Evelina Pajediene, MD1, Jolita Janusauskaite, MD1, Gintaute Samusyte, MD1, Kestutis Stasaitis, MD2, Kestutis Petrikonis, MD, PhD1 and Indre Bileviciute-Ljungar, MD, PhD3
From the 1Department of Neurology, Lithuanian University of Health Sciences, 2Department of Anesthesiology and Intensive Care Medicine, Lithuanian University of Health Sciences, Kaunas, Lithuania, and 3Department of Clinical Sciences, Karolinska Institutet, Danderyd University Hospital, Stockholm, Sweden
OBJECTIVE: To investigate acute whiplash-associated disorder in the Lithuanian population who are unaware of the phenomenon.
DESIGN: Controlled cohort study.
SUBJECTS/PATIENTS: Seventy-one patients were enrolled from the emergency departments of the Kaunas region of Lithuania following road traffic accidents, examined within 3–14 days after the accident, and compared with 53 matched controls.
METHODS: Clinical neurological examination, including range of motion and motion-evoked pain or stiffness in the neck; spontaneous pain and pain pressure threshold. Questionnaires: Quebec Task Force questionnaire (QTFQ); Disability Rating Index (DRI); Cognitive Failures Questionnaire (CFQ); Hospital Anxiety and Depression Scale (HADS) and health perception.
RESULTS: Sixty-six of 71 (93%) patients developed acute symptoms. The most frequent symptoms found after road traffic accidents were neck or shoulder pain; reduced or painful neck movements, including decreased range of motion; multiple subjective symptoms according to QTFQ and significantly reduced pain threshold. Perceived health status was decreased and DRI was increased, while HADS showed a significantly higher risk of developing anxiety. Higher grade whiplash-associated disorder was linked with a greater reduction in range of motion and more prominent neck pain.
CONCLUSION: Road traffic accidents induce whiplash-associated disorder in patients who seek help, but who are unaware of the condition whiplash-associated disorder. Whiplash-associated disorder should be considered and treated as an entity per se.
Key words: whiplash-associated disorder; neck pain; headache; disability; traffic collision; neck trauma.
J Rehabil Med 2014; 46: 00–00
Correspondence address: Indre Bileviciute-Ljungar, Department of Clinical Sciences, Karolinska Institutet, Danderyd University Hospital, Building 39, 3rd Floor, SE-182 88 Stockholm, Sweden. E-mail: indre.bileviciute-ljungar@ds.se
Accepted Jun 23, 2014; Epub ahead of print Oct 13, 2014
Introduction
Whiplash-associated disorder (WAD) is a costly health-related problem in developed countries. According to the Whiplash Commission’s Final Report, written by a Swedish medical consensus group in 2005, WAD results in high costs for society: more than 4 billion Swedish crowns annually, most of which is due to loss of productivity and compensation for work disability (1). Although the Quebec Task Force systematic review, presented in 1995, concluded that the prognosis of acute WAD is favourable (2), later studies found that it varies greatly depending on the population sampled and the insurance/compensation system under which individuals are allowed to claim benefits (3).
According to Holm et al. (4), WAD affects people in many countries. However, the expectations of the sequelae symptoms of whiplash injury vary from country to country, as showed by Ferrari & Lang (5). For example, in Lithuania, Germany and Greece, the expectations for persistent symptoms after “perceived” whiplash injury were scored lower compared with the Canadian population (5–7). There is also a clear correlation between patient’s expectations for recovery and prognosis (8, 9). Although, over the last 4 years, the number of people killed on the roads of the Republic of Lithuania has decreased by 53%, according to the main accident indices Lithuania still has one of the highest per capita rates of traffic-related deaths in the European Union (10). Despite the high number of road traffic accidents in Lithuania resulting in injuries (e.g. 3,625 during 2010 (10)), awareness of chronic WAD remains low, among both the general population and the medical community. Awareness of WAD may also be reflected in the frequency of publications in both social and scientific media. For instance, when searching using the keyword “whiplash” with the search engine Google, only 4 articles could be found published in Lithuanian web pages during the past 5 years (the most recent published in 2010), while search for “whiplash” web pages in Swedish language resulted in approximately 60,000 during the same time period. There is also no patient organization or local whiplash patients’ support group in Lithuania.
Some aspects of legal and medical unawareness are confirmed by the fact that long-term working incapacity of severe-to-moderate level (0–55%) during the period from 2008 to 2011 was attributed to 624 patients diagnosed with a cervical disc disorder, but not due to diagnosis of neck ligament distortion or WAD (personal communication from Lithuania’s Disability and Working Capacity Assessment Office). The WAD diagnosis, usually coded as S13.4, is not listed by Lithuanian insurance companies and insurance indemnity. This indicates that chronic WAD, which in a portion of these cases leads to health-related costs in Western countries, is a rare diagnosis in Lithuania.
Based on the assumption that public awareness of WAD in Lithuania is low, the aim of this study was to evaluate the symptomatology by clinical examination and patient-rated questionnaires in patients seeking emergency medical help after motor vehicle collisions. The primary hypothesis was that the Lithuanian population does not develop classical WAD due to ignorance of WAD and the absence of economic compensation for neck trauma caused by road traffic accidents.
Material and Methods
Study group
A controlled cohort study took place in Kaunas, the second largest Lithuanian city, of approximately 340,000 inhabitants. Individuals (both drivers and passengers) who sought medical help at the emergency departments in the Kaunas region from November 2008 to October 2010 after motor vehicle collisions were considered for participation. The main inclusion criteria were age range 18–65 years and involvement in a motor vehicle collision irrespective of its mechanism. The main exclusion criteria were major injuries or bone fractures inflicted during the accident and confirmed at the emergency department. Patients who met the selection criteria were contacted by phone and invited to participate in the study. A visit to the emergency department of Kaunas University Hospital was arranged within 3–14 days after the accident. Acute WAD symptoms are thought to manifest within this time-period (1). Signed consent to participate in the study was obtained prior to any assessment procedures. Medical and surgical histories were taken, and patients with chronic neurological disorders, previous trauma with residual symptoms or spine surgery were further excluded from the study. The rest of the patients, irrespective of the mechanism of collision, head trauma or absence of whiplash-like symptoms, were included. They completed questionnaires and underwent detailed neurological examination in order to detect acute WAD symptoms and signs. As all the participants were native-speaking Lithuanians, there should have been no issues related to language or literacy. While completing the questionnaires, the patients were able to ask any questions that arose, in order to get a more detailed explanation of the task.
Control group
The control group comprised individuals with no history of car accidents, with the rest of the exclusion and inclusion criteria matching those of the study group. The control group was matched by age, sex, education and employment status. Controls were recruited from several sources. Firstly, the study participants were asked to inform their acquaintances about the ongoing study and those willing to participate contacted the investigators. If they met the inclusion and exclusion criteria for the study, they were enrolled in the control group and matched one-to-one with the study group participants and participated in the subsequent follow-up study. Secondly, for each participant who did not have a control, the investigators found a person from their circle (i.e. colleagues, acquaintances, etc.) of the same gender, relatively similar by age, education and employment status who also met the study criteria. The controls underwent the same physical examination and questionnaires as the study group at the time of selection.
Objective examination
Physical examination of the musculoskeletal system in the upper body region and neurological examination were performed to establish the diagnosis and grade of WAD according to the Quebec Task Force (2). The examination of every patient started from standard muscle strength testing in all groups of upper limb muscles using the MRC’s (Medical Research Council) scale and deep tendon reflex testing in upper limbs. Point tenderness to palpation was tested at the projections of spinal processes of the cervical and thoracic vertebra, as well as paravertebrally. Neck range of motion (ROM) and motion-evoked pain or stiffness was also tested. ROM was evaluated using a metric tape, while patients were comfortably seated on a chair with their arms resting on their thighs. Active neck flexion, extension, rotation, and lateral flexion were assessed by measuring the distance between the 2 landmarks in the neutral position and in maximal motion. The ROM was determined by the difference between the 2 measures in cm. The landmarks for neck flexion and extension were the sternal notch and the tip of the chin. The landmarks for rotation were the tip of the chin and lateral tip of the acromion process. The landmarks for lateral flexion were the tip of the mastoid process and the lateral tip of the acromion process (11).
Pressure pain threshold was tested with a hand-held pressure algometer (Pain TestTM Algometer, Wagner Force dial FDK 20) at 14 points (7 sites bilaterally): 1) front chest area at second costochondral junction; 2) back of the neck at suboccipital muscle insertion; 3) trapezius muscle at midpoint of the upper border; 4) shoulder blade area above the medial border of the scapular spine; 5) elbow area 2 cm distal to the lateral epicondyle (these points also correspond to the points of fibromyalgia in the upper part of the body (12); 6) at the median nerve projection 10 cm above the carpal tunnel, and 7) the control point at the middle/upper part of the anterior tibial muscle. Points 1–4 were chosen to evaluate pressure pain thresholds in the neck/shoulder girdle region, which is affected during the whiplash injury; points 5 and 6 – distal points innervated by the cervical nerve roots that may also be affected during the whiplash trauma; point 7 – a control point in a remote region. Patients were instructed and a single trial was carried out before taking the measurements. All points were tested once in the craniocaudal order and measurements were recorded in kilograms per square centimetre (kg/cm2).
The neurological examination was carried out to evaluate a possible nervous system injury and involved standard muscle strength testing in all groups of upper limb muscles using MRC’s scale; deep tendon reflex testing in upper limbs and sensory testing the C2–C7 dermatomes using a 10 g monofilament in order to identify sensory disturbances. Radicular involvement was confirmed when reduced muscle strength and/or reduced or absent deep tendon reflex with or without sensory impairment was detected in the corresponding segment.
Questionnaires
The following questionnaires were used:
1) Visual analogue scale (VAS) (0–100 mm) (no pain – worst pain) to measure pain intensity and general health perception (best health – worst health).
2) Quebec Task Force Questionnaire (QTFQ) to mark symptoms after the accident and to evaluate their severity at the time of testing (2). The QTFQ consists of a list of symptoms (see also Table III) associated with whiplash injury. The patient was asked to mark symptoms he/she was experiencing at the moment of assessment and to grade their severity (mild, moderate, severe, and unbearable).
3) Disability Rating Index (DRI) to evaluate performance of everyday activities and understand the impairments of self-rated physical functioning (13). DRI consists of 12 daily activities, for which patients were asked to score their ability to perform each activity according to a VAS scale, which ranged from 0 to 100, where 0 is “without difficulty” and 100 indicates “not possible”. The total DRI score could range from 0 to 1200.
4) Cognitive Failure Questionnaire (CFQ) to measure person’s likelihood of committing an error in the completion of an everyday task and to understand the impairments of self-rated cognitive functioning (14). CFQ consists of 25 questions and the sum of all answers ranges from 0 to 100, with the cut-off score of 43 and above reflecting cognitive impairment.
5) Hospital Anxiety and Depression Scale (HADS) to determine the levels of anxiety and depression a person is experiencing (15). The entire sum for both HADS anxiety and HADS depression levels ranges from 0 to 21. A score equal to or more than 10 indicates clinically significant symptoms of anxiety or depression.
QTFQ, DRI and CFQ were all translated into Lithuanian, back-translated by native speakers, and readjusted after back-translation. The face validity of the questionnaires was then checked by 3 different neurologists and by a pilot study population of 20 patients who had been involved in motor vehicle collisions. In the pilot group Cronbach’s alpha was 0.86 for CFQ and 0.93 for DRI. Sociodemographic data was also recorded. The study protocol was approved by the Lithuanian Bioethics Committee (BE-2-57, issued 11/09/2008).
Statistics
Descriptive statistics for nominal data are represented by the number of participants/group and percentage. Interval data are presented by mean and standard deviation (SD). Ordinal data are presented by mean and SD as well as median and interquartile range (IQR). The Shapiro-Wilk test was used to test the normality of the sample when the hypothesis of normality is rejected if the p-value is less than 0.05. Baseline characteristics of nominal data (gender, education, employment status) were compared using the χ2 test. For age and body mass index (BMI) t-test was used to compare the basic values. Parametric or non-parametric tests were chosen depending on the normality of the sample. Comparison of self-rated and objective symptoms between the groups was made by using either t-test (ROM, CFQ) or Mann-Whitney U test (degree of WAD, pressure pain threshold, VAS for pain and general health status, total DRI and HADS). The distribution of parametric measurements among WAD grades were analysed by analysis of variance (ANOVA), while distribution of non-parametric data was analysed by Kruskal-Wallis test. Scores of QFTQ between WAD patients and controls were analysed by Mann-Whitney U test.
Ninety five percent confidence intervals (95% CIs) for proportions were calculated. p-values less than 0.05 were considered to be significant. Statistical package SPSS 17.0 and MS Excel were used for coding and analysing the data.
Results
Characterization of participants
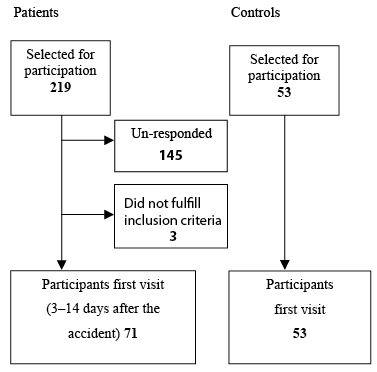
A total of 219 patients were selected for participation. The patient flow is summarized in Fig. 1. For the first visit, 74 patients presented for examination. Three patients were excluded due to pre-existing neurological deficits. Seventy-one patients met all the selection criteria and were examined within 3–14 days (mean 8.6 days (SD 4.5)) after the accident. The response rate was approximately 33%. The control group comprised 53 matched controls. Baseline characteristics of the study and control group are shown in Table I. The circumstances of an accident are summarized in Table II. ANOVA analysis revealed that the circumstances of an accident did not significantly influence the severity of WAD symptoms, except for the sitting location of the victim; sitting in the driver’s seat or front passenger seat more often resulted in second-grade WAD in the study population compared with other sitting positions (p < 0.05).
|
Table I. Baseline characteristics of whiplash-associated disorder (WAD) and control group. Nominal data is presented by number of participants/group and in percentage. Interval data is presented by mean and standard deviation (SD). Nominal data (genus, education, employment status) was compared using the χ2 test, and interval data (age and body mass index (BMI)) using t-test. No statistical difference was found between the groups |
|||
|
WAD (n = 50–71) |
Controls (n = 49–53) |
||
|
Age, years, mean (SD) Gender, n (%) Men Women |
33.5 (13.3) 27 (38) 44 (62) |
31.4 (11.8) 20 (37.7) 33 (62.3) |
|
|
Education, n (%) Secondary Professional University |
32 (45.7) 14 (20) 24 (34.3) |
20 (37.7) 10 (18.9) 23 (43.4) |
|
|
Employment status, n (%) Employed Unemployed Not working Students Employed students |
46 (64.8) 6 (8.5) 4 (5.6) 11 (15.5) 4 (5.6) |
32 (60.4) 1 (1.9) 2 (3.8) 14 (26.4) 4 (7.5) |
|
|
BMI, mean (SD) |
24.3 (4.7) |
24.1 (4.2) |
|
|
Table II. Details of the accident (n = 71) |
|
|
Variable |
n (%) |
|
Type of vehicle Car Minibus |
67 (94.4) 4 (5.6) |
|
Collision direction Front Back Driver’s side Passenger’s side Other Do not know |
14 (19.7) 29 (40.8) 10 (14.1) 14 (19.7) 1 (1.4) 3 (4.2) |
|
Was the vehicle moving or standing still? Moving Standing still |
52 (73.2) 19 (26.8) |
|
Estimated driving speed, km/h Mean (SD) Min – max values |
39.4 (33.6) 0–170 |
|
Did the vehicle turn over? Yes No Do not know |
5 (7) 65 (91.5) 1 (1.4) |
|
Was it possible to use a vehicle after the accident? Yes No Do not know |
20 (28.2) 45 (63.4) 6 (8.5) |
|
Sitting position of victim Driver’s seat Passenger’s front seat Left seat in the back Right seat in the back Middle seat in the back |
41 (57.7) 17 (23.9) 4 (5.6) 6 (8.5) 3 (4.2) |
|
Did you wear a seat belt? Yes No Do not know |
52 (73.2) 16 (22.5) 3 (4.2) |
|
Did you have a head rest? Yes No Do not know |
52 (73.2) 17 (23.9) 2 (2.8) |
|
Did you lose consciousness during the accident? Yes No Do not know |
12 (16.9) 56 (78.9) 3 (4.2) |
|
Did you experience head contusion? Yes No Do not know |
31 (43.7) 34 (47.9) 6 (8.5) |
Degree of whiplash-associated disorder and symptoms according to the Quebec Task Force questionnaire
WAD symptoms were considered as new symptoms that had not been noted before the accident. Table III summarizes the symptoms experienced by the patients after the accident and the symptoms experienced by the controls. According to the physical examination and Quebec Task Force Classification, 66 of 71 (93%) patients developed acute WAD symptoms. Fifteen patients (21.1%) showed symptoms and signs determined as grade I, 48 (67.6%) as grade II, and 3 (4.2%) as grade III. WAD patients complained significantly more frequently of neck/shoulder pain, headache, reduced/painful neck and jaw movements, numbness/tingling or pain in the arms/hands, dizziness, nausea/vomiting compared with controls (Table III). There was no significant difference in the distribution of WAD grades I–III when studied by gender. Nevertheless, females were likely to be diagnosed with any WAD grade than males, since grade 0 (or no WAD) was more common among male patients.
|
Table III. Self-rated symptoms of whiplash-associated disorder (WAD) and control group according to the Quebec Task Force Questionnaire. Data are presented as number of patients (percentage) |
||
|
WAD symptoms |
WAD (n = 71) n (%) |
Control group (n = 53) n (%) |
|
Neck/shoulder pain |
54 (76.1)*** |
11 (20.8) |
|
Reduced/painful neck movements |
39 (54.9)*** |
6 (11.3) |
|
Headache |
42 (59.2)** |
16 (21.2) |
|
Reduced/painful jaw movements |
6 (8.5)* |
0 (0) |
|
Numbness/tingling or pain in arms/hands |
25 (35.2)** |
5 (9.5) |
|
Numbness/tingling or pain in legs/feet |
15 (21.1) |
9 (17.0) |
|
Dizziness/unsteadiness |
42 (59.2)*** |
5 (9.4) |
|
Nausea/vomiting |
13 (18.3)*** |
1 (1.9) |
|
Difficulty/swallowing |
4 (5.6) |
0 (0) |
|
Tinnitus |
12 (16.9) |
7 (13.2) |
|
Memory problems |
13 (18.3) |
6 (11.3) |
|
Concentration problems |
14 (19.7) |
6 (11.3) |
|
Vision problems |
10 (14.1) |
7 (13.2) |
|
Lower back pain |
19 (26.8) |
18 (34.0) |
|
*Indicates statistically significant difference between WAD vs control group (*p < 0.05, **p < 0.001 and ***p < 0.001, Mann-Whitney U test). |
||
Pain, neck range of motion and Disability Rating Index
Pain intensity and pressure pain thresholds were compared between the patient and control groups. After the accident patients experienced more intense pain according to VAS and had a significantly reduced pain threshold for pressure of the mean points score in the upper part of the body as well as in the lower leg muscles compared with controls (Table IV). However, there was no significant difference in the mean pressure pain threshold score in the upper body region between WAD grades (data not shown). When comparing neck ROM separately, a significant reduction was found in forward flexion, right and left lateral flexions. The total ROM was also significantly reduced in patients’ group. The patient group also had higher DRI compared with controls (Table IV).
The total ROM and separate neck ROM did not differ significantly between genders in the patient group, except for left rotation that was significantly reduced among females (data not shown).
ANOVA revealed that the higher WAD grade was linked to the greater reduction in neck flexion and total ROM (p < 0.05) and more prominent pain in the neck according to QTFQ (p < 0.01), but not to any other characteristics of the patients.
Health status, Cognitive Failures Questionnaire and Hospital Anxiety and Depression Scale
Patients had worse general health status compared with controls after the accident (Table IV). Cognitive impairment (CFQ ≥ 43) was found in 11 respondents in the patient group (maximum up to 65) and in 5 controls (maximum up to 57); however, there was no statistically significant difference between those 2 groups (Table IV). Anxiety disorders (HADS for anxiety ≥ 10) were suspected in 17 patients and 5 controls, while the risk of depressive disorders (HADS for depression ≥ 10) was found in 3 patients and 2 controls. In addition, the means of HADS for anxiety and depression differed significantly between the patient and control groups (Table IV).
|
Table IV. Data on pain intensity, pain pressure threshold, Disability Rating Index (DRI), range of motion (ROM), general health status, cognitive functioning (CFQ) and emotional status (HADS) |
||
|
Characteristic |
WAD (n = 71) |
Controls (n = 53) |
|
Pain intensity, VAS, mm, mean (SD) [median; IQR] |
44.4 (24.0)*** [49; 26–63] |
10 (14.1) [3.5; 0–15.0] |
|
Pain threshold, kg/cm2, mean (SD) [median; IQR] Upper part of the body Lower leg muscles |
2.87 (1.21)* [2.56; 1.94–3.77] 3.22 (1.67)* [2.95; 2.16–3.98] |
3.71 (1.69) [3.05; 2.47–4.97] 5.62 (3.32) [4.7; 3.03–7.28] |
|
ROM, cm, mean (SD) Flexion Extension Right lateral flexion Left lateral flexion Right rotation Left rotation Total sum of all ROM |
10.82 (3.25)*** 6.71 (2.46) 5.32 (2.1)** 5.5 (2.49)*** 10.06 (2.86) 9.81 (2.93) 48.2 (10.02)*** |
13.61 (3.07) 7.45 (2.28) 6.68 (2.3) 7.35 (2.63) 10.73 (1.78) 10.68 (2.01) 56.5 (7.31) |
|
Total DRI, mean (SD) [median; IQR] |
367.7 (302.1)*** [324; 112–550] |
43.3 (56.9) [23; 0–61.5] |
|
General health status, VAS, mm, mean (SD) [median; IQR] |
34.7 (21.0)*** [33.5; 15.75–52] |
12.3 (13.8) [8; 3.5–17.5] |
|
CFQ, mean (SD) |
31.4 (11.6) |
28.4 (10.4) |
|
HADS, mean (SD) [median; IQR] Anxiety Depression |
7.2 (3.7)* [7; 4–9] 3.3 (2.8)** [3; 1–5] |
5.2 (3.3) [4; 2.5–7] 2.3 (2.8) [1; 0–3] |
|
*Indicates statistically significant difference between WAD and control group (*p < 0.05, **p < 0.01 and ***p < 0.001, t-test for ROM and CFQ and Mann-Whitney U test for pain intensity, pain pressure threshold, DRI, general health status and HADS). WAD: whiplash-associated disorder; SD: standard deviation; IQR: interquartile range. |
||
Discussion
The results of the present study indicate that 66 (93%) of the patients developed acute WAD symptoms after traffic collision, and the majority of them (67.6%) met grade II criteria. This is in line with the results of Girotto et al. (16), who reported that almost 90% of more than 1,000 people with neck injuries registered in the emergency department developed WAD (grades II and III) according to the Quebec Task Force criteria and clinical examination. The most frequent WAD symptoms found in our study were neck or shoulder pain, reduced or painful neck movements, headache and dizziness. These symptoms, as well as reduced/painful jaw movements, numbness/tingling or pain in upper and lower limbs, nausea/vomiting were significantly more common in the patient group than among the controls. WAD patients had significantly lower pressure pain threshold and reduced forward, right and left lateral flexions, as well as total ROM compared with controls. In comparison with controls, the patient group had higher disability, worse general health status, more intensive pain and higher HADS scores. The higher WAD grade was linked to the greater reduction in neck flexion and total ROM as well as more prominent pain in the neck. The results of the clinical objective and subjective findings in the present study are in line with other studies on WAD (17–19) and indicate the acute multiple symptoms presented. However, these results differ from the study published by our colleagues in 1999, in which less than half of road traffic accident victims had acute pain with only mild or moderate intensity (20). The difference could be explained by the different modes of recruitment and different topics addressed in the studies (neck pain/headache vs WAD symptoms). The participants of the latter study were surveyed by postal questionnaires asking precisely about the features of neck pain and headache, while in the present study questions regarding WAD symptoms were followed by a detailed clinical examination.
The response rate in our study was only 33%, which is a limitation and should be considered as a selection bias. During phone calls we frequently registered excuses, such as “I don’t have time”, “I don’t see the point of participating”, “I am feeling healthy”, etc. The low participant rate may also be due to the lack of WAD symptoms, which, at least if they persisted, probably did not worry the patient. The following efforts were made to attract the participants: personal invitation by phone to attend a qualified clinical examination by a doctor at University Hospital and a minor financial encouragement. On the other hand, it is also important to note that clinical research studies involving patients with no clear damage or hospitalization are not so common among Lithuanians, making the procedure of recruitment even more challenging. We also found a discrepancy between patient’s common perception of his/her health situation and symptoms found during clinical examination (not presented in this study), an interesting aspect in order to understand the role of expectations and awareness in WAD-phenomenon. The low participant rate is partially explained by the fact that patients were not concerned about their health after the accident due to suggested unawareness of WAD and/or lack of expectations for persistent symptoms, as demonstrated in the previous report (7).
According to the Quebec Task Force definition of “whiplash-related injury” (2), it may result from rear-end or side-impact motor vehicle collisions. In our study there were 4 main mechanisms of accident: rear-end and vice versa, and impact from the driver’s or passenger’s side. The mechanism of an accident itself did not significantly influence the development of WAD or severity of its symptoms, while the exact sitting location of the victim (driver’s seat or passenger’s front seat) was related to the second grade of WAD.
In conclusion, the most frequent WAD symptoms found in the Lithuanian population, which is presumed to be unaware of WAD, were neck or shoulder pain, reduced or painful neck movements, headache and dizziness. These results confirm the fact that acute WAD symptoms should be considered as an entity per se and require proper treatment, as well as follow-up, in order to affect the maintenance of the symptoms and prevent development of persistent WAD. Further studies are planned to understand the processes and predictors for long-term symptoms in the Lithuanian population after road traffic accidents.
Acknowledgements
This study has been supported by grants from The Swedish Institute (The Visby Programme) and The Swedish Cancer and Traffic Injury Fund (CTRF).
References
