Birgit Prodinger, PhD1,2, Mwidimi Ndosi, PhD3, Ulla Nordenskiöld, PhD4, Tanja Stamm, PhD1, Gert Persson5, Ingrid Andreasson, MSc6 and Åsa Lundgren-Nilsson, PhD4
From the 1Department of Rheumatology, Medical University of Vienna, Vienna, Austria, 2Swiss Paraplegic Research, ICF Unit, Nottwil, Switzerland, 3Academic and Clinical Unit for Musculoskeletal Nursing (ACUMeN), Section of Clinical Biomechanics and Physical Medicine, Leeds Institute of Rheumatic and Musculoskeletal Medicine, University of Leeds, Leeds, UK, 4The Sahlgrenska Academy, University of Gothenburg, 5Patient Research Partner and 6Sahlgrenska University Hospital, Gothenburg, Sweden
OBJECTIVE: To explore patients’ and health professionals’ views of outpatient rehabilitation services for patients with rheumatoid arthritis in 3 different rheumatology sites across Europe.
METHODS: A qualitative multi-method study was conducted with patients and health professionals in Vienna (Austria), Gothenburg (Sweden) and Leeds (UK). Data collection was carried out during focus groups with patients and health professionals. Patients’ hospital records were integrated into the analysis. Data were analysed for site and findings were compared across sites.
RESULTS: A total of 20 patients and 20 health professionals participated in 12 focus groups. Although the 3 sites were all publicly funded university clinics, there were differences between sites regarding the structure and content of rehabilitation services. The themes that emerged in the focus groups were: referrals; continuity in rehabilitation; information provided to patients; patients’ organizations; documentation and communication amongst health professionals; interface between primary and specialist care; and prescription practices. Most themes were addressed at all 3 sites, but there were variations in the specifics within themes.
CONCLUSION: Integration of patients’ and health professionals’ views on how rehabilitation services are coordinated and how (parts of) processes are set up elsewhere provide valuable information for the further optimization of rehabilitation services.
Key words: delivery of healthcare; rehabilitation; interdisciplinary communication; patient perspective; multi-centre study.
J Rehabil Med 2015; 47: 00–00
Correspondence address: Birgit Prodinger, Swiss Paraplegic Research, Guido A. Zäch Institute, CH-6207 Nottwil, Switzerland. E-mail: birgit.prodinger@paraplegie.ch
Accepted Sep 10, 2014; Epub ahead of print Nov 6, 2014
INTRODUCTION
Rheumatoid arthritis (RA) is a chronic, systemic inflammatory disease that affects a person’s body structures and functions and interacts with the activities in which he or she engages. A person’s functioning is also influenced by the contextual factors that describe the background of their life (1, 2). While there is no cure for RA, there are various treatment options to maintain or improve the functioning of individuals. The aim of maintaining or improving functioning of individuals has been referred to as rehabilitation strategy (3). Services that embody a rehabilitation strategy as their primary goal are referred to as rehabilitation services and can be provided in any organizational setting (4). Rehabilitation services provided to people with RA occur predominantly in a multidisciplinary setting (5, 6).
Differences in service provision for RA are evident across Europe. A survey of health professionals’ (HPs) roles across Europe identified differences in the responsibilities assigned to HPs. For instance, HPs in Sweden and the UK can admit patients to a ward, or manage patient telephone advice lines, neither of which are the case in Austria (7). For people with RA, differences across Europe have been described with reference to accessing biological therapies (referred to as “biologicals”). Biologicals are an expensive newer class of drugs that interfere in the biological processes within the immune system to lessen inflammation. Reasons for country differences related to accessing biologicals include the country’s total health expenditure, as well as variations in content and application of guidelines (8). Emery et al. (9) reviewed guidelines from several European countries and found differences in various aspects, including the definition of the disease activity level required for initiation of treatment with biologicals, and the time to response.
Differences in the views of patients and health professionals of the processes and outcomes of treatment have also been described previously. In a survey with patients and rheumatologists Van Hulst et al. (10) identified factors that are important in the care of people with RA. Only 2 out of 58 factors were ranked by patients and HPs, respectively, within the top 10; namely physical functioning and mobility (which was ranked 1st by patients and 7th by rheumatologists), and impression of overall disease activity (ranked 3rd by rheumatologists and 8th by patients). Integration of the patients’ perspectives into the provision of rehabilitation services for people with RA has been advocated in order to ensure the most appropriate development and delivery of rehabilitation services (11–14).
Thus, we have some insight into differences at the country level and at the level of the patient-provider interaction. However, there is a paucity of knowledge about how rehabilitation services are actually set up at different sites across countries from the perspective of patients and HPs. The main objective of this study was therefore to explore, from the perspective of patients and HPs, how outpatient rehabilitation services for patients with RA are set up in 3 different rheumatology sites across Europe. More specifically, the aims were:
• to reconstruct the institutional processes of a routine visit to a rheumatology site that provides rehabilitation services from the perspective of patients and HPs, and
• to identify similarities and differences between these processes across sites.
METHODS
A qualitative multi-method study was conducted in Vienna (Austria; AUT), Gothenburg (Sweden; SE), and Leeds (United Kingdom; UK). These countries were chosen as they are embedded within different social and health systems (15).
The study design is illustrated in Fig. 1.
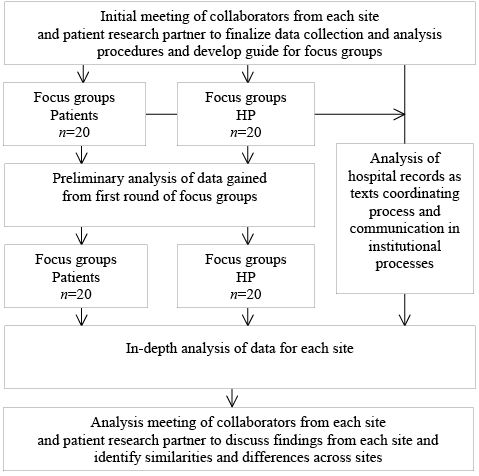
Fig. 1. Overview of study design. HP: health professionals.
Participants
Patients and HPs participated in this study. The patients were recruited from the outpatient departments of the participating sites. Inclusion criteria were: a definite diagnosis of RA (16); attendance at the clinic at the participating site for at least 1 year, thus being familiar with the institutional processes there. Sampling of patients in each country followed a maximum variation strategy based on age, sex, disease duration, and employment status (17). Patients who fulfilled the inclusion criteria were informed about the study and asked about their interest in participation by a study nurse or other HP at each site. If they were interested in the study, they were asked to contact the responsible local researcher responsible (BP, IA, MN).
HPs who had worked at the respective sites for at least one year were also invited to join focus groups, with maximum variation regarding their professional background. HPs were provided with information about the study by a local researcher (BP, IA, MN) who, at that point, was not involved in clinical practice at the respective site.
In order to accommodate individual opinion within the group the group sizes were set at a maximum of 7 people (18). In line with qualitative research, the aim was to obtain data of sufficient depth and breadth to allow a comprehensive understanding of the context in which rehabilitation is provided (19).
The study was approved by the institutional review boards and ethics committees of the participating centres. All participants provided written informed consent.
Data collection
Multiple methods were used for data collection: focus groups with patients and HPs, respectively, and analysis of the hospital records of the patients who participated in the focus groups.
Focus groups. Two consecutive focus groups were conducted with patients and HPs to explore a routine visit to the outpatient setting at the rheumatology clinic at which rehabilitation services are provided for patients with RA. A short introduction to the study was given at the first focus group, for patients and HPs alike. The main question was to describe how a routine visit to the rheumatology clinic proceeds once a patient has entered the clinic and who is involved. As routine visits usually take place in the outpatient wards, these received particular attention in the focus groups. In the second round of focus groups, participants from the first focus groups were invited again. Following a presentation by the moderator about the preliminary findings from the first focus group, participants were asked to comment on, clarify and complement the emerging findings. All focus groups were tape-recorded and transcribed verbatim.
Hospital records. In a previous analysis, hospital records were revealed as an intermediary between the patients and institutional processes (20, 21). The hospital records of those patients who participated in the focus groups were analysed with regard to the records’ role in the institutional processes, how information was entered into the records (e.g. electronically or on paper), and which HPs had access to and could add patients’ information to the hospital records. It is noteworthy that the purpose of including hospital records in this analysis was not to gain information on the content captured within the hospital records, but rather to gain a more comprehensive picture of the institutional processes in which hospital records have an intermediary role.
Data analysis
Conceptual framework for analysis. The social theory informing institutional ethnography guided the analysis to reconstruct institutional processes (22–25). Institutional ethnography is a conceptual framework for inquiry that facilitates exploration of how mundane aspects of daily life, such as a visit to the rheumatology clinic, become accomplished through coordinated activities of people (25, 26). The starting point of inquiry is the standpoint of individuals’ lives from which their activities are traced and examined as they are interacting with the activities of other people elsewhere in the institutional processes. For this study the starting point was the individual patient with RA on a routine visit to the rheumatology department. Based on the data from the focus groups about how a routine visit proceeds, the patients’ activities throughout a routine visit were traced. Particular attention was paid to the interaction of patients with various professionals. Texts have a mediating character in such processes (27). Hospital records were included in this study in order to gain a more comprehensive understanding of the institutional processes at each site. For instance, if a referral was issued, it was tracked in order to understand the communication flow between HPs, and how this flow coordinates the activities of various HPs and the patient.
Data were analysed first for each site and subsequently compared across sites. In the first step of analysis, data was read inductively in order to gain an understanding of what is happening throughout a routine visit, who is involved, and how people interact with each other. In the second step, the findings from each site were compared across sites. Therefore, the research team met to discuss the findings from each site and subsequently derive themes about similarities and differences across sites.
Trustworthiness of analysis. The local principal investigators (MN, ALN, BP) had experience with qualitative, as well as multi-site and cross-cultural research before this project. All focus groups were chaired by a trained and experienced moderator and an assistant. The moderators were all familiar with the study protocol. Method triangulation was applied, using focus groups with patients and HPs, respectively, and hospital records, to enhance the trustworthiness of the findings. The preliminary findings of the first focus groups from the respective sites were presented to participants in the second focus groups in order to gain participants’ validation. The final analysis meeting of all research collaborators and the patient research partner ensured that researchers from any site could picture and understand the institutional processes in which rehabilitation services are provided and the findings from the other sites. Moreover, the discussions during this meeting with people from all 3 sites ensured that all sites were represented accurately, adequately and comprehensively.
RESULTS
Twenty patients and 20 HP participated in 12 focus groups (2 for patients and 2 for HPs in each country). Characteristics of participants are shown in Table I. The results are presented as follows: first, a description of the institutional structure and related processes at each site is presented; and, secondly, themes related to similarities and differences across sites are outlined.
|
Table I. Demographic data of study participants |
|||
|
Demographic data |
AUT site |
SE site |
UK site |
|
Patients |
|||
|
Number of patients |
7 |
4 |
9 |
|
Women, % |
6 (86) |
3 (75) |
6 (66) |
|
Age, years; median (range) |
49 (30–69) |
60,5 (53–67) |
64 (59–73) |
|
Disease duration, years; median (range) |
9.5 (3–36) |
8 (1–16) |
7 (3–24) |
|
Treated at clinic, years; median (range) |
8 (1–14) |
8 (1–16) |
4 (2–20) |
|
Health professionals |
|||
|
Number of health professionals |
7 |
7 |
6 |
|
Women, % |
6 (86) |
7 (100) |
5 (83) |
|
Age, years; median (range) |
48 (26–51) |
54 (52–59) |
36,5 (29–48) |
|
Worked at this site, years; median (range) |
3 (1–21) |
23 (7–24) |
6 (2–16) |
|
Professional background |
Radiographer, OT, nurse, doctor |
PT, OT, nurse, assistant nurse social worker, doctor |
PT, OT, nurse, doctor, podiatrist |
|
AUT: Austria; OT: occupational therapy; PT: physiotherapy; SE: Sweden; UK: United Kingdom. |
|||
Description of sites and institutional processes
The 3 selected sites are all publicly funded university clinics and, hence, operate within a governmental frame of reference. The rheumatology units are supervised by a medical doctor specialized in the area of rheumatology and include an inpatient ward, an outpatient ward, and a day clinic at each site. Analysis focussed on institutional processes in the outpatient wards. The services offered at each site and the professionals involved varied across sites, as described in Fig. 2.
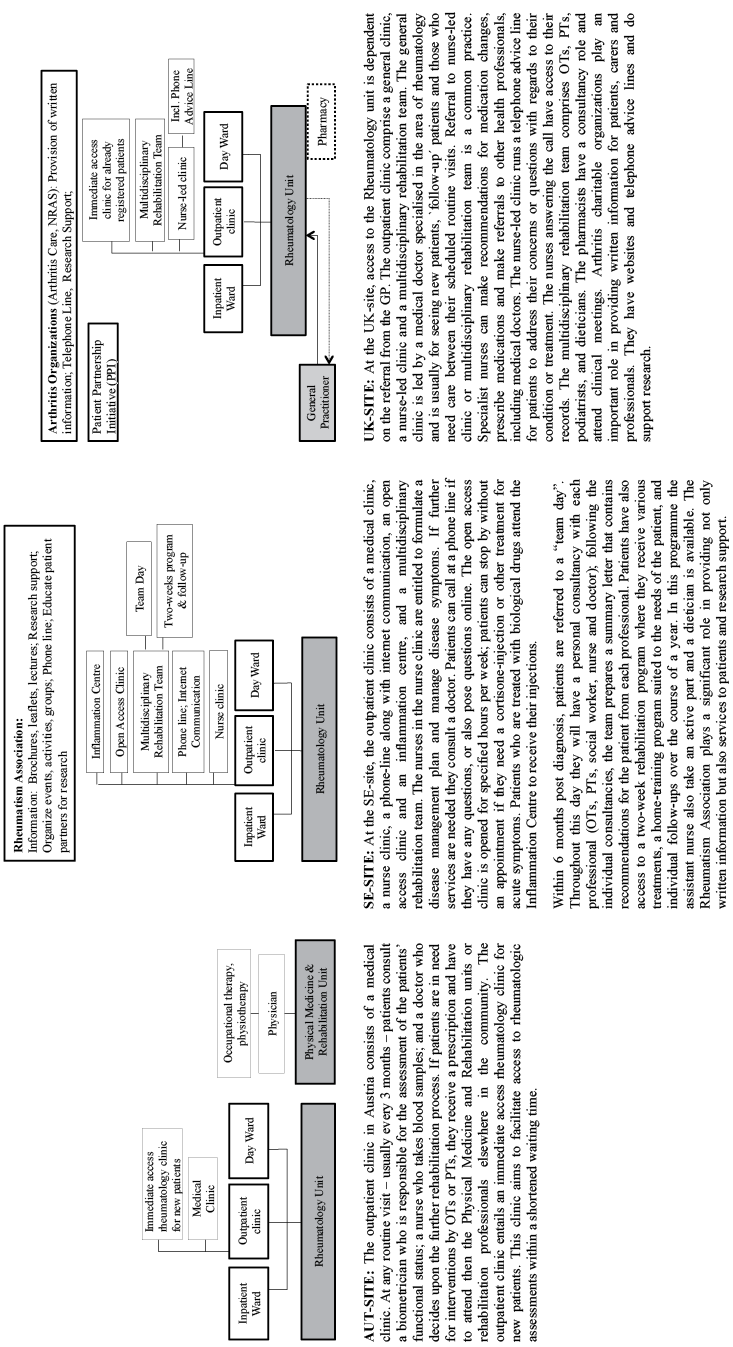
Fig. 2. Institutional processes at each site.
Similarities and differences between sites
The findings presented in this section reflect the themes that emerged in the focus groups. In the subsequent paragraphs, each theme is described by highlighting the similarities and differences across sites. Table II complements these paragraphs with participants’ quotations.
Referrals. Referrals were mentioned at each site, but with varying importance. In Austria allied HPs (occupational therapists, physiotherapists, etc.) require a doctor’s referral in order to treat a patient, as constituted in the law for allied HPs. Referrals are also required if the patient wants to consult therapists at another unit within the same clinic. Cross-referrals across allied HPs are not possible. In contrast, in Sweden HPs can make cross-referrals within the specialized setting once a patient is registered. In Sweden patients can also make self-referrals; for instance, for pool training. In the UK, the GP is the gatekeeper to specialized care. Here, patients and HPs stressed the salient role of the GP in gaining access to, and coordinating, specialized care. Once registered in secondary care, cross-referrals by therapists are possible.
|
Table II. Themes that revealed in the focus groups and reflect differences in the institutional processes across the 3 sites |
|||
|
AUT site |
SE site |
UK site |
|
|
Referrals |
This [getting referrals] is an additional step, which is very burdensome for the patient. And, of course, you also have to see it from an economic point of view. Why do you need a second consultation if it is not necessary? (HP, L95-105) |
Then there is also self-referral, especially to the pool (HP, L397-413) |
I‘ve got a superb GP, which helps enormously. (Pat. L369) You need a really good GP, ‚cos like [name of other participant] said, if you‘ve got a really good GP they can recognize that you‘ve got RA and know where to send you. (Pat. L504-506) |
|
Continuity of rehabilitation |
We don‘t have such a continuous system (…) it depends on individuals … the system does not regulate it. (HP, 162-171) The connections between the departments basically don‘t exist. You only learn about it over time. Yes, you only learn about it. I think so too. You only learn about it with increasing disease duration and increasing experience. (Pat. L539-553) |
The main principle is that the nurse has an important role in providing information about the drugs, so that the patients are on the right track, that there is no misunderstanding; it is just not sufficient to provide the information on the first day Pat. It is so much to absorb. We have seen that there would be misunderstandings in the medication intake. The nurse is very important to ensure that patients really follow the referral in the right way. (HP, L75-79) |
You could ring your specialist nurse; you couldn‘t ring your consultant, so you did feel as if there was an intermediate. Very valuable… . And she goes through everything with you, and then sends you to have a blood test, whatever, and you might see your rheumatologist next time, but they specialize, and that has been very good. It‘s a few years now that they‘ve come up with this concept. (Pat. L 472-495) |
|
Information provided to patients |
I believe, when you receive your diagnosis (…) and have no clue how things will continue and I was only told: „what you would like to become a nurse, well, that won‘t work out, and then, Aha, you are horse riding, well, that won‘t be possible anymore.“ and these were all things that gave everything a negative twist right from the beginning and all these things won‘t be possible anymore. Nobody said, now we are going to do this and that, then we are going to do this therapy and you can try this and we will find a way and will have a look how you are doing. Maybe you can continue then with everything. (Pat. L979-1002) |
The basic policy is that all new patients should be offered a team day within the first 6 months after diagnosis. Partly because of the help they can get from the team, but also to see and learn about the whole panoply of what therapies are available, so that in the future they can themselves formulate whom they may have to see. (HP, L155-158) If you must mention the letter. When the team meets after the patient had gone home, the recorder goes around, each team dictates a little bit about the patient, findings and recommendations for future training and medication. And finishes with information about the next appointment, so that patients have it all together on one paper. Initially it was thought that patients would take this letter and could show it to interested relatives or to the doctor in any other part of Sweden, if having an emergency when on summer vacation. (HP, L169-202) |
This is the gold standard [referring to what is outlined in the NICE guidelines for RA with respect to patient education]. This is basically mostly unachievable. [laughter] It is! (…) when you bear in mind that we are a regional centre that has a patient caseload of thousands, we‘ve got 2.8 nurse specialists. Who are the people who do the majority of patient education? Nurse specialists. But there‘s no way on this earth that we could provide that with the staffing that we‘ve got, and we are a very low priority in the great food chain of the musculoskeletal services for the NHS. So beautiful, but unachievable. (HP, L476-483) I think the problem we have when we‘re first diagnosed, is that nobody sits down, explains properly what RA is. (Pat. L199-205) |
|
Patients‘ organizations |
Not discussed. |
We collaborate with patient organizations, for example regarding in the information brochure and regarding many other things. The Rheumatism Association is the largest individual patient; they have a lot of skilled people in their organization (…) There is some good material there. The Rheumatism Association is also a bit involved in the rehabilitation processes, one can say. (HP, L54-73) |
If you subscribe to the arthritis magazine, you know about all the treatments that are available. (Pat. L 156) The [1 Out of 3 patient organizations] group, we would use that as an avenue to educate patients. We‘d have set lectures, we‘d have them every 4 weeks, so we had quite a few a year. And that‘s a charity. (HP, L 535-547) |
|
Table II. Contd. |
|||
|
AUT site |
SE site |
UK site |
|
|
Documentation and communication amongst HPs |
Everybody has its own record-system, which remains at the outpatient clinic, the patient moves on elsewhere with the referral … then you ask „Why are you coming?“, or „What are your laboratory results?“; then you have to print the results again, although they are already in the other record, which you don‘t get … this is really difficult. (HP II, L470-474) Well, I do have to report all my medication again, and then I have to say exactly when I have been here the last time and then one starts to search. That is consultation time that gets lost on the costs of the patient. (Pat. L314-330) Also, information gets lost between departments – always: in the staircase, in the elevator. (HP, L438-461) |
I can read others‘ notes. That‘s for all; you can make your own notes and read the others‘ notes. It is structured with fixed keywords. That way we try to avoid double-documenting. We all have the same data record, so that no doctor would write what the physiotherapist has already recorded, or the nurse doesn‘t have to write as the doctor has it already done. (HP, L 207-258) |
One of the main patient complaints is that when they go to clinic they have to start from the beginning again with their history because again, going back to the fact that we rely on paper notes, that some things aren‘t filed, some things aren‘t in the right order, the results aren‘t always in the notes, that we do rely heavily on the patient history when they come to clinic. (HP, L 416-441) It‘s about that closer working, because, at the moment, the OT and PT department sits downstairs and sometimes you feel like you don‘t really know what‘s going on and it would be much easier to be able to say, „well y‘know, will you come and have a look at this patient?“ or „can you do this?“. (HP, L228-255) |
|
Interface between primary and specialist care |
Similar efforts to improve interface between primary and specialist provision of services were mentioned at each site, as outlined in the text. |
||
|
Prescription practices |
When I get a prescription, I have to go to my GP, have to pay there for the visit I don‘t understand that. You are sent from the specialist back to the GP (…) These are errands where you think … this is basically not necessary. Especially when your feet are already impaired, these are incredible distances, which are not necessary at all. (Pat. L140-186) |
I always come in late spring and then it‘s been a year and my prescription is expired, and when you go through the recipes, so they are renewed for 1 year. (Pat. L270-279) |
|
|
AUT: Austria; GP: general practitioner; HPs: health professionals; OT: occupational therapy; Pat.: patient; PT: physiotherapy; SE: Sweden; UK: United Kingdom. |
|||
Continuity of rehabilitation. The role of the nurse was particularly salient with respect to continuity of care. Based on the findings of the focus groups, the Austrian system is not set up to be continuous. Individuals (patients and professionals alike) have to ensure continuity. For patients this becomes easier with increasing disease duration, as they develop a better understanding of how the institution operates. At the SE and UK site it is the nurses who see the patients regularly. Patients do not have to see a doctor at every visit. Patients appreciated the role of the nurse and pointed out that it is the nurse who ensures continuity and coherence in rehabilitation.
Information provided to patients. The time at which patients receive information about their diagnosis, as well as the amount and type of information provided, was discussed at all 3 sites. Patients in the Austrian focus groups stressed that the information they received with regard to living with RA was portrayed rather negatively. Very little information was provided about the possibilities regarding rehabilitation and what a patient would still be able to do in daily life. Based on the findings of the focus groups at the SE site, information is dealt with comprehensively and in a multi-modal manner. Moreover, additional information is provided by the rheumatology association (Reumatiker-forbundet) and the multidisciplinary rehabilitation team within special education sessions. Dieticians are also available for consultation and provide, for instance, information about the side-effects of cortisone. At the UK site, information was not dealt with satisfactorily as voiced by patients and HPs alike. While the provision of information (including patient education) is outlined in the respective guidelines of the National Institute for Health and Care Excellence (NICE), HPs stressed that there are no additional resources allocated to enact what is set out in the guidelines.
Patients’ organizations. Patients and HPs at the SE and UK sites regarded patients’ organizations as playing an important role in rehabilitation services provided to people with RA. In contrast, at the AUT site, no patient organization was mentioned in the focus groups; only a short reference was given to privately-run self-help groups. At the UK site, several arthritis-related charitable and non-profit organizations were mentioned, which provide information for patients, organize events for patients and the public, provide funding for research and further education, and advocate for the rights and needs of people with arthritis.
Documentation and communication amongst HPs. Documentation and communication differed at the respective sites. At the AUT and UK sites routine documentation was mostly on paper, whereas at the SE site it is electronic and all HPs have access to the hospital records. At the AUT and UK sites, where formal communication was paper-based, HP discussed additional possibilities for exchanging information through informal means. Informal means of communicating were largely informed by the vicinity of therapy rooms and offices, as illustrated by the quotations in Table II. Communication amongst professionals is facilitated at the SE site through the “team day” offered to patients and the subsequent preparation of the “Summary letter” for the patient (see also description in Fig. 2). It is worth mentioning that, besides the routine documentation, there is a National Quality Register in Sweden. Certain information is entered into this register by patients at each visit in order to maintain and improve the quality of healthcare provision across Sweden.
Interface between primary and specialist care. In the focus groups at each site increasing efforts toward enhancing awareness of RA in primary care were highlighted, such as medical doctors specialized in rheumatology running consultancies in primary care. Such initiatives aim to improve the interface between primary and specialist care. Patients and HPs across all sites highlighted that RA has received more media attention, and public health campaigns are geared toward providing information about RA. Such efforts raise awareness about the disease: patients see specialists earlier, and the increased awareness reduces stigma or stereotypical opinions amongst the public (e.g. that RA occurs only in elderly people).
Prescription practices. At the AUT and SE sites an additional theme on the prescription of medication emerged. In Austria, hospital-based and community-based healthcare operate within different funding schemes (28). The outpatient clinic is included in the hospital-based funding as it is attached to the hospital. However, prescriptions that patients receive from the outpatient clinic are reimbursed by the community-based scheme, based on a codex of reimbursement. Patients have to verify with their GP whether the prescribed medication is included in the codex.
Swedish pharmacies are partly privatized; there are licensed pharmacies that have access to a national database where any prescriptions of pharmaceuticals for patients are registered. Doctors can provide patients with prescriptions of up to 1 year; pharmacists can subsequently provide the patients with medication for a consumption-period of not more than 3 months. Medication can be picked up at any pharmacy throughout the country that is legitimized to access the database (29).
Across all sites, patients in the focus groups emphasized that they went through a process of being newly diagnosed and a novice within the healthcare system, then, over time, they got to know the system better and learned where to get information and access to services.
DISCUSSION
This study provides a reconstruction of institutional processes within which rehabilitation services are provided to patients with RA at specific sites in AUT, SE and the UK. Furthermore, the results shed light on similarities and differences in these processes and services.
The findings from the AUT site point to a rather hierarchical structure of the Austrian system, with allied HPs requiring doctors’ referrals, and patients being assigned a rather passive role as service recipients. Documentation and communication across HPs is mainly paper-based, and patients emphasized that limited information is provided to them.
The findings from the UK site were that rehabilitation services were referred to as meeting the needs of patients well, whereby the nurses take on a leading role. Documentation and communication across HPs is primarily on paper. While the provision of information to patients was emphasized as being important, patient education, in particular, was referred to as “being a rather unfeasible ideal”.
The findings from the SE site revealed that rehabilitation services are set up toward shared responsibility of patients and HPs and the empowerment of patients through the provision of comprehensive information, in particular within the frame of the team day. Documentation is mainly electronic. Referral and prescription practices are organized to meet the needs of patients in a flexible, yet structured, manner.
While most of the themes are evident at each site, there are variations within these themes across sites. With respect to patient organizations, they were almost absent in Austria, but were found to play a role in the rehabilitation processes at the UK and SE sites. They have a particularly salient role in Sweden, where collaborations of policymakers and service providers with patient organizations mark a significant contribution of the patient organizations to ensure and enhance quality and safety of care across Sweden (29). Regarding documentation and communication, the SE site was the only site primarily using electronic records. The challenges of limited communication amongst HPs mentioned at the AUT and UK sites were not supported at the SE site, where the records were fully accessible to all HPs.
Further differences occurred with regard to referrals, whereby the AUT site was the only one where physicians’ referrals are required in order to access allied HPs. This referral practice is increasingly put under scrutiny, and alternative models for providing rehabilitation services, such as extended roles (7) or direct contact with HPs (30), are suggested. In addition to more direct access to allied HPs at the UK and SE site, the role of nurses was stressed at those sites. Previous research based on patients’ perspectives has shown that nurse-led clinics facilitate the distribution of, and access to, information, accessibility to nurses whenever needed, regularity of visits, and comprehensive and coordinated care (31). Information provision to patients appeared to work best at the SE site, based on the findings of this study. Challenges in information provision in the UK are also supported by a previous UK study, in which PTs indicated that they felt restricted by the system in providing information to patients due to high case-loads and limited time for consultations and follow-ups (32).
While previous research has frequently stressed a discrepancy between patients’ and HPs’ perspectives on rehabilitation processes and related services (10, 33, 34), the findings of our study indicate agreement of patients and HPs on important themes regarding the institutional processes. The complementary insights of patients and HPs on what works and what could be optimized in providing rehabilitation services at the selected sites, as well as the similarities and differences across sites, may spark innovative suggestions for further optimization of the institutional processes in which rehabilitation services are provided. In addition, comparisons across sites from different countries offer relevant information and examples of how (parts of) institutional processes within which rehabilitation services are provided can be set up differently.
Study limitations
This study has some limitations. No information about the level of functioning of participating patients was collected. The level of functioning at the point of recruitment to the study was not assessed, as this study aimed at institutional processes, thus disease duration and the duration of treatment at the respective site were considered the most important indicators for gaining knowledge about the processes. Future studies should include a more detailed analysis of how institutional processes are set up to meet the needs of patients with different levels of functioning. Furthermore, only one site per country and only a small number of participants were included in the study from each site. In addition, the focus was limited to outpatient rehabilitation services provided at a specialized rheumatology outpatient clinic. Nevertheless, it is within the nature of qualitative research to aim for an in-depth understanding of the phenomenon, based on the experiences and knowledge of a rather small group of individuals, rather than to aim for generalization (18, 19). Findings gained from qualitative research may provide insights into new aspects of a phenomenon, which were previously not taken into account, and provide the foundation for formulating hypotheses for further empirical testing. It is noteworthy that systems are continuously changing and developing; thus, changes may have occurred during this study, and in the time since study completion, that are not included in the analysis.
Further research is needed to investigate to what extent the themes revealed in this study can serve as a framework for more detailed data collection and comparison of institutional processes, including inpatient and outpatient rehabilitation, across Europe. The inclusion of a wider range of rehabilitation settings nationally and internationally is recommended. For future research, it is also important to consider the International Classification of Functioning, Disability and Health (ICF), as a reference classification published by the World Health Organization (WHO) and a suggested framework for rehabilitation (3, 35, 36), when aiming at optimization of rehabilitation services.
AcknowledgEments
The authors would like to thank all patients and health professionals who participated in this study; and Michaela Stoffer from Vienna, Austria and Dr Jackie Hill and Helen Greenwood from Leeds, UK.
Funding. This study was funded by a EULAR-Health Professional Research Grant.
The authors declare no conflicts of interest.
References
