Agnes F. Hoeksma, MD, PhD1, Marion A. J. van Rossum, MD, PhD2,3, Wilma G. W. Zinger, MD1, Koert M. Dolman, MD, PhD2,4, Joost Dekker, PhD1,5 and Leo D. Roorda, MD, PT, PhD1
From the 1Amsterdam Rehabilitation Research Center and 2Jan van Breemen Research Institute, Reade, 3Department of Paediatric Rheumatology, Emma Children’s Hospital, Academic Medical Center, 4Department of Rheumatology, Sint Lucas Andreas Hospital and 5Department of Rehabilitation Medicine, VU University Medical Center, Amsterdam, The Netherlands
OBJECTIVE: To determine the prevalence of hand- and wrist-related symptoms and impairments, with resulting activity limitations and participation restrictions in children being treated for juvenile idiopathic arthritis.
Design and patients: Cohort study of children, diagnosed in our hospitals between 2003 and 2008 with juvenile idiopathic arthritis, who received standard treatment with regular follow-ups in the same institutions. Patients were asked about hand and wrist symptoms, and underwent a standardized physical examination. For activity limitations, they were asked to complete the Dutch version of the Childhood Health Assessment Questionnaire (CHAQ). Concerning participation restrictions, children were asked about any hand- and/or wrist-related difficulties during daily activities.
RESULTS: Of all 152 eligible patients, 121 (80%) participated in the study; 34 boys and 87 girls, mean age 13.7 years (standard deviation (SD) 4.2), mean disease duration 2.6 years (SD 1.4), mean Juvenile Arthritis Disease Activity Score in 71 joints (JADAS-71) score 8 (SD 8), indicating low disease activity. Of these 121, 84 (69%) had at least 1 symptom and 40% had at least 1 impairment. The median CHAQ-total score was 0.5 (mean 0.75 (SD 0.77)), indicating mild-to-moderate activity limitations; and 54% reported having hand- and/or wrist-related problems at school.
CONCLUSION: Despite low disease activity, many children appeared to have hand- and/or wrist-related symptoms and impairments, with resulting moderate to severe levels of activity limitations and participation restrictions at school.
Key words: juvenile idiopathic arthritis; JIA; hand; wrist; symptoms; impairments; activity-limitations; participation-restrictions.
J Rehabil Med 2014; 46: 00–00
Correspondence address: Leo D. Roorda, Rehabilitation Medicine, Amsterdam, Rehabilitation Research Center, Reade, 1040 HG Amsterdam, The Netherlands. E-mail: l.roorda@reade.nl
Accepted May 26, 2014; Epub ahead of print Sep 3, 2014
Introduction
Juvenile idiopathic arthritis (JIA) is the most common form of arthritis in children (1). European studies have shown that prevalence varies between 16 and 150 per 100,000 children (2). JIA is described as arthritis in 1 or more joints, which starts before the age of 16 years, lasts for at least 6 weeks, and has no other apparent cause (3). Seven different categories of JIA can be distinguished; systemic arthritis, oligoarthritis (subcategories: persistent or extended), rheumatoid factor negative (RF–) polyarthritis, rheumatoid factor positive (RF+) polyarthritis, psoriatic arthritis, enthesitis-related arthritis and undifferentiated arthritis (4). In general, JIA affects more girls than boys.
Early involvement of the hand and wrist has been described, and in approximately 80% of all cases of JIA, hand arthritis will eventually develop (5). It can occur in all subcategories of JIA, but is most often seen in systemic arthritis, extended oligoarthritis, RF– polyarthritis, RF+ polyarthritis and psoriatic arthritis (6).
In the hand and wrist, synovitis and tenosynovitis are the first symptoms that may eventually result in destruction of joints, laxity of ligaments and imbalance of muscle function. As this process progresses, impairments reinforce one another in such a way that eventually serious deformities may develop and lead to limitations in activities of daily living. There is little information about the prevalence of hand- and wrist-related symptoms (i.e. pain or stiffness) and impairments (i.e. problems in body function or structure, such as limitation of the range of motion (ROM)), and their resulting activity limitations (i.e. difficulties in handwriting) and participation restrictions (i.e. problems with involvement in life situations, such as attending school) (7) in JIA. In order to provide optimal pharmacological and non-pharmacological care, it is important to gain insight into the clinical features of the hand and wrist after appropriate pharmacological care.
The aim of the study was therefore to determine the prevalence of hand- and wrist-related symptoms and impairments, and their resulting activity limitations and participation restrictions in children being treated for JIA.
Patients and methods
Patients
We studied the complete patient population of the Paediatric Rheumatology Departments of Reade and the Emma Children’s Hospital at the Academic Medical Center (AMC), both in Amsterdam, The Netherlands. Inclusion criteria were: (i) to have been diagnosed with JIA in accordance with the International League of Associations for Rheumatology (ILAR) (3) at 1 of these institutions between January 2003 and January 2008; (ii) to have received standard care at 1 of these 2 institutions since the diagnosis; and (iii) to have attended regular follow-ups at these departments during this study, between October 2006 and March 2010. Exclusion criteria were; serious cognitive impairment and if there was a language barrier precluding the interview and questionnaire. All participants and their parents gave written informed consent. Patients who met all inclusion criteria, but could not be invited for the study or who refused informed consent, were noted as non-participants. The study protocol was approved by the local medical ethics committee.
Procedure
During a routine appointment at the Department of Paediatric Rheumatology, a standardized physical examination of the hand and wrist was performed by a paediatric rheumatologist. The children (for children ≥ 10 years of age) or the parents (for children < 10 years of age) were asked to complete the Dutch version of the Childhood Health Assessment Questionnaire (CHAQ). Within 1 week of this consultation, children (for children ≥ 10 years of age) or the parents (for children < 10 years of age) were contacted at home by telephone by an independent researcher, in order to collect information about hand- and wrist-related symptoms, activity limitations and participation restrictions (see below).
Measurements
Demographic and disease characteristics. Data on age, gender, age at onset, disease duration, ILAR classification, and use of medication were obtained from the medical records. Disease activity (signs and symptoms related to inflammation) was assessed using the Juvenile Arthritis Disease Activity Score in 71 joints (JADAS-71), a recently validated composite disease activity score for JIA. This score is based on: (i) self-reported or parent-reported global assessment of well-being; (ii) doctor-reported global assessment of disease activity; (iii) doctor-reported number of active joints count; and (iv) erythrocyte sedimentation rate (ESR) (8). The self-reported or parent-reported global assessment of well-being during the previous week, was rated on a 100-mm visual analogue scale (VAS) (VAS well-being) range 0–100 (0 = very good; 100 = very poor). The doctor-reported global assessment of disease activity was rated by a paediatric rheumatologist on a 100-mm VAS (VAS disease activity) range 0–100 (0 = no disease activity; 100 = severe disease activity). Overall pain in the previous week was assessed during the consultation on a 100-mm VAS pain (0 = no pain; 100 = most severe pain). A joint examination was performed by a paediatric rheumatologist. An active joint was defined as a joint with swelling not due to bony enlargement or, if no swelling was present, limitation of motion accompanied by either pain on motion or tenderness (9). Active joints (0–71) were assessed in this way, according to the core set of outcome variables in JIA (10). The blood samples for the calculation of the ESR were taken on the same date as the appointment at the outpatient clinic. The JADAS-71 was calculated in accordance with the recommendations in the literature, resulting in a score ranging from 0 to 101, with 101 indicating high disease activity (8).
Symptoms. The patients or their parents were asked in a structured way whether they experienced any hand-related problems and any wrist-related problems, and, if they did, whether they experienced any pain, stiffness, muscle weakness, paraesthesia, limited fist function, limited pinch grip, any joint deviation, aesthetic complaints, or any other symptoms; followed by the questions “do you use any device such as an adapted knife, pencil, laptop or other devise” and “do you use any hand or wrist braces or splints”. They were also asked to indicate their main symptom on the dominant and the non-dominant hands.
Impairments. A standardized physical examination of the hand and wrist was performed to test for joint range of motion (ROM), any dislocation or deviation of joints, tendon-gliding, signs of synovitis and tenosynovitis, and signs of tendon rupture or muscle weakness. Joint ROM was considered to be impaired if the passive measurement was ≥ 15° less than the normal values (11, 12). Involvement of the first carpometacarpal (CMC-1) joint was scored positive if passive motion of this joint was painful, and if the CMC-1 joint was prominent during inspection of the hand contour. Z-deformity of the thumb was scored positive if, on inspection, there was a flexed first metacarpophalangeal (MCP-1) joint and a hyperextended interphalangeal joint that could not be actively corrected. Flexor-tendon gliding was graded with the Amsterdam Severity Scale in Stenosing Tenosynovitis (ASSiST, range 0–3) (13). Tenosynovitis ≥ grade 2 was considered to indicate impairment, in which a perceptible click or a reduced tempo of active finger flexion could be observed, in combination with a full active range of motion (aROM) (determined by the passive range of motion (pROM)). A swollen extensor tendon sheath on palpation was interpreted as tenosynovitis in this tendon.
Activity limitations. To measure activity limitations, the children or their parents were asked to complete the Dutch version of the Childhood Health Assessment Questionnaire (CHAQ) (14–17). The CHAQ assesses 8 functional areas (dressing, arising, eating, walking, hygiene, reaching, grip and activities) with a score ranging from 0 to 3 (0 = without any difficulty; 1 = with some difficulty; 2 = with much difficulty; 3 = not possible). For each item a “not applicable” option is available for patients with age-related limitations in performing an activity. The question with the highest score determines the score in that functional area. If aids or devices are used or help is needed to complete tasks in a certain area, a minimum score of 2 is recorded for the corresponding functional area. The scores of each of the 8 functional areas are averaged to calculate the CHAQ-disability index (CHAQ-DI), which ranges from 0 (no or minimal physical dysfunctioning) to 3 (very severe physical dysfunctioning). In addition to the CHAQ-DI, the sub-score for grip (CHAQ-grip) was analysed separately, because the focus of the study was on hand- and wrist-related activity limitations.
Participation restriction. The children or their parents were asked about their daily occupations: school or study, work and hobbies. In each sub-category, they were asked whether they experienced any hand- or wrist-related difficulties (yes/no) while carrying out these occupations, or if they had had to discontinue any of these occupations (yes/no) because of hand- or wrist-related problems. We scored an item as a problem when a child reported any difficulty in a category or when he or she had had to stop this occupation because of hand- or wrist-related problems.
Statistical analysis
All analyses were performed in SPSS (version 19.0). Descriptive statistics were reported in terms of mean with standard deviations (SD) for continuous variables with normal distribution, and medians with interquartile ranges (IQR) for not-normally distributed continuous and non-continuous variables. Comparisons between participants and non-participants were calculated using the Pearson’s χ2. Correlations were quantified using the Spearman correlation test. Two-sided p-values ≤ 0.05 were considered as statistically significant. To calculate any potential relationships between the JIA subtypes, we compared 3 groups: the 2 largest groups (persistent oligoarthritis and RF– polyarthritis, including extended oligoarthritis) with the other JIA subtypes.
Results
Patients
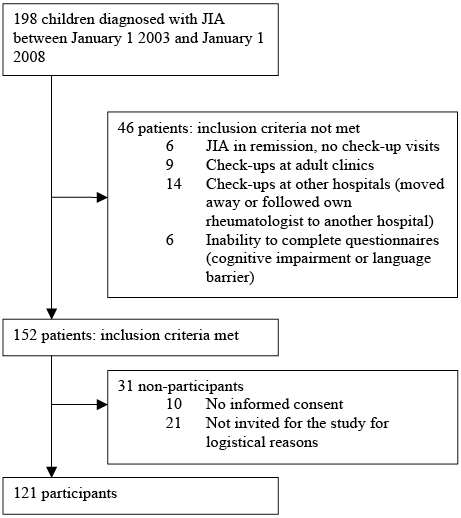
Between January 2003 and January 2008, JIA was diagnosed in 198 children, of whom 152 met all our inclusion criteria (see Fig. 1). Of the 152 patients, 121 (80%) participated in the study (34 boys and 87 girls, mean age 13.7 years (SD 4.2), mean disease duration 2.6 years (SD 1.4), mean JADAS-71 score 8 (8), i.e. low disease activity). The demographics and clinical characteristics of the participants and non-participants are summarized in Table I.
|
Table I. Demographic and disease characteristics of 121 participants and 31 non-participants |
|||
|
Participants (n = 121) |
Non-participants (n = 31) |
p-value |
|
|
Gender, male/female, n |
34/87 |
16 /15 |
0.013* |
|
Right/left dominance, n |
106/15 |
||
|
Age at study visit, years, mean (SD) |
13.7 (4.2) |
13.2 (4.3) |
0.572 |
|
Age at disease onset, years, mean (SD) |
11.0 (4.2) |
9.9 (4.5) |
0.165 |
|
Disease duration, years, mean (SD) |
2.6 (1.4) |
3.4 (1.9) |
0.053 |
|
JIA sub-type, n (%) |
0.603 |
||
|
Systemic |
– |
– |
|
|
Oligoarticular persistent Oligoarticular extended |
23 (19) 14 (12) |
7 (23) 2 (7) |
|
|
Polyarticular RF– |
7 (6) |
1 (3) |
|
|
Polyarticular RF+ |
64 (53) |
20 (65) |
|
|
Psoriatic |
7 (6) |
– |
|
|
Enthesitis-related |
6 (5) |
1 (3) |
|
|
Undifferentiated |
– |
– |
|
|
Medication, n (%) |
0.309 |
||
|
No medication |
7 (6) |
4 (13) |
|
|
Only NSAIDs |
12 (10) |
1 (3) |
|
|
DMARDs |
85 (70) |
20 (65) |
|
|
Biological DMARDs |
17 (14) |
6 (19) |
|
|
Disease activity |
|||
|
Self-reported or parent-reported, median (IQR) |
|||
|
VAS well-being (0–100)a |
14 (0–47) |
||
|
CHAQ: VAS-Pain last week 0–100a |
12 (0–50) |
||
|
Doctor-reported, median (IQR) |
|||
|
VAS disease activity (0–100)a |
10 (0–23) |
10 (0–25) |
0.882 |
|
Number of active joints whole body (0–71) |
2 (0–5) |
3 (0–5) |
0.848 |
|
ESR (mm/h), median (IQR) |
6 (3–13) |
5 (2–9) |
0.177 |
|
JADAS-71 (0–101), mean (SD) |
8 (8) |
||
|
aHigher scores indicate worse situation. *Participants vs non-participants: significant if p < 0.05. NSAIDs: non-steroidal anti-inflammatory drugs; SD: standard deviation; IQR: interquartile range; JIA: juvenile idiopathic arthritis; DMARDs: non-biological disease-modifying anti-rheumatic drugs, including methotrexate, prednisone and sulfasalazine. Biological DMARDs, including etanercept, infliximab and adalimumab: with or without non-biological DMARD. CHAQ: Childhood Health Assessment Questionnaire; VAS: visual analogue scale; ESR: erythrocyte sedimentation rate; JADAS-71: Juvenile Arthritis Disease Activity Score in 71 joints. |
|||
Symptoms
Current symptoms, as well as the main symptom in the dominant and the non-dominant hands, are summarized in Table II. More than two-thirds of the children reported symptoms in the hands and/or wrists (69%), most frequently in the hands (55%) but also often in the wrists (49%); and most frequently on the dominant side. The most frequently reported symptom was pain (53%). When divided into handedness: 64% of the patients reported symptoms within the dominant hand and 53% in the non-dominant hand.
|
Table II. Hand- and/or wrist-related symptoms of participants (n = 121) |
|||
|
Symptom present n (%) |
Main symptom |
||
|
Dominant side n (%) |
Non-Dominant side n (%) |
||
|
Any symptom hands and/or wrists |
84 (69) |
||
|
Any symptom hands |
67 (55) |
||
|
Any symptom wrists |
59 (49) |
||
|
Pain |
64 (53) |
47 (39) |
36 (30) |
|
Stiffness |
50 (41) |
12 (10) |
11 (9) |
|
Experienced less grip force |
52 (43) |
7 (6) |
7 (6) |
|
Paraesthesia |
24 (20) |
6 (5) |
4 (3) |
|
Limited fist function |
21 (17) |
1 (1) |
– |
|
Deviated fingers or wrist |
18 (15) |
2 (2) |
2 (2) |
|
Cosmetic problems |
12 (10) |
||
|
No symptoms |
43 (36) |
57 (47) |
|
Impairments
Impairments in both sides together as well as divided into handedness, are shown in Table III. Impairments of hands and/or wrists were detected in 40%; in the hands in 40% and in the wrists in 30%; most frequently on the dominant side. Restricted ROM was more often seen in the wrists than in the hands. However, in general, impairments were more commonly noted in the hands than in the wrists. Involvement of proximal interphalangeal (PIP) joints was more frequently noted than impairments of the MCP joints. Tenosynovitis, intrinsic tightness, Boutonniere deformity and reduced grip force were not frequently present. Swan-neck deformity, subluxation or deviation of finger joints, Z-thumb or tendon ruptures were not observed.
|
Table III. Impairments of participants (n = 121) |
|||
|
One or both sides n (%) |
Dominant side n (%) |
Non-dominant side n (%) |
|
|
Any impairment hands and/or wrists |
48 (40) |
||
|
Impairments wrists |
|||
|
Any impairment wrists |
35 (30) |
31 (26) |
21 (17) |
|
Arthritis wrist |
28 (23) |
25 (21) |
15 (12) |
|
Restricted ROM wrist |
27 (22) |
25 (21) |
14 (12) |
|
Impairments hands |
|||
|
Any impairment hands |
48 (40) |
44 (36) |
37 (31) |
|
Arthritis in any hand joint |
18 (15) |
18 (15) |
12 (10) |
|
Restricted ROM ≥ 1 MCP |
10 (8) |
10 (8) |
5 (4) |
|
Restricted ROM ≥ 1 PIP |
21 (17) |
20 (17) |
16 (13) |
|
Restricted ROM ≥ 1 DIP |
6 (5) |
4 (3) |
5 (4) |
|
Stenosing tenosynovitis flexor tendons |
1 (1) |
1 (1) |
– |
|
Tenosynovitis extensor tendons |
3 (3) |
3 (3) |
2 (2) |
|
Intrinsic tightness |
1 (1) |
– |
1 (1) |
|
≥ 1 Boutonniere deformity |
2 (2) |
2 (2) |
– |
|
Reduced grip force |
5 (4) |
5 (4) |
5 (4) |
|
ROM: range of motion; MCP: metacarpophalangeal joint; PIP: proximal interphalangeal joint; DIP: distal interphalangeal joint. |
|||
Activity limitations
Activity limitations, expressed with the CHAQ with its sub-item CHAQ-grip, and the widespread use of braces or devices are described in Table IV. The median CHAQ total score was 0.5 (IQR 0.0–1.25; mean 0.75 (SD 0.77)), the median subcategory CHAQ-grip 0.0 (IQR 0.0–2.0; mean 0.88 (SD 0.98)). Forty-five children (37%) reported the use of braces or splints (mostly wrist braces), and 52 (43%) indicated the use of devices such as an adapted knife, pencil or laptop.
|
Table IV. Activity limitations and participation restrictions of participants (n = 121)* |
|
|
Activity limitations |
|
|
Self-reported or parent-reported |
|
|
CHAQ total score (0–3) |
|
|
Median (IQR) mean (SD) |
0.5 (0.0–1.25) 0.75 (0.77) |
|
CHAQ-grip (0–3) |
|
|
Median (IQR) mean (SD) |
0.0 (0.0–2.0) 0.88 (0.98) |
|
Use of braces/splints, n (%) |
45 (37) |
|
Use of devices (adapted knife, pencil, laptop), n (%) |
52 (43) |
|
Participation restrictions, n (%) |
|
|
Self-reported or parent-reporteda |
|
|
Hand- and/or wrist-related problems at school |
61 (54) |
|
Hand- and/or wrist-related problems in sports/hobbies |
36 (30) |
|
Hand- and/or wrist-related problems during work (weekend job) |
10 (27) |
|
aWe scored an item as a problem when a child reported any difficulty in a category or when he or she needed to stop this occupation because of hand- or wrist-related problems. CHAQ: Childhood Health Assessment Questionnaire; SD: standard deviation; IQR: interquartile range. |
|
Participation restrictions
Self-reported hand- and wrist-related problems at school, in sports/hobbies or during work/weekend job, are described in Table IV. Almost one-third of the children reported that they experienced hand- or wrist-related problems during hobbies and work, or that they needed to stop these occupations because of this. And more than half of the children reported hand- or wrist-related problems at school.
Relationships
Relationships between hand- and/or wrist-related symptoms, impairments, activity limitations and participation restrictions on the one hand, and JIA-subtypes on the other hand, are described in Table V. A relationship was shown only between wrist-related symptoms and problems at school, with higher incidences in RF– polyarthritis and lower incidences in oligoarthritis.
No significant relationships between the above items and disease duration, age at diagnosis and actual age could be found. Furthermore, these items were not statistically significant different between male and female patients.
|
Table V. Relationshipsa between hand- and/or wrist-related symptoms, impairments, activity limitations and participation restrictions on the one hand, and JIA-subtype on the other hand |
||||
|
Variables |
JIA-subtypes |
pa |
||
|
Oligoarthritisb n = 23 n (%) |
RF- polyarthritisc n = 77 n (%) |
Other subtypesd n = 21 n (%) |
||
|
Any symptom |
||||
|
Hands and/or wrists |
8 (35) |
48 (62) |
11 (52) |
0.065 |
|
Hands |
8 (35) |
48 (62) |
11 (52) |
0.065 |
|
Wrists |
5 (22) |
42 (55) |
11 (52) |
0.016* |
|
Any impairment |
||||
|
Hands and/or wrists |
5 (22) |
36 (48) |
7 (33) |
0.098 |
|
Hands |
5 (22) |
36 (48) |
7 (33) |
0.098 |
|
Wrists |
4 (17) |
24 (31) |
7 (33) |
0.372 |
|
CHAQ-gripe |
4 (17) |
24 (31) |
7 (33) |
0.372 |
|
Problems at school, hand- and/or wrist- related |
6 (26) |
48 (62) |
7 (33) |
0.004* |
|
aPearson’s χ2. bJIA oligoarthritis: oligoarthritis persistent. cJIA RF: polyarthritis including extended oligoarthritis. dOther subtypes: including RF+ polyarthritis, psoriatic arthritis and enthesitis-related arthritis. eCHAQ-grip: sub-score for grip in the Childhood Health Assessment Questionnaire. *p < 0.05. JIQ: juvenile idiopathic arthritis. |
||||
Discussion
The aim of this study was to determine the prevalence of hand- and wrist-related symptoms and impairments, and their resulting activity limitations and participation restrictions in a cohort of well-controlled JIA patients.
Sixty-nine percent of the children reported having symptoms in the hands and/or wrists, when specifically asked about them, 64% on the dominant side and 53% on the non-dominant side. Pain in the hands and/or wrists was present in more than half of the children, and was most often indicated as the main symptom, followed by reports of stiffness. More children reported symptoms than impairments were recognized on physical examination. This is in contrast with our clinical practice, in which children tend to report fewer problems during history-taking than are recognized on physical examination, as confirmed by the study of Goff (18). Under-reporting of problems can lead to functional disability, via suboptimal treatment and is therefore a serious issue.
The prevalence of impairments in the hands and wrists was very high. The distribution over the hands and wrists was in line with 2 other studies on clinical symptoms of the wrist and finger joints (6, 19). Compared with hand impairments in rheumatoid arthritis (20), stenosing tenosynovitis of the flexor tendons was very infrequently seen. However, this may also be due to the fact that in children stenosing tenosynovitis is difficult to diagnose by physical examination alone. For the detection of (early) tenosynovitis, ultrasound could be a valuable tool (21). In general, there are strong indications that synovitis and tenosynovitis are not always detected on physical examination (22–24),
Concerning activity limitations, the median CHAQ total score was 0.5 (mean 0.75 (SD 0.77)), with the subcategory CHAQ-grip of 0.0 (mean 0.88 (SD 0.98)). Recently, the clinical meaning of the CHAQ has been studied: mild, mild-to-moderate and moderate disability corresponded with CHAQ scores of 0.13, 0.63 and 1.75, respectively (25). Ruperto et al. divided the CHAQ into 4 categories of activity limitation: 0 = none, 0.1–0.5 = mild, 0.6–1.5 = moderate, and > 1.5 = severe (26). However, Hyrich et al. indicated that a CHAQ ≥ 0.75 is moderate to severe disability (27). Using all these different descriptions, we categorized our CHAQ total score as moderate disability. This finding is comparable with the findings of Gutierrez et al. (28). The CHAQ-grip, median 0.0, mean 0.88 (SD 0.98), can be described as follows: half of the children reported no disability in handgrip, and the other half reported severe disability in handgrip. The high frequency of the reported use of braces (37%) and devices (43%) was surprising. In our clinic, all children with JIA are advised to use braces in the occurrence of pain or swelling of the wrists during activities. However, we observe that most children resist wearing them. Only when they are very troubled by their complaints do we notice that they are using the braces. In this study, we asked whether the child was actually using braces. Therefore, we estimate this as an indication as to whether the child is experiencing complaints. We could not find any data on these items in the literature to compare with our results.
At the level of participation restriction, more than half of the children reported hand- and/or wrist-related problems at school. We examined this problem in a previous study on handwriting difficulties in JIA (29). In this study handwriting difficulties with restrictions at school were attributed to pain and the inability to sustain writing for a long period of time.
Exploration of a possible correlation between hand- and wrist-related symptoms, impairments, activity limitations and participation restrictions on the one hand, and disease duration, age at diagnosis, actual age and gender on the other hand, revealed no correlations. Analysis of the subtypes of JIA only revealed increased prevalence of wrist symptoms and more frequent hand- and/or wrist-related problems at school in RF– polyarthritis patients than in oligoarthritis patients.
Concerning our cohort and our study methods, we have the following comments:
Firstly, we defined our cohort as those children that were diagnosed, treated and monitored unambiguously, and in such a way that participation required minimal effort on the part of the children and their parents. Children were not asked to attend for an extra appointment if they had been discharged from check-ups due to disease remission, if they had their check-ups at adult clinics, or if they had moved away. This could have resulted in an over- or under-estimation of the prevalence.
Secondly, we studied 121 of this cohort of 152 children; a high response rate of 80%.
Thirdly, in the non-participant group, the distribution of gender was significantly different from the participant group. But, because no correlation between gender and symptoms or impairments could be found, we considered that this difference had no influence on the estimated prevalences. There were no other differences between participants and non-participants.
Fourthly, the distribution of gender, medical treatment and data on disease activity of the studied children was in agreement with other recent studies. The mean age at disease onset in our study group was older than described for Western Europe (11.0 vs 5.4 and 6.6 years) (27, 28). However, in the calculation of relationships, age at onset did not influence the outcome. In the JIA subcategories, the group of systemic JIA was underrepresented in our population. In general, systemic JIA can induce severe impairments; therefore this underrepresentation could have caused an underestimation of the prevalences.
Regarding disease activity, minimal disease activity can be defined as a physician global assessment ≤ 25 mm and a swollen joints count of 0 in patients with oligoarthritis; and as a physician global assessment ≤ 34 mm, a parent global assessment ≤ 21 mm and a swollen joints count of ≤ 1 in patients with polyarthritis (30). According to this definition, together with the ESR and JADAS-71, the disease activity status in our study population can be rated as minimal, which is in line with the patient- and parent-reported VAS well-being.
In conclusion, in this cohort of children with JIA there was a high prevalence of hand- and/or wrist-related symptoms and impairments, with resulting moderate to severe levels of activity limitations and participation restrictions at school. The children frequently used braces and devices, despite low levels of disease activity. When looking for relationships, only correlation of wrist symptoms and hand- and/or wrist-related problems at school with the JIA subtypes RF– polyarthritis vs oligoarthritis could be found.
Based on the findings of this study, we recommend that physicians specifically ask about symptoms and screen for hand and wrist impairments on a structural, e.g. yearly, basis.
Acknowledgements
The authors would like to thank J. M. van den Berg, P. Mau-Asam and M. Verrij for their contribution to the data collection.
References
