Thomas Rudolfsson, MSc1,2, Mats Djupsjöbacka, PhD1, Charlotte Häger, PhD2 and Martin Björklund, PhD1,2,3
From the 1Centre for Musculoskeletal Research, University of Gävle, Gävle, 2Department of Community Medicine and Rehabilitation, Umeå University, Umeå and 3Alfta Research Foundation, Alfta, Sweden
OBJECTIVE: To evaluate the effect of neck coordination exercise on sensorimotor function in women with neck pain compared with best-available treatment and sham treatment.
DESIGN: Observer-blinded randomized controlled trial with short-term and 6-month follow-ups.
SUBJECTS: Women with chronic non-specific neck pain were randomized to 3 groups: neck coordination exercise with a novel training device; strength training for the neck and shoulders; or massage. Each group had 36 participants.
METHODS: The intervention period was 11 weeks with 22 individually supervised sessions. Primary outcomes were postural sway measures and precision of goal-directed arm movements. Secondary outcomes were range of motion for the neck, peak speed of axial rotation, and neck pain. A repeated measures multivariate analysis of variance (MANOVA) was conducted separately on the primary outcomes for the short-term and 6-month evaluations and on the sensorimotor secondary outcomes for the 6-month effect. The 6-month effect on pain was analysed with a repeated measures analysis of variance (ANOVA).
RESULTS: No significant treatment effects in favour of neck coordination exercise were found for short-term or 6-month evaluations.
CONCLUSION: Neck coordination exercise is no better than strength training and massage in improving sensorimotor function. Further research should investigate the use of cut-offs for sensorimotor dysfunctions prior to proprioceptive or coordinative training.
Key words: neck pain; rehabilitation; coordination training; resistance training; postural balance; randomized controlled trial.
J Rehabil Med 2014; 46: 908–914
Guarantor’s address: Martin Björklund, Centre for Musculoskeletal Research, University of Gävle, Box 7629, SE-907 12 Umeå, Sweden. E-mail: martin.bjorklund@hig.se
Accepted May 6, 2014; Epub ahead of print Sep 2, 2014
Introduction
Neck pain is a common problem, with an estimated 1-year prevalence of 30–50% (1). The symptoms are often fluctuating and recurrence is common (2). Treatment recommendations for non-specific neck pain usually involve exercise and manual therapy, but our knowledge of treatment is not sufficient (3).
Alongside symptoms of pain and muscle tenderness, neck pain is often accompanied by a deficit in sensorimotor functions (4). These deficits extend beyond the functioning of the cervical spine to include tasks involving eye–hand coordination and postural sway (5–8). The clinical relevance of these laboratory findings has not been thoroughly investigated, but is partly supported by associations between sensorimotor impairments and self-rated functioning (5).
The causality between neck pain and sensorimotor impairments is unknown, but the hypothesis that coordination and proprioceptive exercises are effective for improving neck pain disorders has been tested in short-term evaluations. Neck proprioceptive training has been shown to reduce pain and increase the accuracy of head repositioning (4, 9), while specific coordinative training of the deep cervical flexor muscles has been shown to reduce pain and alter the coordinative muscle activation pattern between deep and superficial neck flexors (10). The long-term effect and transfer to other sensorimotor functions of these interventions are unknown. Transfer to other activities may, however, occur, since neck proprioception may influence the precision of goal-directed arm movements (11, 12) and postural sway (13).
As a further development of sensorimotor interventions, we proposed a novel exercise method for neck coordination training (14). An important aspect of the design was to incorporate theories of motor learning. Previous sensorimotor interventions included closed skills that are predictable to the performer. In contrast, our new approach includes an open skills task to promote neuromuscular problem-solving and levels of progression in order to maintain an adequate level of task difficulty throughout the exercise period (15). In an uncontrolled pilot study (14) the participants participated in 8 training sessions distributed over a 4-week period. They were positive about the method, showed improvement in sensorimotor functions, and reported increased general health and decreased disability.
The overall aim of the present study was to evaluate the short- and long-term effects of the proposed neck coordination exercise on sensorimotor function in people with non-specific neck pain, compared with best-available treatment and sham treatment. Strength training was chosen as the best-available treatment, based on evidence of effect on pain and disability in neck disorders (16–18). Massage was chosen as the sham treatment, based on lack of evidence for long-term effect on pain and disability in neck disorders (19, 20).
We hypothesized that neck coordination exercise had better short- and long-term effects in the form of decreased postural sway and improved end-point precision in goal-directed arm-movements compared with strength training or massage. We further hypothesized that neck coordination exercise had a better long-term effect than massage on cervical range of motion, fast cervical rotations and neck pain.
MethodS
Trial design
The study was an observer-blinded randomized controlled trial with a 3-arm parallel group design, performed in Gävle, Sweden (ISRCTN trial registration number: ISRCTN92199001). Participants with neck pain were randomized to either neck coordination exercise (NCE), strength training (ST) for the neck and shoulder regions, or massage treatment groups. A group of healthy women without neck pain were included for baseline cross-sectional comparison (21, 22). The study was approved by the ethics review board in Uppsala and all participants gave their written consent.
Participants
Subject’s eligibility was verified by a telephone interview, questionnaires and physiotherapy assessment. Inclusion criteria were: Swedish-speaking women, age range 25–65 years, with chronic (> 3 months) non-specific neck pain, assessed by pain drawings of “most painful area” (23). In addition, all participants were required to report disability, measured as > 9 normalized points of the first 19 items in the Disability Arm Shoulder Hand (DASH) questionnaire (24). These items specifically address limitations in performing everyday activities involving the neck, shoulders and arms. Exclusion criteria were: onset or worsening of neck pain associated with trauma to the head and neck, a diagnosis of psychiatric, rheumatic, neurological, inflammatory, endocrine or connective tissue disease, fibromyalgia, cancer, stroke, cardiac infarction or diabetes type I, surgery or fracture to the back, neck, or shoulder in the last 3 years or shoulder luxation in the last year. Finally, participants were excluded if they had performed strenuous exercise > 3 times/week during the last 6 months. If participants reported pain below the shoulders or dizziness, a clinical examination for cervical radiculopathy or vestibular disorders was performed. Positive findings led to exclusion.
Participants were recruited through advertisements in the local papers and by invitations at primary and occupational healthcare units, work sites in the municipality and the county council and via the social insurance agency.
Study settings
Data were acquired in a laboratory setting. The 3 interventions took place in separate buildings, reducing the probability that participants from different groups would communicate with each other. Four physiotherapists, all experienced in the field of neck rehabilitation, led the NCE and ST groups. The massage group was led by 2 certified massage therapists with several years of work experience. All intervention leaders were provided with the same instructions regarding therapeutic approach and attitudes towards the participants. Before the start of the intervention, the physiotherapists completed 8 h of education in the study training programmes.
Interventions
All 3 interventions consisted of 22 individually supervised single-treatment sessions, 30 min each, distributed over 11 weeks within the period August to December 2008.
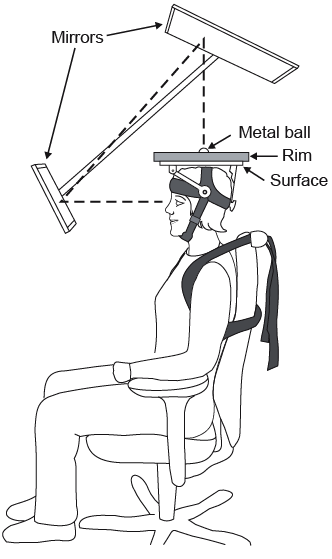
Neck coordination exercise. The NCE was performed with a newly developed training device (patent SE serial # 530879) designed to improve the fine movement control of the cervical spine. For a detailed description of the device and training method, see Röijezon et al. (14). Briefly, the participant wore the training device on their head, fastened with straps around the chin. It consists of a plate with 5 exchangeable surfaces that allow for progression of task difficulty (decreasing rolling resistance). The exercise task, performed in sitting, was to control the movement of a metal ball (weight 220 g) on the plate with the instruction to roll the ball from the starting position to the centre of the plate and hold it still for 3 s. A trial was cancelled if the task was not fulfilled within 45 s. All trials started with instruction to move the ball to a new starting position, indicated by light emitting diodes. Visual feedback with view of the plate from above was provided via mirrors (Fig. 1). A training session comprised 3 blocks with 6 trials each. When the participant successfully completed at least 5 out of 6 trials in a block, the difficulty of the task was increased in the following block by changing to a faster surface. The NCE training consisted of a basic training programme of at least 8 sessions (14) and a progression programme with 12 levels of increasing training dose, task variability and difficulty.
The exercise method has been tested clinically in a vocational rehabilitation centre as well as in our pilot study (14) with no reported adverse effects other than transient tiredness and discomfort in the early phase of the training period, interpreted as a normal post-exercise soreness following unfamiliar exercise. The pilot study supported the clinical applicability of the method, measured as skill acquisition of the task and participants’ positive experience (14).
Strength training. The ST programme targeted the neck and shoulder regions and consisted of isometric and dynamic exercises inspired by the training programme of Ylinen et al. (25). Contraction velocity for the dynamic exercises and frequency of training sessions followed established principles of resistance training (26). The ST session consisted of a 2-min warm-up with slow paced cervical and shoulder movements, 6 strength exercises and ended with a 2-min cool-down.
Three of the 6 exercises were isometric and targeted the neck muscles. The equipment used was a head harness connected to a cable pulley and a training bench with adjustable back support. Two exercises were performed in sitting; while holding the neck stable in relation to the trunk, participants tilted the trunk slightly forward or to the sides. The third was performed in supine position with small rotations of the head (left/right). Isometric contractions were held for 3 s. The dynamic exercises aimed at training the muscles of the shoulder-arm region while stabilizing the neck; seated shoulder press with dumbbells, standing chest press and seated row exercise performed with a straight back.
The first 3 training sessions focused on familiarization with the exercises in which the loading corresponded to participant’s rating of 11–13 (“fairly light” – “somewhat hard”) on the Borg Rating of Perceived Exertion (RPE) scale (27). The dose was 15 repetitions on the isometric exercises and 2 sets of 15 repetitions for the dynamic exercises. At the fourth session, determinations of 1 repetition maximum (1RM) were performed with submaximal tests in each dynamic exercise (28) and with maximal test in the isometric neck flexor exercise (29). Session 5–11 started with a load of 60% of 1RM (RPE ≈ 13) with 2 × 12 repetitions for the dynamic exercises and 1×12 for the isometric. When the RPE rating reached < 12, the load was increased at the next session. At the eleventh session, or when 80% of 1RM was attained, a new 1RM determination was performed. Thereafter, the training load was set to 75% of 1RM (RPE > 16) with repetitions reduced to 2×8 for the dynamic and 1×8 for the isometric exercises. For the remaining sessions the load was increased when the subject’s RPE rating reached < 14.
Both the intensity and the extent of the training period were considered adequate to attain strength gains (26, 30). In addition, this relatively high intensity was effective for women with chronic neck pain (25, 31).
Massage. Massage treatment was deemed suitable, since it is generally considered an acceptable, credible and pleasurable treatment. The treatment consisted of classical massage for the upper body including the back, neck and shoulders. Care was taken by the massage therapists not to massage the affected body regions too forcefully.
Sensorimotor tests
All tests were conducted by author TR who was blinded to the group allocation of the participants. In all tests except postural sway, subjects were seated with belts crossed over the chest to limit their trunk movement.
Postural sway. The migration of the centre of pressure (COP) during quiet standing with eyes closed, feet parallel (18 mm apart) and arms crossed over the chest was measured with a force platform (AMTI model OR6-5, Advanced Mechanical Technology, Inc., Watertown, MA, USA). The sampling frequency was 200 Hz. Instructions were given to: stand as naturally as possible, without tension or intentional body sway. The test duration was 190 s and a short practise trial was performed prior to the test.
Precision of goal-directed arm movements. The precision of goal-directed arm movements was assessed in a pointing task. The set-up was identical to that described by Sandlund et al. (5). A wooden pointer was attached to the palm of the right hand and the pointer tip extended 20 cm from the fingertip of the third digit. This arrangement intended to eliminate influence from fine hand motor control. The soft foam target (1 cm in diameter) was placed in front of the subject at a distance corresponding to the wrist of the subjects’ extended arm, at eye height and 20 cm to the left of the subject’s left acromion. From a starting position with the lower arm on an armrest, subjects made fast and accurate pointing movements towards the target. They were instructed as follows: “Place the pointer as close as possible to the target as fast and accurately as possible. When you have reached the target, keep the pointer still for a few seconds and do not correct the position.” Fifteen trials were performed for each subject (5). The kinematics of the pointer tip were recorded with an electromagnetic tracking system (FASTRAK, Polhemus Inc., Colchester, VT, USA) at a sampling rate of 30 Hz.
Fast axial cervical rotations. The set-up was identical to that described by Röijezon et al. (21). Subjects performed 3 repetitions of cervical axial rotations to each side (right/left) from a neutral head position. The instructions given were: “Turn the head as fast as possible to the right/left.” The kinematics of the head relative to the thorax (Th2) were recorded with an electromagnetic tracking system (FASTRAK, Polhemus Inc.) at a sampling rate of 60 Hz.
Cervical range of motion. The set-up was identical to that described by Rudolfsson et al. (22). Subjects performed 3 repetitions of cervical sagittal flexion and extensions from a neutral head position, followed by 3 repetitions of axial rotation. The instructions were: “Bend your head forward/backward as far as possible.” and “Turn your head to the left/right as far as possible, respectively.” The kinematics of the head relative to the thorax (Th2) was recorded with an electromagnetic tracking system (FASTRAK, Polhemus Inc.) at a sampling rate of 60 Hz.
Primary outcome variables
The 4 primary outcomes were derived from the tests of postural sway and goal-directed arm movements. For the postural sway test, we first decomposed the centre of pressure (CoP) signal to the slow rambling (Ra) and a fast trembling (Tr) components using the method described by Zatsiorsky (32). The magnitude of these signals was calculated as the 95% confidence area for each signal respectively (33). These variables were denoted the centre of pressure area (CoP-A), the rambling area (Ra-A) and the trembling area (Tr-A).
The end-point precision (VE) in the goal-directed arm movement test was calculated as the volume of the ellipsoid spanned by 3 axes representing the variable error (variability of the 15 trials) in the 3 dimensions (34).
Secondary outcomes variables
Four out of 5 secondary outcomes were derived from the tests of cervical kinematics. The fifth was neck pain assessed with a 0–10 Numerical Rating Scale (NRS) (35). We initially aimed to analyse the jerkiness of fast cervical rotations. However, this measure was recently shown to have poor sensitivity and reliability (21) and may also only reflect differences in velocity (36). Based on these results, the peak velocity of fast cervical rotations (Peak Speed) was used instead.
We recently proposed an extended model of estimating range of motion (ROM) in sagittal cervical flexion and extension that separates movements in the upper and lower cervical levels (22). As these ROM measures at baseline were substantially reduced compared with healthy controls in the current sample (22) we modified the secondary outcomes from the trial registration to include upper and lower cervical ROM in flexion and extension (UC-ROM and LC-ROM) as well as maximum axial ROM (axial ROM).
Sample size determination
The required sample size was determined by the postural sway test with the outcome variable CoP-A. This was based on: (i) a 1-week interval reliability test (unpublished data) including 23 participants with neck pain, where the standard deviation of the test-retest difference of CoP-A was 1.07 cm2, (ii) that the least clinical relevant change of CoP-A was determined to 1 cm2 based on our pilot study (14) together with cross-sectional group differences between healthy controls and people with neck pain (unpublished data). For a repeated measures ANOVA the group size was calculated to n = 30 with alpha = 0.05 and beta = 0.05.
Randomization
Baseline measures that could have a main effect on outcome or be a moderator of a specific treatment outcome were considered for the randomization of groups. These measures were age (37, 38), duration of neck pain (37, 39), decreased physical functioning (37, 39) and treatment expectations (38, 39). With 2 independent observers, a computerized random number generator was used to allocate 36 neck pain subjects to each of the 3 intervention groups and 20 to the treatment as usual group (as described above). This step was repeated until no trend of group differences (p > 0.2, t-test) was observed in pair-wise comparisons for the 4 baseline measures.
Statistical analysis
Outcome variables were visually inspected and transformed if normality could not be assumed. A per-protocol analysis approach was used, meaning that only subjects participating in more than 11 treatment sessions and at least one follow-up evaluation were included. The pre-defined hypotheses to evaluate the NCE index treatment with respect to sensorimotor function were tested with 3 repeated measures multivariate analysis of variance (MANOVA), with factor time and group. This method is appropriate when multiple outcomes are related conceptually (40), and since conducting multiple univariate analyses would inflate type 1 error rates. The 3 MANOVAs included 4 primary outcomes for short-term and 6-month effects, respectively, and 4 secondary outcomes for 6-month effect. The factor group had 3 levels (NCE, ST, massage) for the primary outcome analysis and 2 (NCE, massage) for analysis of the secondary outcomes. We defined a treatment effect as a significant interaction between time and group with a p-value < 0.05. If a treatment effect was detected in the MANOVA, additional univariate repeated measures ANOVAs were carried out. The additional secondary outcome of neck pain was analysed with a univariate repeated measures ANOVA for the 6-month effect.
Results
Recruitment and participants
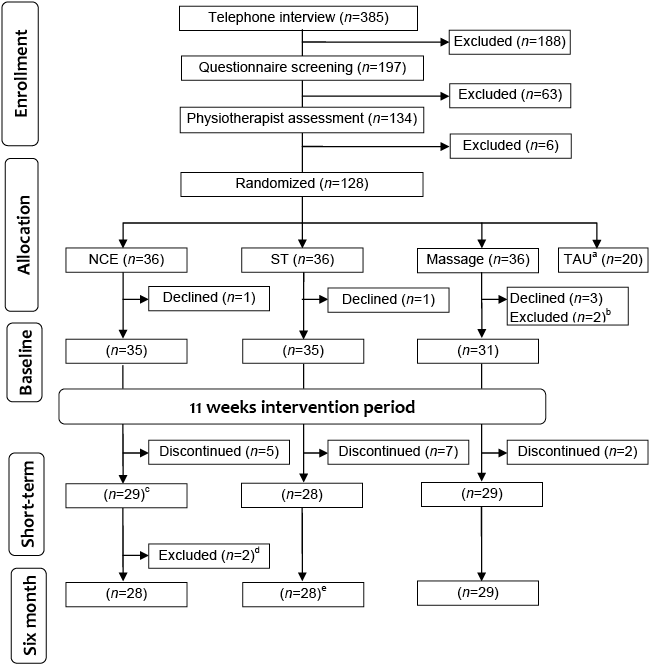
A total of 385 participants were assessed for eligibility for the study. After the randomization there were 36 participants in each of the 3 intervention groups. The flow of participants in the study, including the numbers analysed for short-term and 6-month follow-up, are shown in Fig. 2. Demographic and clinical characteristics of the participants at baseline are shown in Table I.
|
Table I. Baseline demographic and clinical characteristics of the participants in the 3 intervention groups. Neck Disability Index (NDI) and Disability Arm Shoulder Hand (DASH) scores are normalized to the range of 0–100 |
|||
|
Demographics |
NCE (n = 35) |
ST (n = 35) |
Massage (n = 31) |
|
Age, years, mean (SD) |
50.7 (8.6) |
51.6 (9.0) |
51.2 (9.0)) |
|
Weight, kg, mean (SD) |
73.1 (13.1) |
74.1 (14.0) |
73.5 (14.8) |
|
Height, cm, mean (SD) |
167.0 (5.1) |
164.7(5.0) |
165.1 (8.5) |
|
Pain duration, months, median (IQR) |
120 (72–204) |
123 (60–234) |
84 (27–180) |
|
Pain, NRS, median (IQR) |
5 (4–6) |
6 (4–6) |
6 (4–7) |
|
DASH 1–19, median (IQR) |
21.1 (14.5–34.2) |
25 (15.8–31.6) |
26.3 (15.8–42.1) |
|
NDI, mean (SD) |
26.0 (10.3) |
28.6 (10.1) |
30.8 (11.1) |
|
SF-36 PCS, median (IQR) |
43.1 (39.0–46.2) |
39.0 (36.3–45.9) |
39.0 (35.7–47.3) |
|
SF-36 MCS, median (IQR) |
49.4 (38.8–55.3) |
52.3 (42.6–56.1) |
46.5 (33.0–54.5) |
|
NCE: neck coordination exercise; ST: strength training; SD: standard deviation; IQR: interquartile range; NRS: Numerical Rating Scale (35); DASH: Disability Arm Shoulder Hand questionnaire (24); NDI: Neck Disability Index (42); SF-36 PCS: Short Form 36 health survey (SF-36) Physical Component Summary (41); SF-36 MCS: Short Form 36 health survey Mental Component Summary (41). |
|||
In the NCE group, 29 subjects completed the intervention. Out of 22 offered sessions, the median number sessions completed was 22 and the minimum was 13. All subjects completed the basic training programme. Three subjects completed the 12 levels of the progression programme, and the median progression was level 6. The 28 ST subjects who completed the intervention undertook a median of 22 sessions and the minimum was 12. The median number of sessions completed in the massage group (n = 29) was 21 and the minimum was 18. Adverse effects of the index treatment NCE included 1 participant with increased headache and neck pain throughout the intervention period, and 10 participants with transient increased symptoms in the neck or headache on 1–4 occasions.
Primary outcomes
Postural sway measures representing an area were transformed by the square root. The precision of goal-directed arm movements were transformed by the fourth root.
There was a significant treatment effect on the primary outcomes in the short-term evaluation (time × group: Wilks’ lambda = 0.81, F(8, 160) = 2.18, p = 0.03). In the additional univariate repeated measures ANOVAs, variability in end-point precision (VE) was the only variable with significant time × group interaction (F(2,83) = 3.4, p = 0.038). As seen in Table II there was no significant effect on VE in our predefined contrasts, which were NCE compared with ST or massage. We therefore calculated the effect of ST compared with massage on VE as –0.11[–0.20, –0.02], i.e. significantly improved VE for ST, which explains the significant time × group interaction.
Analysis of the 6-month effect of treatment showed no significant difference between interventions (time × group: Wilks’ lambda=0.90, F(8, 156) = 1.03, p = 0.42).
|
Table II. Descriptive statistics of primary outcome measures for all participants at baseline, short-term and at 6 months and effects of exercise as change from baseline compared between groups |
|||||
|
Outcomesa |
NCE Mean (SD) |
ST Mean (SD) |
Massage Mean (SD) |
NCE vs ST Effectsb [95% CI] |
NCE vs Massage Effectsb [95% CI] |
|
CoP-A, cm |
|||||
|
Baseline |
2.50 (0.60) |
2.48 (0.71) |
2.56 (0.69) |
||
|
Short-term |
2.42 (0.51) |
2.36 (0,59) |
2.47 (0.75) |
–0.02 [–0.25 to 0.21] |
–0.06 [–0.36 to 0.24] |
|
Six months |
2.43 (0.52) |
2.40 (0.69) |
2.50 (0.75) |
–0.04 [–0.23 to 0.15] |
–0.09 [–0.33 to 0.16] |
|
Ra-A, cm |
|||||
|
Baseline |
2.07 (0.58) |
2.05 (0.65) |
2.15 (0.65) |
||
|
Short-term |
2.03 (0.48) |
1.95 (0.51) |
2.07 (0.66) |
0.00 [–0.24 to 0.25] |
–0.02 [–0.31 to 0.27] |
|
Six months |
2.04 (0.50) |
2.01 (0.63) |
2.12 (0.69) |
–0.04 [–0.24 to 0.16] |
–0.07 [–0.31 to 0.16] |
|
Tr-A, cm |
|||||
|
Baseline |
0.96 (0.32) |
0.99 (0.32) |
0.97 (0.33) |
||
|
Short-term |
0.91 (0.25) |
0.93 (0.32) |
0.93 (0.35) |
0.00 [–0.09 to 0.09] |
–0.01 [–0.14 to 0.12] |
|
6 months |
0.90 (0.27) |
0.92 (0.34) |
0.93 (0.33) |
0.01 [–0.09 to 0.11] |
–0.01 [–0.13 to 0.10] |
|
VE, cm3/4 |
|||||
|
Baseline |
0.60 (0.15) |
0.64 (0.18) |
0.58 (0.18) |
||
|
Short-term |
0.61 (0.15) |
0.58 (0.17) |
0.60 (0.16) |
0.08 [–0.01 to 0.17] |
–0.03 [–0.10 to 0.04] |
|
Six months |
0.63 (0.17) |
0.60 (0.20) |
0.61 (0.14) |
0.07 [–0.02 to 0.17] |
–0.03 [–0.11 to 0.05] |
|
aTransformed data are presented as outcomes. CoP-A, Ra-A and Tr-A by the square root and VE by the fourth root. bNegative values of effects favour the neck coordination exercise. The effect is calculated on only the participants who completed the follow ups, respectively (see Fig. 2). Cop-A: centre of pressure area; Ra-A: rambling area; Tr-A: trembling area; VE: variability in end point precision; SD: standard deviation; CI: confidence interval; NCE: neck coordination exercise; ST: strength training. |
|||||
Secondary outcomes
There was no significant effect of NCE on the sensorimotor secondary outcomes compared with massage in the 6-month follow-up (time × group: Wilks’ lambda = 0.92, F(4, 53) = 1.12, p = 0.36). Also, the effect on neck pain was non-significant (time × group: F(1, 55) = 1.7, p = 0.20). Group means, standard deviations and differences in univariate change scores between groups are presented in Table III.
|
Table III. Descriptive statistics of secondary outcome measures for all participants in the neck coordination exercise (NCE) and massage groups and effects of exercise as change from baseline compared between groups |
|||
|
Outcomes |
NCE Mean (SD) |
Massage Mean (SD) |
NCE vs massage Effectsa [95% CI] |
|
UC-ROM (°) |
|||
|
Baseline |
71.8 (13.1) |
72.5 (9.6) |
|
|
Six months |
70.1 (13.4) |
71.9 (7.6) |
–0.5 [–3.7 to 2.6] |
|
LC-ROM (°) |
|||
|
Baseline |
20.4 (6.8) |
16.9 (5.4) |
|
|
Six months |
22.4 (7.1) |
21.5 (6.1) |
–2.0 [–4.0 to 0.1] |
|
Peak speed (°/s) |
|||
|
Baseline |
227.8 (78.8) |
213.6 (87.9) |
|
|
Six months |
234.4 (96.0) |
222.3 (84.8) |
1.2 [–26.3 to 28,7] |
|
Axial ROM (°) |
|||
|
Baseline |
118.0 (16.5) |
112.3 (15.9) |
|
|
Six months |
118.5 (16.5) |
116.5 (17.8) |
–2.6 [–7.6 to 2.5] |
|
Pain (NRS) |
|||
|
Baseline |
4.8 (1.5) |
5.8 (1.7) |
|
|
Six months |
3.8 (1.7) |
4.0 (2.1) |
–0.7 [–1.8 to 0.4] |
|
aPositive values of effects favour the neck coordination exercise. The effect is calculated on only the participants who completed the 6-month follow-up (see Fig. 2). UC-ROM: upper cervical range of motion, LC-ROM: lower cervical ROM; peak speed: peak speed of fast cervical axial rotation; axial ROM: ROM of slow paced maximum cervical axial rotations; NRS: Numerical Rating Scale (35). |
|||
Discussion
The main aim of this study was to evaluate the effects of NCE on sensorimotor function in chronic neck pain compared with ST and massage. The primary outcomes showed no superiority of the NCE. In contrast, the ST group showed significant improvement in precision of goal-directed arm movements compared with the sham group. The secondary outcomes concerning cervical ROM, peak velocity of fast cervical rotations and neck pain, showed no superiority of the NCE compared with massage. Thus, our a priori hypotheses were rejected.
An important aspect of this study is that the tasks for which the interventions were evaluated were not intrinsic components of the interventions. This, together with a 6-month follow-up, made it possible to investigate whether transfer and retention of the motor skill were attained. Previous research has shown effects of neck proprioceptive training, evaluated shortly after the intervention in tasks closely related to the training regime (4, 9); this is also supported in a recent study of a specific motor control neck exercise (43). Such effects could be classified as skill acquisition; that is, learning the training task. In the NCE group, skill acquisition was accomplished. Participants completed the 8 levels of the basic programme and the median participant continued to level 6 in the progression programme. Despite this progress, and the fact that the neck coordination exercise method was designed to promote neuromuscular problem-solving, we were not able to show any effects of transfer to other sensorimotor functions.
Tentative explanations for our negative findings could be sought in the choice of outcome variables and the sample size. Even though the outcome variables and the sensorimotor functions they represent have shown associations with neck pain (5, 6, 8, 13), and baseline comparisons between the participants in the present study and healthy controls were found to be significantly different for postural sway (44), cervical ROM (22) and peak speed (21), they were chosen based on cross-sectional findings (5, 6, 8, 13). Hence, the causality is not confirmed. In addition, preliminary analysis of the precision of goal-directed arm movements between the participants in the present study and healthy controls, analysed in accordance with Sandlund et al. (5), was not significant (F(1,133) = 3.448, p = 0.066), which is in contrast with previous findings (5). The sample size was calculated for the primary outcome variable CoP-A of postural sway only. Thus, we cannot be sure of having an accurate sample size for other variables. The above aspects should be considered as limitations of the study.
It is possible that the increased end-point precision found in the ST group follows from the principle of tasks specificity training. In contrast to massage and NCE, the ST intervention included seated shoulder presses with dumbbells and standing chest presses, sharing some resemblances with the goal-directed arm movement task. In addition, training-induced increase in arm-shoulder strength could have improved the control of the rapid goal-directed arm movements in the test. The latter is corroborated by the fact that decreased relative muscle activation favours accurate torque and force production (45).
The synchronized start with parallel interventions is a strength of this study. This eliminated the risk of seasonal effect on the neck pain conditions between groups that otherwise may introduce variance in the outcome measurements. The best evidence and sham control interventions are also strengths. Both interventions are commonly used and massage is an appealing treatment. Thus, biased motivational aspects between groups were probably minimized. Only women were recruited, due to their higher prevalence of neck pain (1), leaving unknown potential treatment effects for males. The study used a convenience sample, thus lowering the generalizability of the results to the population of people with chronic non-specific neck pain. We selected participants who experienced activity limitations due to neck pain. Nevertheless, it is likely that this population is heterogeneous with respect to causality of symptoms as well as to the magnitude of sensorimotor impairments. To minimize the risk of the latter, future rehabilitation research should investigate the use of cut-offs for sensorimotor dysfunction prior to inclusion to proprioceptive or coordinative training modalities. We have now implemented ideas along this line of reasoning in an ongoing study (46).
In conclusion, this randomized controlled trial showed that the neck coordination exercise, carried out with the novel training device, had no advantages over strength training and massage in improving sensorimotor function in women with non-specific chronic neck pain.
Acknowledgements
We thank Maria Frykman and Nisse Larsson for excellent administration and technical assistance. The study was funded by Alfta Research Foundation, grants from the Swedish Council for Working Life and Social Research (2006-1162) and Länsförsäkringar Forskning och Framtid (51-1010/06).
References
