 (3) to 86 years (29).
There was large variation in the detail provided regarding the content of the home assessment visit. Four of the RCTs described the use of protocols or standardized checklists when completing home assessment visits (2, 3, 23, 30). Four of the RCTs compared occupational therapy pre-discharge home assessment visits with standard care, which included in-hospital assessment and education by an occupational therapist (2, 3, 23, 30). One RCT conducted at least one further home visit to reinforce recommendations (23). One RCT included individualized training by the occupational therapist as well as a pre-discharge home assessment visit, but the control group received no contact with an occupational therapist (27). Four studies reported details about the time spent on the home assessment visit (2, 3, 25, 32). The mean duration ranged from 45 min (2) to 58 min (25). Two studies reported on the mean total time (including travel, completing the visit and report writing) as 147 min (25) and 180 min (3). The number of home assessment visits resulting in recommendations for equipment ranged from 52% (27) to 93% (32).
The outcomes that were measured were diverse. The most common outcomes included: falls (3, 23, 25, 26, 30), readmissions to hospital (2, 3, 25, 30, 33), quality of life (2, 3, 24, 25), activity (2, 3, 30) and participation (2, 30). The patient’s experiences, perception of the value of the visit, and satisfaction with the home assessment process were also explored in a number of the studies (25, 28, 29, 34, 35). Specific outcome measures used are detailed in Table III.
|
Table III. Summary of included trials |
|||||||
|
Study |
Country and setting |
Study design |
Participants |
Intervention |
Outcome measured |
Assessments used |
Key results |
|
Atwal et al., 2008 (29) |
England Acute inpatient (geriatric) |
Qualitative Semi-structured interviews |
n = 22 Age (years) = 86.4 (range 73–95) Female (%) = 60 |
Exp = Pre-discharge HAV with OT, Comp = No comparison |
•Preparation for HAV •Participation in HAV •Perception of HAV •Involvement in decision-making process |
HAVs can increase anxiety for patients but reduce anxiety for carers. Older adults often reluctant to accept changes or stop valued occupations. |
|
|
Barras, 2008 (25) and Johnston et al., 2010 (26) |
Australia Inpatient rehabilitation (mixed) |
Prospective observational cohort study |
n = 400 Age (years) = 76 (range 29–96) Female (%) 66 |
Exp = Pre-discharge HAV with OT, Comp = In-hospital assessment and education with OT |
•Falls risk •No. and severity of falls •Quality of Life (QOL) •Disability •Equipment provision and recommendations |
FRASS (37) Falls calendar WHOQoL-BREF (38) FIM (39) |
Patients who had a HAV were less likely to be readmitted to hospital (OR = 0.5, 95% CI 0.3–0.8), less likely to fall (OR 0.5, 95% CI 0.3–0.9) and had improved quality of life scores. |
|
Bore, 1994 (35) |
England Community hospital (geriatric) |
Questionnaire |
n = 18 Age (years) = 81.2 (range 65–93) Female (%) = 83 |
Exp = Pre-discharge HAV with OT, Comp = No comparison |
•Degree of consensus regarding content of HAV •Satisfaction HAV |
HAVs were found to be beneficial but there were differences between the perceptions of patients, carers and therapists. |
|
|
Clark & Dyer, 1998 (34) |
England Acute inpatient |
Qualitative Semi-structured interviews |
n = 28 Age (years) = unknown Female (%) = unknown |
Exp = Pre-discharge HAV with OT, Comp = No comparison |
•Experience of the discharge process related to supply of equipment and/or adaptations as a result of HAV •Impact on independence as defined by the patient |
Older people were often anxious and not fully involved in HAV. The process was driven more by need for safe discharge than enhancing independence. |
|
|
Drummond et al., 2013 (3) |
England Inpatient rehabilitation (stroke) |
RCT |
n = 93 Age (years) = 72.1 (range 34–99) Female (%) = 46 |
Exp = Pre-discharge HAV with OT, Comp = Structured hospital-based interview with OT |
•ADL •Disability •Mood •Quality of life •Mobility •No. of falls and readmissions •Carer strain •Resource use |
NEADL (40) Barthel Index (41) Modified Rankin Scale (42) GHQ-28 (43) SADQ-10 (44) EQ-5D (45) RM I (46) CSI (47) |
No significant difference between groups for ADL at 1 month. Mood was better in HAV group at 1 week (p = 0.05) and readmissions were less in control group at 1 month (p = 0.04). |
|
Hagsten et al., 2004 (27) and Hagsten et al., 2006 (24) |
Sweden Acute inpatient (hip fracture) |
RCT |
n = 100 Age (years) Exp 81 (range 68–93), Comp 79 (range 65–95) Female (%) = Exp 84, Comp 76 |
Exp = Daily individualized training and pre-discharge HAV with OT, Comp = Conventional care, no OT involvement |
•ADL •Need for technical aids and/or home adaptations •Quality of life |
Klein-Bell ADL Scale (48) Disability Rating Index (49) SWED-QUAL (50) |
Statistically significant improvements (p < 0.05) in HAV group after 2 months regarding self-reported IADL (moving around indoors, performance of light housework, and getting in and out of a car). No significant differences between HAV group and control group in QOL at discharge or 2 months. |
|
Table III. Contd. |
|||||||
|
Study |
Country and setting |
Study design |
Participants |
Intervention |
Outcome measured |
Assessments used |
Key results |
|
Lannin et al., 2007 (2) |
Australia Inpatient rehabilitation (mixed) |
RCT |
n = 10 Age (years) = Exp 80 (SD 7), Comp 82.4 (SD 7) Female (%) = Exp 100, Comp 60 |
Exp = Pre-discharge HAV with OT, Comp = Standard practice in-hospital assessment and education with OT |
•Reintegration to community living •Mobility •Functional status •Fear of falling •Quality of life •No. of falls reported by participants •Hours and type of community support •No. of hospital readmissions |
RNLI (51) Tinetti POMA (52) FIM (39) NEADL (40) FES-I (53) EQ-5D (45) |
ADL scores were higher in the HAV group at 2 weeks (p = 0.012) and 2 months (p = 0.003). There were no other clinically significant differences between the groups. |
|
Luker & Grimmer-Somers, 2009 (31) |
Australia Acute inpatient (stroke) |
Retrospective medical record audit |
n = 50 Age (years) = 75 (SD 9.5) Female (%) = 34 |
Exp = Multidisciplinary coordinated care team and HAV with OT, Comp = Multidisciplinary coordinated care team |
•Staff compliance with discharge planning guidelines •Discharge destination •Support needs |
Patients who had HAV were 5.3 times more likely to avoid unpredicted support needs than patients who did not have HAV. Of the patients who received a HAV, 48% went directly home, 48% went to rehabilitation. |
|
|
Nikolaus & Bach, 2003 (23) |
Germany Acute inpatient (geriatric) |
RCT |
n = 360 Age (years) = Exp 81.2 ± 6.3 Comp 81.9 ± 6.5 Female (%) = Exp 72.4 Comp 74.3 |
Exp = CGA and HAV. Additional HAV after 3 months. Comp = CGA with recommendations. No HAV provided. |
•No. of falls •Type of recommended home modifications •Compliance with recommendations |
The HAV group had 31% fewer falls than the no HAV group (IRR = 0.69, 95% CI 0.51–0.97). The proportion of frequent fallers and the rate of falls was significantly reduced for the HAV group compared with the no HAV group (p = 0.009; IRR = 0.63, 95% CI = 0.43–0.94). |
|
|
Nygard et al., 2004 (28) |
Sweden Inpatient (geriatric) |
Qualitative interviews |
n = 23 Age (years) = 78 (range 68–86) Female % 82.6 |
Exp = Pre-discharge HAV and an additional HAV post-discharge, Comp = No comparison |
•Interventions provided on HAV •Patient satisfaction with process |
Patients were satisfied with the HAV but their perceptions and responses to problems differed from therapists. |
|
|
Pardessus et al., 2002 (30) |
France Acute inpatient (geriatric hospitalized for falls) |
RCT |
n = 60 Age (years) = Exp 83.5 ± 9.1 Comp 82.9 ± 6.3 Female (%) = Exp 76 Comp 80 |
Exp = Standard practice and pre-discharge HAV with OT and physical medicine and rehabilitation doctor, Comp = Standard practice including PT and home safety information |
•Functional status •No. of falls •Readmissions |
ADL Scale (54) IADL Scale (55) SMAF (56) |
Rate of falls, hospitalization for falls, institutionalisation, and death were not significantly different between HAV group and no HAV group. Both groups had a loss of autonomy at 12 months. |
|
Renforth et al., 2004 (32) |
England Inpatient (geriatric) |
Semi-structured interviews and chart audit |
n = 79 Age (years) 78.5 Female (%) 65.8 |
Exp = HAV with OT, Comp = No comparison |
•Functional status •Data on HAV length •Recommendations for services, equipment and adaptations |
PSM Scale (57) IADL Scale (55) |
91% were discharged to non-institutionalized settings (mainly their own home). 94% had some kind of equipment after the HAV. |
|
Table III. Contd. |
|||||||
|
Study |
Country and setting |
Study design |
Participants |
Intervention |
Outcome measured |
Assessments used |
Key results |
|
Rosenblatt et al., 1986 (22) |
USA Inpatient rehabilitation (hip fracture) |
Retrospective chart audit |
n = 40 Age (years) = 79.4 (range 65–96) Female (%) 90 |
Exp = Pre-discharge HAV with OT and PT Comp = No comparison |
•Outcome of HAV including discharge plans, discharge destination, and supports required |
93% of patients were discharged as planned and 7% were discharged following changes to the plan. After discharge all patients required formal support, with 3 requiring 24 h assistance. |
|
|
Whitaker & Hornby, 1986 (33) |
Scotland Acute inpatient (geriatric) |
Retrospective chart audit |
n = 59 Age (years) = 82.1 (range 66–96) Female (%) 73 |
Exp = HAV with OT, Comp = No comparison |
•Outcome of HAV including discharge plans, discharge destination, and supports required |
89% of patients were discharged home, 15% had a delayed discharge home. Aids were recommended for 63% of patients and other additional support arrangements were made in 80%. 11% were readmitted within 1 month. |
|
|
Exp: experimental; Comp: comparison; HAV: home assessment visit; OT: occupational therapy; ADL: activities of daily living; CGA: Comprehensive Geriatric Assessment; RCT: randomized controlled trial; IRR: incidence rate ratio; IADL: instrumental activities of daily living; PT: physiotherapy; FRASS: Falls Risk Assessment Scoring System; WHOQOL: World Health Organization Quality of Life; FIM: Functional Independence Measure; NEADL: Nottingham Extended Activities of Daily Living Scale; GHQ: General Health Questionnaire; SADQ: Stroke Aphasic Depression Questionnaire; RMI: Rivermead Mobility Index; CSI: Caregiver Strain Index; SWED-QUAL: Swedish Health-Related Quality of Life Survey; RNLI: Return to Normal Living Index; POMA: Performance-oriented Mobility Assessment; FES-I: Falls Efficacy Scale – International; SMAF: Functional Autonomy Measurement System; PSM: Physical Self-maintenance. |
|||||||
Synthesis of results
Effect of pre-discharge home assessment visit vs no home assessment visit on risk of falling. Meta-analysis of 5 studies with a total of 862 participants provided moderate quality evidence that patients from geriatric, neurological and mixed rehabilitation settings were 32% less likely to fall when they received a home assessment visit prior to discharge from hospital than when they did not receive a home assessment visit (RR 0.68, 95% CI 0.49–0.94; I2 = 28%) (Fig. 2, Table IV).
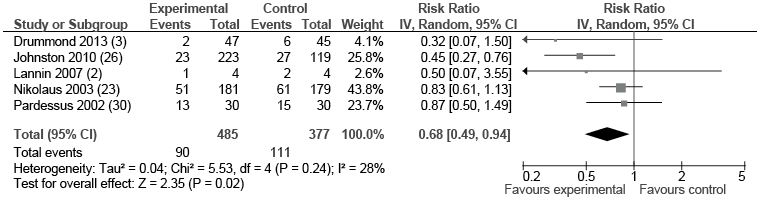
One study by Nikolaus & Bach (23) included in the meta-analysis found that home assessment visits prior to discharge from hospital were particularly effective in those with a history of 2 or more falls, where a 37% lower fall rate was reported for those receiving a home assessment visit (incidence rate ratio (IRR) = 0.63; 95% CI 0.43–0.94, p = 0.028). They also reported that participants who made at least one recommended change as a result of the home assessment visit experienced a significant reduction in falls (IRR = 0.64; 95% CI 0.37–0.99, p = 0.047); however, the number of falls in the home assessment visit group was not significantly different from the control group when no home modifications had been implemented (IRR = 1.05; 95% CI 0.82–0.141). The study by Barras (25) included in the meta-analysis reported that falls risk was reduced by a home assessment visit in all diagnostic groups, except neurological (25, 26). The magnitude of the risk ranged from 3.9 times higher for cardiac, spinal and de-conditioned patients to 8 times more likely to fall for orthopaedic trauma patients who did not receive a home assessment visit.
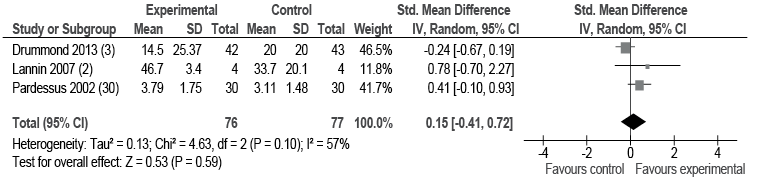
Effect of pre-discharge home assessment visit vs no home assessment visit on activity and participation. Meta-analysis of 3 studies with 153 participants from geriatric, neurological and mixed rehabilitation settings provided low-quality evidence that receiving a home assessment visit did not show any effect on measures of activity compared with not receiving a home assessment visit (SMD 0.15; 95% CI –0.41–0.72; I2 = 57%) (Fig. 3, Table IV). However, there was a moderate degree of heterogeneity in the data. The study by Drummond et al. (3) focussed on patients with a diagnosis of stroke. When this study was removed from the meta-analysis in a sensitivity analysis, I2 reduced to 0% and there remained no evidence of effect on measures of activity.
|
Table IV. Quality of evidence of studies comparing pre-discharge home assessment visit with no home assessment visit |
||||
|
Outcome |
No. of trials (ref) |
No. of participants |
SMD or RR (95% CI), I2 |
Quality of the evidence (GRADE) |
|
Risk of falling |
5 (2, 3, 23, 26, 30) |
862 |
RR 0.68 (0.49, 0.94), 28% |
Moderatea |
|
Activity |
3 (2, 3, 30) |
153 |
SMD 0.15 (–0.41, 0.72), 57% |
Lowb |
|
Participation |
2 (2, 30) |
68 |
SMD 0.49 (0.01, 0.98), 0% |
Lowc |
|
Quality of life |
3 (2, 3, 25) |
474 |
SMD 0.08 (–0.12, 0.27), 0% |
High |
|
Risk of re-admission |
4 (2, 3, 25, 30) |
563 |
RR 0.75 (0.31–1.82), 63% |
Lowd |
|
aReason for downgrade: large confidence interval. bReason for downgrade: large confidence interval, statistical heterogeneity. cReason for downgrade: large confidence interval, inconsistent results. dReason for downgrade: large confidence interval, statistical heterogeneity. GRADE: Grading of Recommendations Assessment, Development and Evaluation; SMD: standardized mean difference; CI: confidence interval; RR: risk ratio. |
||||
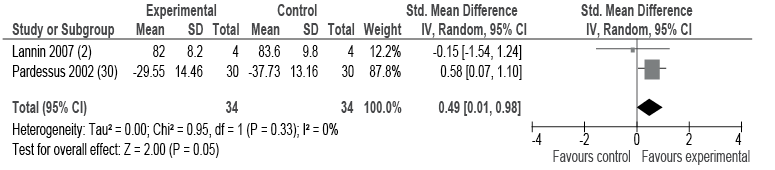
Meta-analysis of 2 studies with a total of 68 participants from geriatric and mixed rehabilitation settings provided low-quality evidence that home assessment visits resulted in a moderate, but significant, effect on participation (SMD 0.49; 95% CI 0.01–0.98, I2 = 0%) (Fig. 4, Table IV).
Additional studies reported activity data, but did not include sufficient data to be included in the meta-analysis (2, 3, 24, 25). Hagsten et al. (24) reported statistically significant improvements in self-reported instrumental activities of daily living (moving around indoors, performance of light housework, and getting in and out of the car) in patients following hip fracture who received training with an occupational therapist and a home assessment visit compared with those who did not. Barras (25) reported that patients who received a home assessment visit prior to discharge were less likely to have deterioration in Functional Independence Measure scores after discharge (odds ratio (OR) 0.4; 95% CI 0.3–0.7). In qualitative data, Barras (25) asked patients to identify additional areas on the home assessment visit that would have contributed to a smoother transition from hospital to home. Primarily the areas identified were external to the home and focused on being able to function in their environment and the community. Two studies measured mobility and found no difference between those receiving a home assessment visit and those who did not receive a home assessment visit (2, 3).
Effect of home assessment visit vs no home assessment visit on quality of life. Meta-analysis of 3 studies with a total of 474 participants from neurological and mixed rehabilitation settings provided high-quality evidence that receiving a home assessment visit did not show any difference in quality of life compared with not receiving a home assessment visit (SMD 0.08; 95% CI –0.12–0.27; I2 = 0%) (Fig. 5, Table IV).
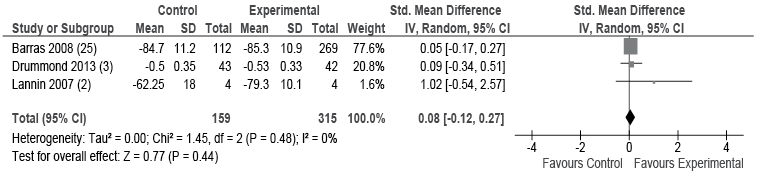
One of these studies (25) reported that the completion of a home assessment visit positively affected the environment domain within the quality of life assessment. This domain measures issues routinely assessed during a home assessment visit, including physical safety and security, the physical environment of the home, patient financial resources, opportunities for recreation/leisure activities, and accessibility of transportation.
An RCT (24) could not be included in the meta-analysis because an overall mean and standard deviation were not available given the outcome measure used. The results were consistent with the meta-analysis, showing no difference in quality of life in a group of patients post hip fracture receiving a pre-discharge home assessment visit and individualized occupational therapy training compared with those who did not receive a home assessment visit.
Effect of pre-discharge home assessment visit vs no home assessment visit on discharge, re-admission and support needs at home. Meta-analysis of 4 studies of participants from geriatric, neurological and mixed rehabilitation settings provided low-quality evidence that receiving a home assessment visit did not show any difference in risk of readmission to hospital between the group that received a home assessment visit and the group that did not (RR 0.75; 95% CI 0.31–1.82; I2 = 63%) (Fig. 6, Table IV). However, there was a moderate degree of heterogeneity in the data. The study by Drummond et al. (3) focussed on patients with a diagnosis of stroke. When the one study focussing on stroke was removed from the meta-analysis in a sensitivity analysis, I² reduced to 0% and suggested that patients were 50% less likely to be re-admitted to hospital if they received a home assessment visit compared with those who did not receive a home assessment visit (RR 0.47, 95% CI 0.33–0.66).
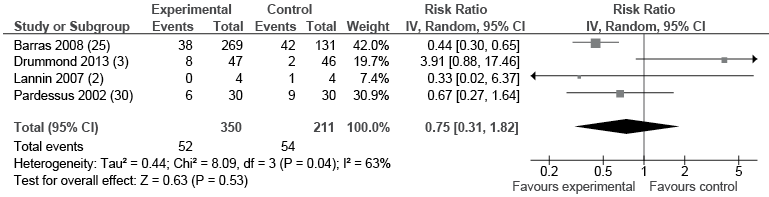
Four observational studies that could not be included in the meta-analysis used discharge destination as an outcome and reported 89–93% of patients were discharged home following a home assessment visit (22, 31–33). Luker & Grimmer-Somers (31) reported that providing a home assessment visit was significantly related to discharge directly home from hospital (OR 28.5; 95% CI 4.5–237.6). The authors also reported that patients who had received a home assessment visit were 5 times more likely to avoid unpredicted support needs than patients who had not received a home assessment visit (OR 5.3; 95% CI 0.8–39.8).
Patient and carer perception of effectiveness of pre-discharge home assessment visits. Five studies reported on patient and carer perceptions of the effectiveness of home assessment visits. Three factors emerged that impacted on the effectiveness of pre-discharge home assessment visits from a patient and carer perspective: satisfaction with the process; the purpose of the visit; and the incorporation of patient and carer opinions in the decision-making process. Patients were generally satisfied with the home assessment visit (25, 28, 29, 35). Barras (25) reported that 84% of patients who received a home assessment visit reported it as a positive experience that was a necessary part of their safe discharge. Atwal et al. (29) reported that although carers found the home visit process helped to eradicate anxiety some older adults were apprehensive. Similar levels of anxiety were also reported amongst other patients (34). Patients, carers and occupational therapists may not view the purpose of a home assessment visit in the same way, resulting in the expectations of patients and carers not always being fully met (28, 34, 35). Clark & Dyer (34) concluded that safe discharge rather than enhancing independence dictated the home visit process. There was little evidence that occupational therapists asked patients about their usual way of performing daily occupations and they also did not consider the wider implications of their decision-making for patients and carers, both in relation to community or social activity and interpersonal interaction or relationships (28, 29, 34). Atwal et al. (29) were able to identify specific instances where not being listened to had consequences for the type of occupations that were being performed. This was also highlighted by Clark & Dyer (34), who suggested that the process enabled patients to live safely within the home, but did not equip them to live their lives as they wished.
Discussion
This systematic review of 14 studies provides evidence that home assessment visits conducted prior to discharge from hospital reduce the risk of falling and increase participation levels in patients from geriatric and rehabilitation settings. The risk of readmission to hospital may also be reduced in these patients, but not for patients following stroke. Receiving a home assessment visit did not demonstrate a benefit on activity or quality of life.
The results of this review suggest that a pre-discharge home assessment visit can deliver clinically important outcomes. Receiving a home assessment visit can significantly reduce a patient’s risk of falling and appears to be particularly effective in patients with a history of falls. This is consistent with a review assessing the effectiveness of interventions for preventing falls in community-dwelling older people, which found that home safety interventions led by occupational therapists reduce the risk of falling (36). There is also evidence to suggest that the risk of readmission to hospital may be reduced, at least in some patient groups, by completion of a home assessment visit. The findings contrast those of a large review of 64 studies by Mayo-Wilson et al. (4), which found no evidence for the effectiveness of home visiting programmes conducted in the community by a variety of different health professionals. However, the patients in that review were not hospitalized, suggesting that their health status and the nature and purpose of the home visits were quite different to those included in the current review.
Further research is needed to clarify the contribution of home assessment visits in reducing the risks of falling and readmission for particular patient groups given the contrasting findings for patients with orthopaedic conditions compared with those following stroke (3, 25). The reason for this difference is not clear, but it is possible that patients with neurological impairments fall due to intrinsic factors that are less preventable through interventions targeting environmental factors. Another possible explanation is that this group of patients receive more therapy input in general than other patient groups, and so the home assessment visit in isolation has less of a contribution to make to their transition home.
It is important to understand the impact of home assessment visits on patients’ functioning in day to day life once they are discharged from hospital. Receiving a home assessment visit does not seem to reduce activity limitations, but does seem to contribute to improved participation. This result is not unexpected, given that home assessment visit interventions focus predominantly on environmental modification, provision of equipment or recommendations for community supports. Measures of participation take into account the resources that a person has in their current environment to enable them to participate in everyday life.
The inclusion of qualitative studies within this review provided valuable information regarding the patient and carer perspective of the effectiveness of home assessment visits. This review is consistent with the conclusions of Atwal et al. (8) and the qualitative studies contribute to an understanding about the process of the home assessment visit, but there remains only a limited body of research that has been conducted in the area. One consistent theme throughout the qualitative studies was that there was little evidence that patients’ needs, concerns and opinions were integral to the home assessment process. The evidence from this review suggests that home assessment visits are currently completed with a short-term view of recovery and safe discharge and not for the purpose of enhancing independence longer term. The patient and carer perspective of home assessment visits suggests that how the visits are completed may have an impact on the outcomes and the effectiveness for patients. It is possible that the effectiveness in relation to patient outcomes, such as activity, participation and quality of life, may be influenced by the process of the home assessment visit. The qualitative research suggests that consultation and participation need to drive the interaction between patients and clinicians involved in discharge planning. It is possible that better integration of patients’ needs and individual coping strategies and the recommendations from the home assessment visits may lead to better outcomes.
The description of the content of the home assessment visit was provided in the studies with varying levels of detail. Nonetheless, the descriptions provided suggest that the home assessment process was similar across studies. The length of follow-up varied considerably between the studies, perhaps suggesting some uncertainty about how long the intervention is likely to be effective. There were also a large number of different outcomes reported and the tools used to measure them were diverse. A number of observational studies of lower methodological quality reported discharge destination as an outcome, suggesting that the number of patients discharged home is an indicator of a successful home assessment visit. However, in clinical practice a decision to delay or prevent discharge home because a patient is unsafe or not ready could also be considered a successful outcome of a home assessment visit.
This review is limited by the quality of the available evidence, with only 5 randomized controlled trials. The studies had relatively small sample sizes, and many had insufficient power to find statistically significant effects. Only one RCT had more than 50 participants in each allocation arm (23). Only 5 studies were able to be used in the meta-analyses (2, 3, 23, 25, 30). The review included diverse conditions and settings, which could be viewed as a limitation, although consideration was given to the clinical homogeneity within the studies included in the meta-analyses and the more conservative random effects model was used for analysis. A number of the meta-analyses demonstrated statistical heterogeneity. A factor contributing to this heterogeneity may have been the synthesis of different outcome measures that measured similar constructs. However, to account for this sensitivity analyses were conducted as appropriate and the GRADE approach was applied, which determines the level of confidence in the results for clinicians and other stakeholders.
In conclusion, this systematic review provides moderate quality evidence that home assessment visits conducted prior to discharge from hospital reduce patients’ risk of falling. There is low-quality evidence that conducting a home assessment visit may result in increased levels of participation and may reduce the risk of readmission to hospital for geriatric and mixed rehabilitation patient groups. This review provided evidence that conducting pre-discharge home assessment visits produces clinically important outcomes, but more research is required to clarify which patient groups benefit most from receiving home assessment visits.
References
