Joep B. Ponten, MD1, Egbert Krug, MD1, Laurens J. van Baardewijk, MD1, Enrike (H.) M. J. van der Linden, MD, PhD2, Reneé Haas, MD3, Pieta Krijnen, PhD1 and Inger B. Schipper MD, PhD1
From the Departments of 1Surgery-Traumatology and 2Orthopaedics, Leiden University Medical Center and 3Topaz Foundation, Leiden, The Netherlands
OBJECTIVE: To gather preliminary data on the effectiveness of intensive rehabilitation after hip fracture surgery, as provided in the Transfer Unit (TU) in Leiden, The Netherlands, compared with the effectiveness of rehabilitation in a regular nursing home. Intensive rehabilitation in the TU consists of physical therapy twice daily by dedicated medical staff and aims to shorten hospital stay and duration of rehabilitation, in order to increase the hospital admission capacity and reduce waiting lists for nursing homes.
DESIGN: Retrospective cohort study.
Patients: A total of 173 hip fracture patients, selected postoperatively for intensive rehabilitation in the TU. Of these, 156 received TU rehabilitation (TU+ group), while 17 were rehabilitated in regular nursing homes for logistic reasons (TU– group).
METHODS: Length of hospital stay, rehabilitation duration and survival were compared between TU+ and TU–.
RESULTS: Both groups appeared comparable at baseline. TU+ patients had a mean hospital stay of 10.4 vs 12.3 days for TU– patients (p = 0.29), while their rehabilitation duration was 25.2 days shorter: 42.0 vs 67.2 days (p = 0.001). One-year survival was similar (87%).
CONCLUSION: Intensive rehabilitation in selected hip fracture patients may reduce rehabilitation duration by almost 4 weeks. Differentiated aftercare appears to increase care efficiency for hip fracture patients in both hospitals and nursing homes and may result in a significant reduction in costs.
Key words: hip fracture; rehabilitation; patient selection; length of stay; survival.
J Rehabil Med 2015; 47: 00–00
Correspondence address: Pieta Krijnen, Department of Surgery-Traumatology, Leiden University Medical Center, Albinusdreef 2, NL-2300 RC Leiden, The Netherlands. E-mail: P.Krijnen@lumc.nl
Accepted Sep 15, 2014; Epub ahead of print Dec 11, 2014
INTRODUCTION
Hip fractures are common and are associated with high mortality (1). Due to ageing populations worldwide, treatment and care put a significant financial strain on healthcare systems (2–4) as a result of the often long duration of hospitalization and rehabilitation (5–6). This challenge can be addressed with a comprehensive approach that shortens both the length of hospital stay and the duration of rehabilitation, while safeguarding the quality of care (7).
In the Netherlands hip fracture patients who cannot return home after surgery and inpatient rehabilitation, are temporarily admitted to regular nursing homes for outpatient rehabilitation before returning home. In the regular nursing homes they share the facilities with permanent residents. The rehabilitation provided is not entirely tailored to their specific needs, which may lead to longer stays than necessary, waiting lists for nursing home admission and, consequently, to lengthier hospital stays than clinically required. This may negatively influence the patient’s outcome and may be an inefficient way of utilizing the limited resources for outpatient rehabilitation.
In 2006, the Surgical and Orthopaedic departments of the Leiden University Medical Center (LUMC) initiated a collaboration with Topaz, a geriatric and rehabilitative care provider with 998 beds. This project was called the Transfer Unit (TU). The TU comprises 18 beds in one of the local Topaz nursing homes, reserved exclusively for LUMC patients. Hip fracture patients form the largest group within the TU. Care in the TU is characterized by intensive physical therapy provided by dedicated medical staff and tailored to the patients’ needs (see Methods for a detailed description). The main goal of rehabilitation in the TU is to facilitate the swift recovery of patient’s functional status and to ensure their safe discharge home.
The purpose of this study was retrospectively to evaluate the effectiveness of intensive rehabilitation in the TU following hip fracture surgery in terms of length of hospital stay, duration of rehabilitation and mortality; and thus provide preliminary data in support of this approach.
METHODS
Patients
All patients ≥ 18 years with a proximal femoral fracture, who had not sustained a previous fracture of the same joint and who were surgically treated in the LUMC between January 2007 and January 2011, were identified. Surgery was performed either in the Department of Trauma Surgery or in the Department of Orthopaedics, with identical operative procedures.
After surgery, a multidisciplinary team consisting of the surgeon, nursing staff, social worker and physical therapist determined which discharge destination they considered the most suitable for each patient based on a clinical evaluation of the patients’ physical and cognitive functioning. If decreased cognitive function was suspected, the Mini-Mental State Examination (MMSE) was scored. Objective criteria for selecting specific discharge destinations for individual patients were not defined, but age, comorbidity and domestic situation (mobility, level of independence and social network) were considered important criteria. Patients were discharged to one of the following destinations: home; the TU for intensive rehabilitation; a regular nursing home for standard rehabilitation; or to stay permanently in a nursing home or other institution.
In this study, only patients who were deemed clinically suitable for intensive rehabilitation in the TU were included. Two subgroups of patients were distinguished: those who were admitted to the TU (TU+ group) and those who were admitted to a regular nursing home despite their selection for the TU (TU– group). The latter situation could occur as a result of TU capacity overload, or because the patient preferred to be admitted to a facility closer to their residence, but not for medical reasons.
Rehabilitation
Rehabilitation in regular nursing homes is not standardized, but comprises a maximum of 5 training sessions per week. In contrast, intensive rehabilitation in the TU consists of physical therapy twice daily. Patients with similar hip pathology are admitted to the same ward, as it is assumed this has a positive effect on recovery. Care is provided by dedicated medical staff, discharge is planned at the moment of admission, and the patients’ progress is monitored by a multidisciplinary team consisting of medical and nursing staff, a physical therapist, social worker, dietician and occupational therapist.
Outcomes and other data
Length of hospital stay and duration of rehabilitation were retrieved from the medical records of the hospital and nursing homes, together with data concerning cause and type of fracture, morbidity, surgery, complications and other patient characteristics. Data on vital status after follow-up were obtained from the Digital Hospital Information System, which is linked to the municipal administrative databases that contain all dates of death of registered citizens in the Netherlands.
Statistical analysis
Comparisons between the TU+ and TU– groups were made using the χ2 test for categorical data and the unpaired Student’s t-test for continuous data. Hospital length of stay, duration of rehabilitation and survival were compared using the Student’s t-test and Cox proportional hazards analysis. In the analysis of rehabilitation duration, patients who did not complete the rehabilitation programme were censored if and when they were readmitted to the hospital, were permanently admitted to a nursing home, or died during rehabilitation.
RESULTS
Study population
Between January 2007 and January 2011, 173 hip fracture patients were deemed to require rehabilitation and were assessed by the multidisciplinary team to be physically and mentally fit for intensive rehabilitation in the TU.
Patients selected for the TU
Of the 173 patients selected for TU intensive rehabilitation, 156 received intensive rehabilitation in the TU (TU+ group). The other 17 patients (TU– group) rehabilitated in a regular nursing home instead of in the TU because there was no bed available in the TU (n = 9) or because the patient preferred to stay in a nursing facility closer to their residence (n = 8). Patient characteristics did not differ between the TU+ and TU– groups (Table I). Also, there was no difference between these groups in terms of type of surgery performed and postoperative complications, such as wound infection, delirium or pulmonary, cardiac, neurological or thromboembolic complications (data not shown). One-year survival rates were 87% for the 156 TU+ patients (1 missing) and 88% for the 17 TU– patients.
|
Table I. Characteristics of 173 patients selected for intensive rehabilitation after discharge from the Leiden University Medical Center |
|||
|
Characteristic |
TU+ group (n = 156) |
TU– group (n = 17) |
p-value |
|
Age, years, mean (SD) |
78.0 (10.7) |
81.6 (8.6) |
0.19 |
|
Female, n (%) |
117 (75.0) |
15 (88.2) |
0.22 |
|
Living independently prior to fracture, n (%) |
138 (89) |
16 (94) |
0.70 |
|
Walking without aid prior to fracture, n (%) |
53/138 (38) |
8/14 (57) |
0.17 |
|
Fracture type, n (%) |
0.55 |
||
|
Femoral neck |
85 (54.5) |
12 (70.6) |
|
|
Pertrochanteric |
60 (38.4) |
5 (29.4) |
|
|
Subtrochanteric |
7 (4.5) |
0 |
|
|
Unknown |
4 (2.6) |
0 |
|
|
ASA, n (%) |
0.87 |
||
|
I |
18 (11.5) |
3 (17.6) |
|
|
II |
89 (57.1) |
10 (58.8) |
|
|
III |
43 (27.6) |
4 (23.5) |
|
|
IV |
2 (1.3) |
0 |
|
|
Unknown |
4 (2.6) |
0 |
|
|
Comorbidity, n (%) |
|||
|
Cardiac |
57 (36.5) |
9 (52.9) |
0.14 |
|
Pulmonary |
27 (17.3) |
1 (5.9) |
0.24 |
|
Diabetes |
24 (15.4) |
3 (17.6) |
0.75 |
|
Neurological |
53 (34.0) |
3 (17.6) |
0.20 |
|
Conditions affecting the lower extremitiesa |
61 (39.1) |
10 (58.8) |
0.08 |
|
Malignancy |
22 (14.1) |
1 (5.9) |
0.36 |
|
Other |
12 (7.7) |
1 (5.9) |
0.82 |
|
aIncluding previous fracture, arthrosis, rheumatic disease, and joint replacement. TU+: intensive rehabilitation in Transfer Unit; TU–: rehabilitation in regular nursing home; ASA: American Society of Anaesthesiologists physical status classification system; SD: standard deviation. |
|||
Length of stay
Length of hospital stay did not differ between the TU+ and TU– groups: 10.4 vs 12.3 days (p = 0.29). In the TU+ group 139 patients completed their rehabilitation and returned to their home situation. The remaining 17 patients did not complete their rehabilitation: 3 died during their stay in the TU, 5 were permanently admitted to a nursing home, and 9 were readmitted to the hospital. One patient in the TU– group did not return home and died in the nursing home. Deceased patients were included in all analyses.
The mean duration of rehabilitation in the TU+ group was 42.0 days (standard deviation (SD) 26.9) compared with 67.2 days (SD 43.0) in the TU– group (p = 0.001). The mean difference was 25.2 days (95% confidence interval (95% CI) 10.7–39.4). In the Kaplan–Meier analysis, the TU+ patients were discharged home after rehabilitation earlier than the TU– patients (hazard ratio 1.79, 95% CI 1.06–3.03; likelihood ratio test, p = 0.02; Fig. 1).
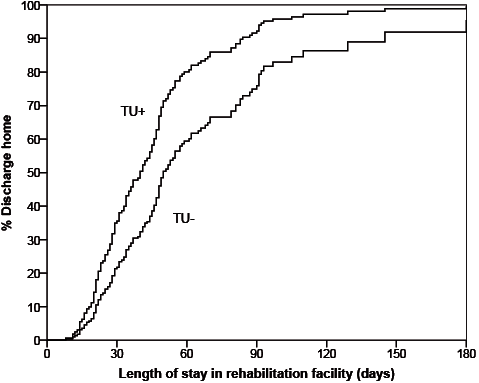
Fig. 1. Length of stay in rehabilitation facility until discharge to home in patients selected for intensive rehabilitation. TU+: intensive rehabilitation in Transfer Unit; TU–: rehabilitation in regular nursing home.
DISCUSSION
This study aimed to provide preliminary data concerning the comparative effectiveness of intensive rehabilitation after hospital admission for hip fracture surgery in selected patients. In the group of patients that underwent this intensive rehabilitation at the TU, rehabilitation was almost 4 weeks shorter compared with similar patients who were rehabilitated in regular nursing homes. The length of hospital stay was the same for both groups and the 1-year survival rate was not adversely affected by the intensive rehabilitation. Widespread implementation of differentiated aftercare for hip fracture patients may lead to a reduction in waiting lists and a significant cost reduction, through enhanced rehabilitation and early return to home.
Rehabilitation in the TU was performed according to a standardized protocol, comprising individual and group physical therapy twice daily for 5 days a week. The intensive rehabilitation involves early and frequent ambulation and mobilization that benefits patients who are physically and mentally fit for this type of care. The aim is to accelerate recovery, stimulate independence, and thus to enable the patients to return home sooner. Previous studies have also shown that frequent and protocol-driven physical therapy leads to a swifter recovery (8–10). The fact that a multidisciplinary rehabilitative approach was used in the TU setting may have contributed to its success (11). The approach described in the present study distinguishes itself from other rehabilitation programmes. The aftercare was patient-tailored, instead of providing a similar rehabilitation programme to all hip fracture patients. It has been stated that, especially in hip fracture patients, patient characteristics should be well acknowledged because they play a vital role in the rehabilitation process (12).
Study limitations
In addition to the fact that the sample size for the control group (TU–) was small, rendering many of the comparisons around patient ‘baseline’ characteristics such as comorbidities inconclusive, retrospective cohort studies such as the present one face several additional methodological challenges and limitations.
Firstly, the 2 groups were not randomly selected, thus selection bias may contribute to the observed differences between the TU groups. However, no gross differences were found in baseline characteristics, such as age, comorbidity and surgery performed, indicating that selection bias may not be contributing to the observed differences in the measured outcomes. Both groups were actually enrolled in the TU programme. TU– patients were rehabilitated elsewhere solely due to logistic problems, and not because of their vitality, which we presumed to be similar in both groups based on the simple fact that all patients were deemed suitable for intensified rehabilitation as provided in the TU. A multidisciplinary team made a qualitative assessment based on implicit, non-quantified criteria, and cognitive and motoric abilities. All patients were assessed to have adequate cognitive function to complete the rehabilitation programme. The criteria for assessing whether a patient was clinically suitable for intensive rehabilitation also included the patient’s age, comorbidity and level of independence, although more recent evidence suggests that these should not be used as criteria for intensive rehabilitation (13).
Secondly, no valid data were available from the period before the implementation of the TU, since the detailed documentation of hip fracture patient data began simultaneously with implementation of the TU project. Consequently, comparing the length of hospital stay before and after introduction of the TU aftercare project was not possible.
Finally, no information regarding quality of life was available for evaluation. This would have been helpful to assess the outcome after rehabilitation in detail. In spite of the limitations mentioned above, we believe that the results are representative and applicable to other Dutch, and possibly international, populations.
Conclusion
Intensive rehabilitation after hip fracture surgery for patients who are deemed sufficiently fit, is likely to reduce the total length of stay compared with similar patients who receive regular postoperative rehabilitation. On average, the difference was almost 4 weeks, mainly due to a shorter rehabilitation period, whereas survival was not adversely affected. Differentiated aftercare may benefit all hip fracture patients, since relatively fit patients could return to their domestic situation sooner, while relatively less fit patients would benefit from shorter waiting lists for nursing homes. Nationwide, and even international, implementation of similar clinical pathways for hip fractures can relieve the financial burden that this condition puts on healthcare systems. More research is needed to confirm the trends observed in this study as well as the effects of intensive rehabilitation on quality of life.
REFERENCES
