Robert F. Pangalila, MD1,2, Geertrudis A. M. van den Bos, PhD3, Bart Bartels, PT1,2, Michael P. Bergen, MD, PhD2, Mike J. Kampelmacher, MD, PhD3, Henk J. Stam, MD, PhD1 and Marij E. Roebroeck, PhD1
From the 1Department of Rehabilitation Medicine and Physical Therapy, Erasmus MC University Medical Center, 2Rijndam Rehabilitation Center, Rotterdam, 3Department of Social Medicine, Academic Medical Center, University of Amsterdam, Amsterdam and 4Center for Home Ventilation, University Medical Center Utrecht, Utrecht, The Netherlands
OBJECTIVE: To assess quality of life of adults with Duchenne muscular dystrophy in the Netherlands and to identify domains and major problems influencing quality of life.
DESIGN: Cross-sectional.
SUBJECTS: Seventy-nine men aged ≥ 20 years with Duchenne muscular dystrophy.
METHODS: The Medical Outcome Study Short Form-36 (SF-36), World Health Organization Quality of Life – BREF (WHOQOL-BREF) and an interview were used to assess quality of life and problems.
RESULTS: Compared with Dutch general population reference values, the SF-36 domains scores were lower on all domains except mental health and role limitations due to emotional problems. On the WHOQOL-BREF the social relationships domain score was lower. Main problems were intimate relationships, work, leisure, transport and meaningfulness of life. Seventy-three percent stated overall quality of life as “(very) good”. The SF-36 domains mental health (rs 0.53, p < 0.001) and vitality (rs 0.49, p < 0.001) had the strongest associations with overall quality of life.
CONCLUSION: Adult men with Duchenne muscular dystrophy assess their health status as low in the physical, but not in the mental, domains. Experienced problems are mainly in the area of participation. They are generally satisfied with their overall quality of life.
Key words: Duchenne muscular dystrophy; adult; quality of life.
J Rehabil Med 2015; 47: 161–166
Guarantor’s address: R. F. Pangalila. Erasmus MC, Department of Rehabilitation Medicine, PO Box 2040, NL-3000 CA Rotterdam, The Netherlands. E-mail: r.pangalila@erasmusmc.nl
Accepted Jul 7, 2014; Epub ahead of print Dec 9, 2014
Introduction
Duchenne muscular dystrophy (DMD), an X-linked neuromuscular disease, is the most common form of muscular dystrophy in childhood. It occurs in approximately 1/3500 live male births. In its natural course, DMD leads to progressive muscle wasting, which results in loss of ambulation at around 10 years of age, progressive loss of upper limb function, and cardiac and respiratory failure, with death occurring at around 20 years of age (1). From pre-puberty, boys are increasingly care-dependent for activities of daily living. In the last decades, improvement in care, most notably the introduction of home mechanical ventilation, has led to a considerable increase in life expectancy; nowadays 60% of patients survive into the third decade (2–4). As a result, we are confronted with a relatively new group of adult patients with DMD. As it is likely that this group will expand in the future due to further improvements in therapy (5, 6), it is important to gain knowledge about health, participation and quality of life (QoL) of these adults with DMD in order to provide adequate care.
The increase in life expectancy notwithstanding, muscle wasting continues; without exception, adults with DMD are severely disabled and heavily dependent on care. In the past, doubts have been voiced about the QoL of these men, sometimes leading to withholding information about life-prolonging ventilation by physicians to patients and their family (7). On the other hand, several studies have shown that the patients themselves generally consider the quality of their lives to be good, even in the face of their severe disability (8–10). In children, too, there is debate, some studies finding a good QoL (11, 12), others finding a lower QoL (13–15). One study (16) found that older boys perceived better psychosocial QoL than younger boys.
To add to a more thorough understanding of the health-related QoL of adult men with DMD in the Netherlands we chose a broad approach, addressing different aspects of health-related QoL. We focused on both the assessment of health status by the adult DMD patients and their subjective evaluation of their health status, overall and in physical, psychological and social domains. We studied the following questions: (i) on which domains of QoL do adults with DMD indicate major problems? (ii) How do adults with DMD perceive their overall QoL? and (iii) Which domains are related to overall QoL? Knowledge of the level and the contributing domains of QoL may aid in designing care and educational programmes that aim, from childhood on, to acquire skills and render opportunities for adults with DMD in the salient domains.
Methods
Subject selection and procedure
This study was part of a larger, cross-sectional study into the functioning and QoL of adults with DMD and their informal caregivers. Subjects were recruited by letter by all 4 Centers for Home Ventilation in the Netherlands, and by Dutch rehabilitation centres and the Dutch patient organization for neuromuscular diseases (Spierziekten Nederland). Inclusion criteria were a diagnosis of DMD and an age of 20 years or over. All subjects gave written informed consent for participation. The subjects were interviewed during 2 consecutive visits to their homes to prevent overexertion as the entire procedure took more than 4 h. The study was approved by the medical ethics committee of the Erasmus University Medical Center, Rotterdam, The Netherlands.
Measurements
We recorded age, data on physical situation (ventilation, gastrostomy, ambulation using the Vignos scale (17), hand function using the Brooke scale (17), use of medication and on participation (living situation, relational status, education level, work) to describe our population. For this study we used 2 widely used generic measures for health-related QoL: the SF-36 (18), addressing health status and the World Health Organization Quality of Life – BREF (WHOQOL-BREF) (19), emphasizing the subjective evaluation of health-related QoL. The Medical Outcome Study Short Form-36 (SF-36) comprises 36 questions that are combined into 8 subscales: physical functioning (PF), role limitations due to physical health problems (RP), bodily pain (BP), general health perception (GH), vitality (VT), social functioning (SF), role limitations due to emotional problems (RE) and mental health (MH). Scores on the subscales range from 0 to 100, with higher scores representing better QoL. The SF-36 has been validated extensively (18). The WHOQOL-BREF is a questionnaire developed for cross-cultural comparison of QoL relevant to global well-being (19). It comprises 26 items; 1 item measuring overall QoL, 1 measuring satisfaction with health, and 24 items that can be combined into subscales for 4 domains (physical functioning, psychological functioning, social relationships and environment). All items are assessed with a 5-point Likert scale. Item scores are converted to domain scores ranging from 4 to 20, with higher scores representing better QoL. The WHOQOL-BREF has good validity, internal consistency and test-retest reliability (20).
Also, we used the single-item overall QoL score of the WHOQOL-BREF to assess associations of overall QoL with health status as measured with SF-36 and the QoL domains as measured with the WHOQOL-BREF.
To find potential aspects not covered by the standard measurements we also asked all subjects to indicate what they considered the 3 greatest problems they had related to the fact that they had DMD.
Statistical analysis
With SPSS version 16, descriptive statistics were used to assess the outcomes on the various measurements. We used a 1-sample t-test to compare the outcomes with a reference population. As the distribution of the results was not normal, Spearman’s rho was used to assess associations between the single-item overall QoL outcome of the WHOQOL-BREF and the domains of WHOQOL-BREF and SF-36.
Results
We located 151 patients; 80 agreed to participate in the study. One patient was excluded due to too much missing data. The mean age and the distribution of ventilation type (none, non-invasive or invasive) of the non-responding group were comparable to those of the responders.
Table I shows that the participants were severely disabled (all were wheelchair dependent and most were only able to use their hands in table-top activities) and had a low participation in intimate relationships and paid employment. Comparing the scores on domains of QoL, as measured with the SF-36, the men with DMD scored considerably lower on the physical domains and social functioning, but equal or even higher on the domains role limitation – emotional and mental health compared with a Dutch reference population (18) (Table II). Comparing the domains measured with the WHOQOL-BREF with a Dutch reference population (21), there was no difference in evaluation of physical functioning and environment. The men with DMD scored lower on social relationships, but once again slightly, though statistically significantly, higher on psychological functioning. Looking at the WHOQOL-BREF items in more detail (Table III), the subjects emerging as the most problematic were: sexual life, employability, meaningfulness of life and possibilities for transport and leisure activities. The least problems were experienced with pain preventing necessary activities, acquiring relevant information and accepting bodily appearance – notwithstanding being wheelchair-dependent and often having deforming contractures.
|
Table I. Demographics and patient characteristics |
|
|
Patient characteristics |
|
|
Age, years, mean (SD) |
28.2 (6.3) |
|
95% CI [range] |
26.8–28.2 [20–44] |
|
Mobility, % |
|
|
Vignos 9 |
98.7 |
|
Vignos 10 |
1.3 |
|
Hand function, % |
|
|
Brooke 3 |
2.5 |
|
Brooke 4 |
6.3 |
|
Brooke 5 |
88.6 |
|
Brooke 6 |
2.5 |
|
Educational level, % |
|
|
Practical |
46.8 |
|
Lower |
24.1 |
|
Intermediate |
20.3 |
|
High |
8.9 |
|
Cardiac medication, Yes, % |
64.5 |
|
Antidepressant medication, Yes, % |
11.4 |
|
Gastrostoma, Yes, % |
27.9 |
|
Ventilation, % |
|
|
None |
1.3 |
|
Non-invasive |
45.6 |
|
Invasive |
53.2 |
|
Living situation, % |
|
|
Parental home |
58.2 |
|
Individual |
7.6 |
|
Residential |
34.1 |
|
Relational status, % |
|
|
Steady partner |
9.0 |
|
On-off |
3.8 |
|
Single |
87.2 |
|
Employment (n = 70), % |
|
|
None |
84.3 |
|
≤ 24 h/week |
11.4 |
|
> 24 h/week |
4.3 |
|
95% CI: 95% confidence interval; SD: standard deviation; Vignos 9: wheelchair dependent; Vignos 10: bedridden; Brooke 3: brings glass of water to mouth; Brooke 4: brings hands to mouth; Brooke 5: table-top activities; Brooke 6: no functional use of hands; cardiac medication: a.o. Perindopril, diuretics; antidepressant medication: a.o. Paroxetine, Amitryptiline, Oxazepam. |
|
|
Table II. World Health Organization Quality of Life – BREF (WHOQOL-BREF) and Short Form-36 (SF-36); domains compared with norm (n = 79) |
||||
|
Domains |
Mean (95% CI; SD) |
Ref (SD) |
Mean diff |
p |
|
WHOQOL-BREF |
||||
|
Physical health |
15.0 (14.4–15.6; 2.5) |
15.2 (2.6) |
–0.2 |
0.437 |
|
Psychological health |
14.9 (14.4–15.4; 2.3) |
14.3 (2.0) |
0.6 |
0.035 |
|
Social relationships |
13.8 (13.2–14.4; 2.6) |
15.4 (2.9) |
–1.6 |
< 0.001 |
|
Environment |
15.8 (15.3–16.2; 1.9) |
15.8 (2.0) |
0.0 |
0.753 |
|
SF-36 |
||||
|
Physical functioning |
0.0 |
93.1 (11.8) |
||
|
Role limitations–physical |
66.1 (57.6–74.8; 38.6) |
86.4 (27.6) |
–20.3 |
< 0.001 |
|
Bodily pain |
73.0 (68.1–77.8; 21.6) |
80.9 (19.4) |
–7.9 |
0.002 |
|
General health perception |
46.0 (41.8–50.3; 18.9) |
78.2 (17.3) |
–32.0 |
< 0.001 |
|
Energy vitality |
64.4 (60.5–68.2; 17.1) |
70.7 (16.4) |
–6.3 |
0.002 |
|
Social functioning |
75.0 (69.5–80.5; 24.8) |
87.8 (19.1) |
–12.8 |
< 0.001 |
|
Role limitations–emotional |
91.6 (84.4–96.7; 22.9) |
85.4 (30.0) |
6.2 |
0.019 |
|
Mental health |
76.6 (73.3–79.6; 13.2) |
78.7 (15.2) |
–2.0 |
0.174 |
|
95% CI: 95% confidence interval; SD: standard deviation. One-sample t-test. WHOQOL-BREF: Dutch general population; n = 218 (21). SF-36: Dutch general population age 16–40 years (18). |
||||
|
Table III. Problem inventory: items of World Health Organization Quality of Life – BREF (WHOQOL-BREF) ranged from most to least problematic (1: very poor, 5: very good)) and problems indicated in open questions (n = 79) |
|||||
|
Mean (IQR) |
Median [range] |
Self-indicated problems |
|||
|
Problem |
Participants (%) |
||||
|
1 |
Sex life |
2.73 (2–3) |
3 [1–5] |
Intimate relation |
15.2 |
|
2 |
Work capacity |
3.24 (3–4) |
4 [1–5] |
Work |
3.8 |
|
3 |
Meaningfulness of life |
3.30 (3–4) |
3 [1–5] |
||
|
4 |
Transport |
3.34 (3–4) |
4 [1–5] |
Mobility |
34.2 |
|
5 |
Leisure activities |
3.38 (3–4) |
3 [1–5] |
Going out |
20.3 |
|
Sport |
8.9 |
||||
|
6 |
Enjoying life |
3.56 (3–4) |
4 [1–5] |
||
|
7 |
Sleep |
3.56 (3–4) |
4 [1–5] |
||
|
8 |
Performing daily activities |
3.57 (3–4) |
4 [1–5] |
Dependency |
27.8 |
|
9 |
Energy for daily life |
3.61 (3–4) |
4 [1–5] |
Fatigue |
12.7 |
|
10 |
Satisfaction with oneself |
3.66 (3–4) |
4 [1–5] |
||
|
11 |
Negative feelings |
3.73 (3–4) |
4 [2–5] |
||
|
12 |
Conditions of living place |
3.76 (3–4) |
4 [1–5] |
||
|
13 |
Personal relationships |
3.77 (4–4) |
4 [1–5] |
Social relations |
16.5 |
|
14 |
Access to health services |
3.78 (3–4) |
4 [1–5] |
||
|
15 |
Need of medical treatment in daily life |
3.80 (3–5) |
4 [1–5] |
||
|
16 |
Support from friends |
3.85 (3–4) |
4 [1–5] |
||
|
17 |
Healthiness of physical environment |
3.89 (3–5) |
4 [1–5] |
||
|
18 |
Ability to concentrate |
3.90 (3–5) |
4 [1–5] |
||
|
19 |
Ability to get around |
3.96 (4–5) |
4 [1–5] |
Access |
5.1 |
|
20 |
Enough money |
4.20 (4–5) |
4 [1–5] |
||
|
21 |
Safety in daily life |
4.23 (4–5 |
4 [2–5] |
||
|
22 |
Accepting bodily appearance |
4.28 (4–5) |
5 [1–5] |
||
|
23 |
Availability of information |
4.35 (4–5) |
4 [2–5] |
||
|
24 |
Physical pain |
4.44 (4–5) |
5 [1–5] |
Pain |
10.1 |
|
Negatively phrased items recoded. PARTICIPANTS: % of participants naming a problem domain. IQR: interquartile range. |
|||||
The greatest problems, as indicated in the open questions, are also shown in Table III. 36 subjects mentioned 3 problems, 21 mentioned 2, 12 mentioned 1 and 10 did not mention any problem. Mobility, dependency and opportunities to go out were mentioned most frequently.
The severe level of disability notwithstanding, 73% of participants stated that their QoL was good or very good and only 8% considered their QoL to be (very) poor (Fig. 1). Even in this population, more than half were satisfied with their health (Fig. 2).
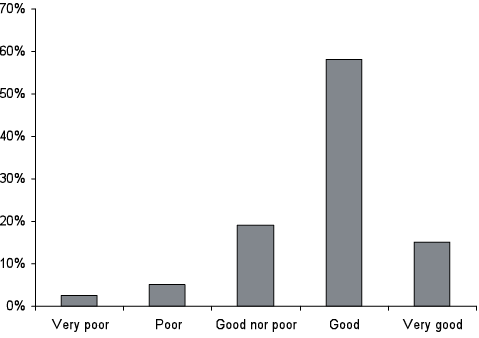
Fig. 1. Overall quality of life. World Health Organization Quality of Life – BREF (WHOQOL-BREF) 1-item overall quality of life rating (n = 79).
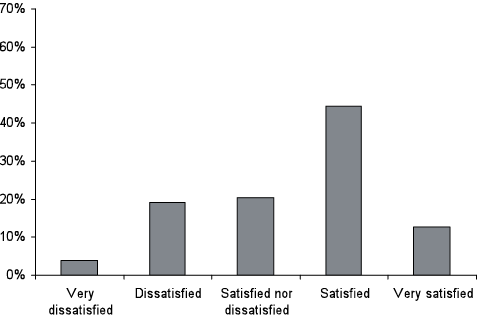
Fig. 2. Satisfaction with health. World Health Organization Quality of Life – BREF (WHOQOL-BREF) 1-item satisfaction with health rating (n = 79).
All domains of the WHOQOL-BREF and the SF-36 showed a correlation with overall QoL, as measured with the single-item question of the WHOQOL-BREF. For the SF-36, the strongest associations were with mental health and vitality; for the WHOQOL-BREF with physical health and psychological (Table IV).
|
Table IV. Correlation World Health Organization Quality of Life – BREF (WHOQOL-BREF) and Short Form-36 (SF-36) domains with overall quality of life (WHOQOL-BREF item 1) (n = 79) |
||
|
Overall QOL |
||
|
rs |
p |
|
|
WHOQOL-BREF |
||
|
Physical health |
0.47 |
< 0.001 |
|
Psychological health |
0.55 |
< 0.001 |
|
Social relationships |
0.31 |
0.006 |
|
Environment |
0.29 |
0.011 |
|
SF-36 |
||
|
Physical functioning |
||
|
Role limitations-physical |
0.26 |
0.020 |
|
Bodily pain |
0.22 |
0.046 |
|
General health perception |
0.39 |
< 0.001 |
|
Energy vitality |
0.49 |
< 0.001 |
|
Social functioning |
0.28 |
0.012 |
|
Role limitations-emotional |
0.39 |
< 0.001 |
|
Mental health |
0.53 |
< 0.001 |
|
Change in health |
0.25 |
0.024 |
|
QOL: quality of life. Two-tailed correlation, Spearman’s rho. |
||
Discussion
When assessing QoL, it is important to consider what is meant by the term. In line with the World Health Organization (WHO) definition, it is seen as a broad-ranging concept affected in a complex way by a person’s physical health, psychological state, level of independence, social relationships, and their relationships with salient features of their environment (22). In relation to health and disease states, health-related QoL was developed to abridge the QoL construct and to place emphasis on the domains relating to health (23). Both the level of health problems and disabilities (health status) and the (subjective) evaluation of these disabilities may be assessed (24).
Comparing the WHOQOL-BREF and the SF-36, Huang (19) found that they measure different constructs: the SF-36 measures health status: perceived states, capabilities and functioning related to health; the WHOQOL-BREF measures satisfaction with the perceived states of and capabilities and functioning related to health and the other domains, making it a more subjective assessment. Also, the WHOQOL-BREF measures a broader range of perceptions, including personal health, access to healthcare and social services, social network, spirituality and safety of the personal environment, leading to a more global assessment of QoL.
These differing constructs are reflected in our findings. The adults with DMD in our study are severely disabled in physical and social domains of health status, but not on psychological domains. The scores on the SF-36, compared with the general population, show that they are aware of their disabilities. Nevertheless, adults with DMD are often satisfied with the way the activities corresponding with these disabilities are managed, as shown by the scores on the WHOQOL-BREF. They are least satisfied with their sex life, employment and transportation. In general, they are satisfied with their overall QoL.
These findings demonstrate the so-called disability paradox. The discrepancy between level of disability and QoL may be due to the fact that their relationship is far from straightforward; there are no linear associations between severity of disability and perceived QoL (25). People faced with chronic disease or disability learn to re-evaluate their situation and their desires in life (“response shift”) (26). As a result, they may express satisfaction with certain situations or activities (for instance, moving around, albeit in a wheelchair), where others would consider them disadvantaged (as they are unable to move around without aids).
Our findings are in line with earlier studies in adult DMD patients. In an early study on life satisfaction of ventilated DMD patients, Bach et al. (8) found that the vast majority had positive affect and were satisfied with life. Rahbek et al. (9) and Kohler et al. (10) also found a high QoL in adults with DMD. Their relative satisfaction with their situation notwithstanding, the patients indicate a relatively low satisfaction with “meaningfulness of life” and often indicate their dependency as a major problem. In a qualitative study in 10 adult men with DMD, Gibson et al. (27) found that these men maintained balance by adopting a day-to-day approach to life, striving to find meaning and satisfaction in the present. Verberkt (28), sister of an adult DMD patient, describes how she admires her brothers’ ability to make the most out of every single moment. Gibson found that patients, in view of the uncertainty of their future, were more disposed toward a deep resignation about their situation; they considered thinking about the future counter-productive. Gibson states that, despite material and social barriers hampering their participation in personally meaningful activities, patients had few complaints and few suggestions for improvement. This is reflected in our study: the patients were often unable to indicate 3 problem areas related to their disease. But as Gibson et al. (27) say, that does not mean that their situations could not be improved in ways that would be welcomed by them. For instance, even though pain is an issue, according to the results on the SF-36 and the open questions somewhat surprisingly the item pain emerges as the least problematic on the WHOQOL-BREF, indicating that pain does not greatly prevent the men from doing what they need to do. Nevertheless, relieving pain would surely be seen as an improvement.
Overall QoL had the strongest associations with the health status domains mental health and vitality. Wagner et al. (29) found that 30% of patients were on anti-depressant therapy; on the other hand, in boys aged 8–17 years Bray et al. (23) found that disease progress was not related to psychosocial functioning. In our study, mental health is rated by the patients themselves as at the same level as in the general population and they experience fewer limitations in their functioning due to emotional problems than the general population. Nevertheless, those patients who have worse mental health are the ones who experience poorer QoL; which might be improved by adequate mental health treatment. In relation to vitality, fatigue is often mentioned as a problem. Approximately one-quarter of the patients in our study were dissatisfied with the quality of their sleep. This could be due to problems with nightly ventilation or mental problems; it is possible that these problems are treatable in the individual patient. Cardiac problems, especially dilated cardiomyopathy, which are frequent in DMD patients (1) may also be a cause of lower vitality.
Adult DMD patients show the least satisfaction in the social domain; here they regard themselves as disadvantaged compared with the general population. They are most dissatisfied with their sexual lives and wish for an intimate relationship; in our study only 1 in 8 patients was involved in a relationship. Also, capacity for work is an important problem area; only 1 in 7 of the adult DMD patients was employed, the majority of these for less than 24 h per week. The findings that sexual relationships and work are major issues are in line with the findings of Rahbek et al. (9). Transportation and opportunities for leisure activities, too, are indicated as problematic areas. All in all, adults with DMD are most dissatisfied with aspects of participation, more than with their overall QoL.
The present sample is a special group, in the sense that they are the first generation of DMD patients to reach adulthood, owing to improvements in care. In their childhood, there was no expectation of an adult life. The low level of participation is partly due to the physical impairments and maybe to cognitive involvement; but it is possible that the fact that patients, parents, and society were not prepared for adult issues in this group influenced actual participation. Parents find it difficult to plan ahead when their sons with DMD are young (30); like their adult sons, they tend to cope with the disease on a day-to-day basis. The educational level of the sample was low; possibly due to a lower cognitive level in some subjects, but also due to the fact that many individuals had been educated at special schools that were not equipped to provide them with the qualifications that would match their intellectual levels. A recent study from England has shown that care for this population, both medical care and care pertaining to acquiring skills of independence, employment and social participation, are insufficiently organized after puberty (31).
Nowadays a substantial percentage of patients with DMD reach adulthood; the standard use of corticosteroids, and the development of new therapies will probably extend life expectancy even further in the future. For these reasons, it is of utmost importance that, like every child, boys with DMD are prepared, both in rehabilitation care and in education, for an adult life with the possibility of social participation that is fully in accordance with their faculties. In rehabilitation care, there should be a specific focus on the transition phase between childhood and adulthood.
Once they reach adulthood, patients with DMD should be offered opportunities to participate. Problems with work, transportation and leisure are amenable to alleviation by measures that could be taken by governments and society, for instance special funding and government guarantees for employers who hire disabled individuals and government funding for hiring aides for transport and support in leisure activities. However, it cannot be automatically assumed that more participation will lead to a measurably better overall QoL (32). The low level of participation notwithstanding, the fact that many adults with DMD report a good QoL is important knowledge. For instance, it may give some perspective to young DMD patients and their families. Also, it should be taken into consideration when assessing whether or not DMD patients should be offered life-prolonging therapies, such as ventilation and cardiac transplants.
Concerning our study there are 2 possible sources of bias that should be taken into consideration. As almost all adults with DMD are known to the Centres for Home Ventilation, we believe that we reached the vast majority of eligible subjects in the Netherlands. Therefore, invitation to participate in this study probably did not generate a bias. However, participation rate was 53%; it is possible that the patients taking part in our study had a relatively more stable health situation and that more unstable patients were less inclined to participate.
Secondly, the findings in this Dutch sample of adults with DMD may not be applicable to populations elsewhere, where there may be a different level of healthcare along with differences in health policies and social opportunities.
In conclusion, the adult men with DMD in our study assessed their health status as lower than the general public in the physical domains but not in the mental domains. They considered their overall QoL to be at the same level as the general population, except on the social domain. Mental health and vitality have the strongest associations with good overall QoL. The major problems experienced by this group are of participation: getting involved in intimate relationships, work and leisure activities and mobility and transportation. DMD patients should, from a young age, be prepared for an adult life with optimal participation; in adulthood, specific social measures are needed to enable them to participate.
ACKNOWLEDGEMENTS
This work was supported by grants of “Children’s Fund Adriaanstichting” (KFA grant number 2005/0143), “Johanna Children’s Fund” (JKF grant number 2005/0143) and “Nuts Ohra Foundation” (grant number SNO-T-0701-85).
The authors wish to thank the Departments of Home Mechanical Ventilation of the University Medical Centers at Rotterdam (J Rischen-Vos, MD), Groningen (PJ Wijkstra MD PhD), Maastricht (NAM Cobben, MD PhD), and patient organization Spierziekten Nederland for recruiting participants for this study.
References
