Sacha van Twillert, MSc1, Ilse Stuive, PhD1, Jan H. B. Geertzen, MD, PhD2, Klaas Postema, MD, PhD2 and Ant T. Lettinga, PhD1
From the 1Center for Rehabilitation, University Medical Center Groningen, University of Groningen, Haren and 2Department of Rehabilitation Medicine, Center for Rehabilitation, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands
OBJECTIVE: To examine functional performance, participation and autonomy after discharge from prosthetic rehabilitation and to identify the barriers and facilitators affecting these outcomes.
DESIGN: Concurrent mixed-methods design. Quantitative and qualitative data were collected at discharge from rehabilitation, and 3 and 6 months later. The data were integrated during analysis.
SUBJECTS: Thirteen patients with a unilateral lower limb amputation participating for the first time in prosthetic rehabilitation in a Dutch rehabilitation centre.
METHODS: Functional performance was measured using the Two-Minute Walk Test and L test, and participation and autonomy using the Impact on Participation and Autonomy questionnaire. Barriers and facilitators were identified in semi-structured interviews.
RESULTS: After discharge, 9 out of 13 patients declined in functional performance. The principal problems in participation were observed in the “autonomy outdoors” and “family role” domains. Many factors affected functioning and participation and many differences were observed in the way that factors acted as barriers or facilitators for individual patients. No time patterns were found for barriers and facilitators.
CONCLUSION: Post-discharge, distinctive fluctuations were observed in functional performance and participation and autonomy in patients with lower limb amputation. It is recommended that patients are educated about these fluctuations and the barriers and facilitators identified in the environmental, personal and medical contexts.
Key words: amputation; follow-up studies; ICF; rehabilitation.
J Rehabil Med 2014; 46: 00–00
Correspondence address: Sacha van Twillert, Center for Rehabilitation, University Medical Center Groningen, 9750 RA Haren, The Netherlands. E-mail: s.van.twillert@umcg.nl
Accepted Apr 3, 2014; Epub ahead of print Jul 30, 2014
Introduction
Prosthetic rehabilitation is complex and multifaceted, involving both physical and psychosocial challenges for the patient (1). It aims to optimize health, function, independence and quality of life (2). After discharge from rehabilitation, a long-term adaptation phase begins, during which the harsh realities of the disability are felt by the amputee patient in their own living environment without the direct support of the multidisciplinary rehabilitation team (3, 4). Clinicians have called for more insight into this phase, as they are concerned that the functional performance achieved in rehabilitation, especially of elderly amputee patients, declines after discharge (5). However, little is known about possible changes in functional performance post-discharge and how patients perceive their participation and autonomy in their own living environment. More information is required about the factors that affect these outcomes, so that the content of current rehabilitation programmes can be improved and amputee patients can be optimally prepared for the post-rehabilitation period.
To our knowledge, there have been only 4 follow-up studies after discharge from rehabilitation that have assessed the stability of certain rehabilitation outcomes (6–9). The studies found stability or improvement in examined outcomes, contrary to the decline expected by clinicians. More specifically, the studies found stability in functional status and prosthetic use after 2 months (6) and, after 3 months, sustained low balance confidence scores and improvements in walking ability (7), relative stability in quality of life (8) and improvements in prosthetic wear and locomotor capabilities with the prosthesis and stability in the performance of life habits (9). A variety of outcome measurements and follow-up periods were used, and thus it was difficult to make comparisons. Furthermore, little attention has been paid to autonomy within participation, which is the extent to which patients can determine which activities they participate in and how they participate.
Other studies have attempted to identify the factors that predict functional outcome (10) or quality of life (QoL) (11, 12) of patients with lower limb amputation (LLA). Age at amputation, one-leg balance on the unaffected limb, comorbidity and cognitive impairment were detected in one study as patient factors that forecast functional outcome (10). Many diverse factors, such as perceived prosthetic mobility, prosthesis use and problems, use of an assistive device, phantom limb pain, residual limb pain, depression, social support, social activity participation, employment status, comorbidity and age, were identified as predictors of QoL in 2 other studies (11, 12). A study using secondary data analysis provided preliminary knowledge of the environmental barriers, activity limitations and participation restrictions experienced by patients with a major limb amputation (13). Climate, physical environment and income were pinpointed as the most common environmental barriers encountered by patients with LLA.
Therefore, some studies have provided insight into the sustainability of functional performance post-discharge. Others have indicated which patient and environmental factors might influence their outcome. A more integrated picture of the complexities inherent in functional performance, participation and autonomy after discharge is, however, lacking.
The aim of this study is to provide a better understanding of the impact of barriers and facilitators on functional performance and participation and autonomy post-discharge. Combining both topics in a single study could provide answers as to which factors impact these outcomes post-discharge, as well as to how they affect them. We therefore conducted a mixed-methods study that enabled us to combine the outcome measurements and experiences of these concepts for patients with LLA.
Methods
For this explorative study a concurrent mixed-methods design was used, integrating both quantitative and qualitative research methodologies in the context of a single study (14). Quantitative and qualitative data were collected concurrently at rehabilitation discharge (T0), at 3 months (T1) and 6 months (T2) after discharge, and then integrated during data analysis. The study protocol was approved by the ethics committee of the local University Medical Center.
Patients with LLA participating in prosthetic rehabilitation (inpatient and outpatient service) at a Dutch rehabilitation centre were recruited between June 2009 and September 2010. Inclusion criteria were: (i) the patient has a LLA above Syme level; (ii) the rehabilitation team expects that the patient will function at home with a prosthesis; and (iii) the patient has a good understanding of Dutch language. Exclusion criteria were: (i) the patient has a bilateral LLA; and (ii) the patient was re-admitted for prosthetic rehabilitation. Fifteen participants were initially included. One person did not finish the rehabilitation programme and one person died post-discharge, leaving 13 participants who completed the study. All participants provided written informed consent.
Quantitative methodology
Data on sociodemographic characteristics and diagnosis were extracted from medical records and obtained using a brief self-constructed questionnaire. To assess functional performance, patients performed the Two-Minute Walk Test (2MWT) (15, 16) and the L test (17, 18). The 2MWT objectifies the distance a person can walk within 2 min. The reliability of the test is good: intra-rater reliability 0.90–0.96 and inter-rater reliability 0.98–0.99 (15). The 2MWT has proved responsive to changes in rehabilitation in patients with LLA (16). The L test is a modified version of the Timed Up & Go test (TUG), developed to overcome ceiling effects and insufficient challenge, and to provide a more realistic simulation of the minimal mobility required for older adults to function at home (17, 18). The L test is a walk test in which the seconds are registered to make 2 transfers (get up and sit down) and walk a 20 m L-shaped trail requiring turns to both the right and left (17). The L test has excellent intra-rater and inter-rater reliability; 0.97 and 1.00, respectively (18). Both a higher score on the 2MWT and a lower score on the L test indicate progress. A minimum detectable change of 34.4 m in the 2MWT is considered a relevant change (19). To assess participation and autonomy, patients completed a generic questionnaire on the Impact on Participation and Autonomy (IPA) (20, 21). The IPA measures participation and autonomy in 5 domains: autonomy indoors, family role, autonomy outdoors, social life and relationships, and work and education. Patients can score: 0 = very good, 1 = good, 2 = fair, 3 = poor, and 4 = very poor. Therefore, a higher score on the IPA domains indicates more perceived limitations in participation and autonomy. The IPA has been validated for persons older than 18 year with several chronic conditions within rehabilitation practice (21), but, to our knowledge, has not been used in patients with LLA. Cronbach’s α for each of the domains varies between 0.81 and 0.91 (21). The responsiveness of the IPA is good (20). Due to a difference in scoring of the IPA questionnaire and no available data on subjects with LLA, we had no indication of the minimal detectable change or standard error of measurement. Therefore, the extent of possible changes in outcome on the IPA is difficult to judge.
Qualitative methodology
Semi-structured interviews were used to explore the patients’ individual perceptions and experiences on factors affecting their functioning. The first interview at T0 focused on their perceptions of functioning at that time, on perceived problems in functioning at home, and on their expectations of functional performance and participation post-discharge. At T1 and T2, patients were asked to elaborate on their experiences, to reflect on their previously mentioned expectations, and to indicate barriers and facilitators in post-discharge functioning and participation. Paraphrasing and reflective listening were used at all the interviews. All the interviews were tape-recorded and transcribed verbatim.
Quantitative analysis
Descriptive statistics were used to analyse the quantitative data, including sociodemographic data and measurements of functional performance and participation and autonomy. Data were analysed using SPSS version 16.0.The sociodemographic data of all individual cases are presented in Table I. Scores for functional performance and IPA domains were calculated separately for T0, T1 and T2 for each case. As described in the IPA manual, the domain scores were calculated if 75% of the items were completed. The mean domain score was calculated by dividing the sum score by the number of completed items (21).
Cases were categorized into 3 groups: those that showed an increase or decrease in outcome from T0 to T2 and those retaining their baseline levels.
|
Table I. Sociodemographic data for all individual cases |
|||||||||||
|
Case |
Age (years) |
Gender |
Marital status |
Living accommodation |
Work status |
Duration of rehabilitation (days) |
Type of treatmenta |
Level of amputation |
Side of amputation |
Cause of amputation |
Walking aids |
|
1 |
73.7 |
Male |
Living together |
At home |
No |
114 |
A |
Transtibial |
Left |
Vascular |
Hand-stick |
|
2 |
51.8 |
Male |
Living together |
At home |
No |
105 |
A |
Transtibial |
Left |
Vascular |
None |
|
3 |
72.3 |
Male |
Living together |
Sheltered housing |
No |
94 |
A |
Transtibial |
Left |
Vascular |
One crutch |
|
4 |
36.4 |
Male |
Living together |
At home |
Yes |
207 |
A |
Knee disarticulation |
Right |
Trauma |
None |
|
5 |
55.1 |
Female |
No partner |
At home |
No |
112 |
A |
Transtibial |
Left |
Vascular |
None |
|
6 |
68.7 |
Male |
No partner |
At home |
No |
102 |
A |
Transfemoral |
Left |
Vascular |
Wheeled walker |
|
7 |
57.7 |
Female |
Living together |
At home |
Yes |
137 |
B |
Transtibial |
Right |
Trauma |
One crutch |
|
8 |
38.3 |
Male |
Living separate |
At home |
No |
87 |
B |
Transtibial |
Left |
Trauma |
None |
|
9 |
61.8 |
Male |
Living together |
At home |
No |
170 |
A |
Knee disarticulation |
Right |
Vascular |
One crutch |
|
10 |
55.0 |
Male |
Living together |
At home |
Yes |
240 |
A |
Transtibial |
Right |
Vascular |
One crutch |
|
11 |
54.5 |
Male |
No partner |
At home |
No |
119 |
A |
Transtibial |
Left |
Vascular |
None |
|
12 |
46.9 |
Female |
Living together |
At home |
No |
214 |
A |
Transtibial |
Left |
Other |
One crutch |
|
13 |
29.7 |
Female |
Living separate |
At home |
Yes |
132 |
A |
Transtibial |
Left |
Trauma |
None |
|
aType of treatment: A: inpatient service followed by outpatient service; B: outpatient service. |
|||||||||||
Qualitative analysis
Interview transcripts from each individual case were analysed by the first author (SvT) using Atlas.ti, a qualitative software package. A code list was prepared based on the ICF classification constructs, to provide codes for external factors, personal factors and for body functions and structures (22, 23). As the ICF does not categorize personal factors, we followed the Dutch translation of the ICF, in which personal factors are defined as: aspects of the individual that are no part of the functional health status of the patient (23). Examples are: gender, race, age, coping-behaviour, social background, education and former life experiences. The interviews were coded using the code list. In addition, the quotations grouped within the “external factors”, “personal factors” and “body functions and structures” codes were analysed to identify overall issues. The last author (AL) took the position of reflective questioner to critically asses the coding and analysis. The original transcripts were re-read for renewed analysis in case of disagreement or lack of clarity.
Integration of data
All findings were recorded in a single table to provide an overview (Table II). A maximum of 3 most prominent affecting factors selected for T0, T1 and T2 were combined with an indication of improvement or deterioration over T0 to T2 for the 2MWT and the IPA domains. Data were analysed horizontally within the table at an individual level, which permitted discussion of the quantitative findings with the qualitative findings on barriers and facilitators. Data on affecting factors at T0, T1 and T2 were analysed vertically within this table, which permitted exploration for time patterns in factors. Factors affecting patients who improved were contrasted with factors affecting those who deteriorated.
Results
Population characteristics of the 13 participants are described in Table I.
Functional performance
The L test revealed a range of 16–61 at T0, 16–45 at T1 and 15–45 at T2. The individual scores on the L test and 2MWT showed virtually identical patterns. Due to high Spearman’s rho correlations between the 2 tests for the difference scores at T1–T0, T2–T1 and T2–T0 of –0.94, –0.88 and –0.93, respectively, graphs are presented only for the 2MWT. In total, 9/13 (69.2%) of the patients showed a decline in functional performance (i.e. those who showed a decrease in outcome and those who were not able to perform the performance test on T1 and/or T2). Figs 1a–c illustrate the developments in functional performance: 4 individuals showed an increase (Fig. 1a), 4 showed a decrease in outcome (Fig. 1b) and 5 were unable to perform the performance test on T1 and/or T2 as they were not able to walk (Fig. 1c). The cases with an increase in outcome showed quite a linear progress, whereas the cases with a decrease showed a more variable pattern. Of the cases able to perform the test at all time-points, a clinically relevant change in the 2MWT of 34.4 m was observed only in case 3 between T0 and T1 (decrease), in case 13 between T0 and T2 (decrease) and in case 10 between T0 and T2 (increase).
|
Table II. Individual representation of barriers and facilitators on T0,T1, T2 and developments on Two-Minute Walking Test (2MWT) and IPA over T0 toT2 |
|||||||||
|
IPA |
|||||||||
|
Cases |
Factors T0 |
Factors T1 |
Factors T2 |
2MWT |
AI |
FR |
AO |
SR |
W |
|
Case 1 |
Housing situation – Support + Vascular problems non-amputated leg – |
Climate – Support + Medical condition general – |
Medical condition general – Mood – Prosthetic problems – |
↓ T0 to T1 |
↔ |
↑ |
↓ |
↓ |
× |
|
Case 2 |
Support + Personal factor attitude + Climate – |
Wound stump – Support + Prosthesis + |
Support + Personal factor confidence + Prosthesis + |
↓ |
↔ |
↑ |
↔ |
↑ |
× |
|
Case 3 |
Climate – Housing situation – Support – |
Housing situation – Prosthetic problems – Support – |
Prosthetic problems – Support + Personal factor attitude + |
↓ |
↔ |
↓ |
↓ |
↓ |
× |
|
Case 4 |
Adapted bicycle/car- Personal factor attitude + |
Adapted car/bicycle + Personal factor attitude + Physical condition + |
Personal factor attitude + Automatism + Climate – |
↑ |
↑ |
↑ |
↑ |
↑ |
↑T1 to T2 |
|
Case 5 |
Housing situation – Vascular problems non-amputated leg – Support – |
Housing situation – Operated on non-amputated leg + Stump problems – |
Operated on stump – Prosthetic problems – Housing situation + |
↑T0 to T1 |
↓ |
↓ |
↓ |
↓ |
× |
|
Case 6 |
Personal factor attitude + Assistive devices + Support + |
Prosthetic problems – Inactive coping – Personal factor attitude + |
Climate – Physical condition – |
Measurements only at T0 |
↔ |
↑ |
↓ |
↓ |
× |
|
Case 7 |
Pain free functioning due to amputation + Stump problem – Housing situation + |
Outdoor mobility – Prosthetic problems – |
Outdoor mobility + Stump problems – |
↑ |
↔ |
↑ |
↓ |
↑ |
↓ |
|
Case 8 |
Personal factor attitude + Pain free functioning due to amputation + |
Pain free functioning due to amputation + Employment services – Personal factor attitude + |
Personal factor attitude + Prosthesis + Employment services – |
↑ |
↑ |
↑ |
↑ |
↑ |
↑ |
|
Case 9 |
Housing situation – Pain free functioning due to amputation + Personal factor attitude + |
Stump problems – Climate – Personal factor attitude + |
Transfemoral amputation – Pain free due to amputation + |
↓ |
↓ |
↓ |
↓ |
↓ |
× |
|
Case 10 |
Personal factor attitude + Physical condition – Housing situation – |
Climate – Medical condition general – Personal factor attitude + |
Mood – Employment service: declared unfit to work – |
↑ |
↑ |
↓ |
↑ |
↑ |
↑T0 to T1 |
|
Case 11 |
Medical condition general – Personal factor attitude + Outdoor mobility – |
Medical condition non-amputated leg – Outdoor mobility + Housing situation – |
Medical condition non-amputated leg (will be amputated) – |
Measurements only at T0 |
↓ |
↓ |
↓ |
↓ |
× |
|
Case 12 |
Housing situation – Outdoor mobility + No automatism – |
Medical condition non-amputated leg – Prosthetic problems – Physical condition – |
Medical condition non-amputated leg – Prosthetic problems – |
Measurements only at T0 |
↓ |
↓ |
↓ |
↓ |
× |
|
Case 13 |
Medical condition general – Housing situation – Acceptance – |
Medical condition general – Acceptance – Personal factor attitude + |
Acceptance + Medical condition: operated on non-amputated leg + Personal factor attitude + |
↓ |
↑ |
↓ |
↑ |
↑ |
↓T1 to T2 |
|
+: positive influence; –: negative influence; ×: not applicable; ↔: stable from T0 to T2; ↑: improvement T0 to T2 (i.e. increase Two-Minute Walk Test (2MWT) and decrease IPAdomain); ↓: deterioration T0 to T2 (i.e. decrease 2MWT and increase IPAdomain); IPA: Impact on Participation and Autonomy; AI: autonomy indoors; FR: family role; AO: autonomy outdoors; SR: social life and relationships; W: work and education. |
|||||||||
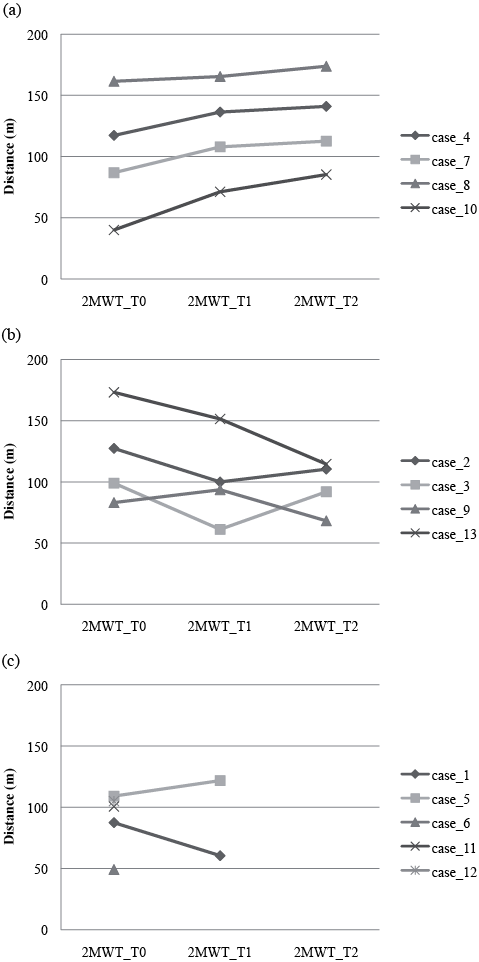
Fig. 1. (a) Increase and (b) decrease in outcome Two-Minute Walk Test (2MWT). (c) Outcome 2MWT for cases unable to perform 2MWT at T1 and/or T2.
Participation and autonomy
The main limitations in participation and autonomy were observed in the “autonomy outdoors” and “family role” domains, with scores of fair to poor. Figs 2–6 illustrate all individual data on the 5 IPA domains. Autonomy indoors: 4 cases showed a decrease (Fig. 2a), 4 showed an increase (Fig. 2b) and 5 had the same scores at T2 as at T0 (Fig. 2c). Family role: 6 cases showed a decrease (Fig. 3a) and 7 showed an increase (Fig. 3b). Autonomy outdoors: 4 cases showed a decrease (Fig. 4a) and 8 showed an increase (Fig. 4b). Fig. 4c presents the one case in which T2 equals T0. Social life and relationships: 6 cases showed a decrease (Fig. 5a) and 7 showed an increase (Fig. 5b). Of the domain “work and education” (Fig. 6) those 5 cases are presented for whom work was relevant during the study. Case 10 showed a small decrease over T0 to T1 and case 4 showed a decrease over T1 to T2. For case 13, work became an issue at T2, at which point the patient scored high for problems in autonomy. Case 8 showed a temporary decrease at T0 to T1, but an increase from T1 to T2, and case 7 showed an increase, indicating more limitations in autonomy at work.
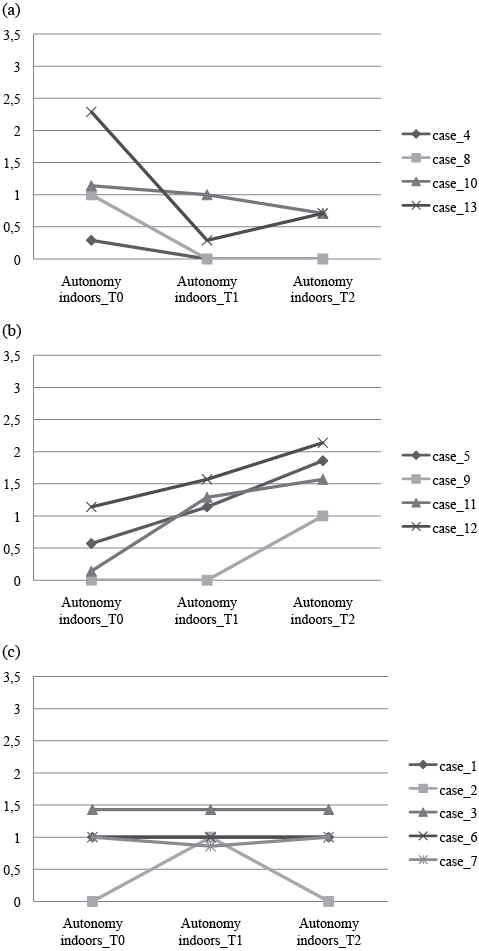
Fig. 2. (a) Decrease and (b) increase in outcome Impact on Participation and Autonomy domain Autonomy indoors. (c) Outcome in IPA domain Autonomy indoors T0 = T2.
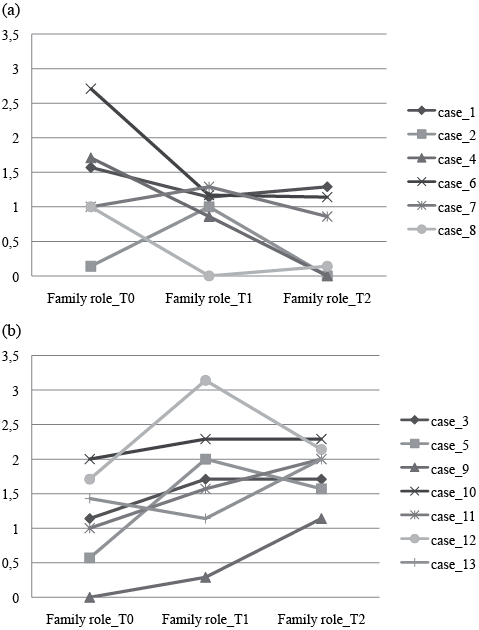
Fig. 3. (a) Decrease and (b) increase in outcome Impact on Participation and Autonomy domain Family role.
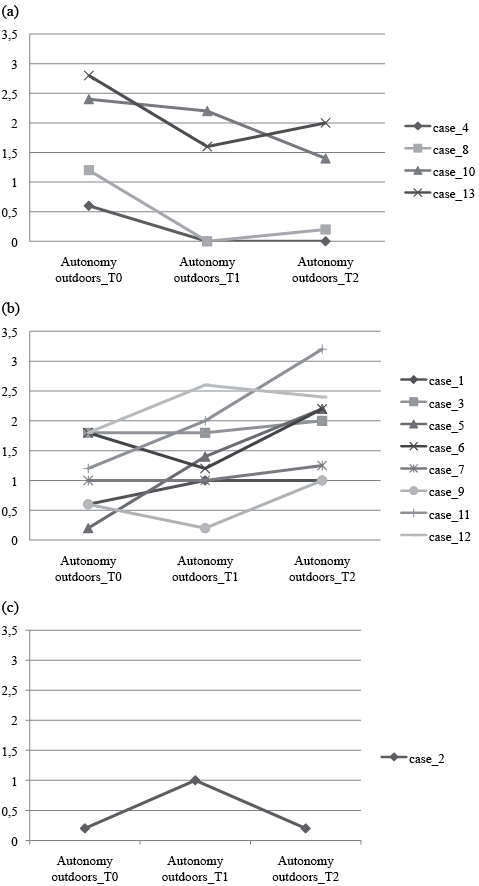
Fig. 4. (a) Decrease and (b) increase in outcome Impact on Participation and Autonomy (IPA) domain Autonomy outdoors.
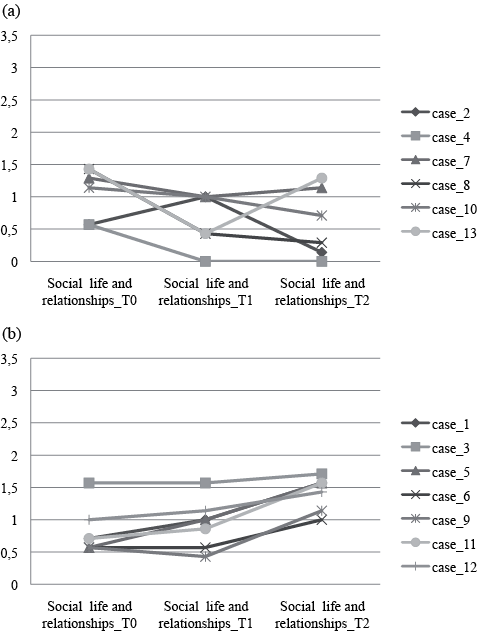
Fig. 5. (a) Decrease and (b) increase in outcome Impact on Participation and Autonomy domain Social life and relationships.
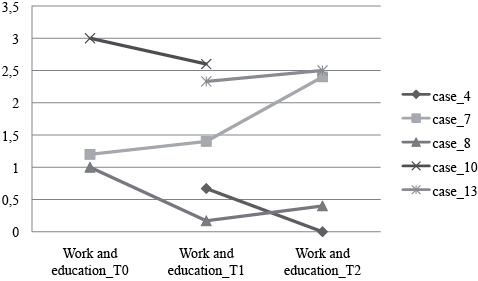
Fig. 6. Outcome Impact on Participation and Autonomy domain Work and education.
External factors
With regard to the external factors, the Products and technology item stood out as the most frequently mentioned factor in both a positive (facilitator) and a negative sense (barrier). This item centred on 2 topics: prosthetic-related issues, such as fitting problems due to decreased stump volume, and outdoor mobility-related issues, such as adapted bicycles, cars or hand-bikes. The fitting problems led to reduced activity in some patients, while others actively sought help and talked about the adjustments required instead of problems. Many patients expressed an experience of freedom when regaining outdoors mobility; to be able to go outdoors, without being dependent on others, was highly valued. The natural environment and, more specifically, the inevitable consequences of the Dutch climate, was a barrier for many patients. A long snowy winter and slippery surfaces hindered many in functioning, although warm weather was also indicated as negative as it led to sweating and irritated skin when wearing the prosthesis. Support from partners, family, friends and personal care providers was most often seen as a facilitating factor. The support of peers was especially prominent as a valued factor during rehabilitation, and was accordingly experienced as a loss post-discharge. Support was also mentioned by some patients as a barrier: the unsought support from family members or partners, overprotective spouses and loss of support from health professionals were perceived as hindering independent functioning. With regard to services, systems and policies, many patients experienced problems in their housing situation; for instance, narrow areas and stairs complicated functioning at home, especially when patients did not wear their prostheses. Few patients mentioned labour and employment services. One patient experienced no cooperation in his desire to return to work, others were declared unfit to work or were advised to look for other jobs.
Personal factors
At discharge, many patients were positively orientated and appreciative of the goals they had reached during rehabilitation, and they expected to continue to improve. The personal factors mentioned at all time-points were diverse. Coping strategies and attitude were often indicated as positive. A positive attitude, confidence, perseverance, goal-orientation, internal motivation, and a solution-focused attitude were personal characteristics that helped many of the patients to deal with the amputation and their changed reality in daily life. Personal factors that were perceived more negatively often referred to personal characteristics and lifestyle, such as perceived feelings of aversion towards asking for help or fear about undertaking certain activities. Some patients indicated a lack of motivation that hindered them from maintaining the physically active lifestyle they had experienced during rehabilitation.
Body functions and structures
The most common barriers to functioning were factors of body functions and structures. Only two individuals (both improvers) reported no physical problems. Most of these factors were related to the amputation, such as wounds on the stump, skin problems or related conditions, such as vascular diseases, which impacted their non-amputated leg. One patient received a transfemoral amputation after the initial transtibial amputation, one was re-operated on the stump, two were operated on their non-amputated leg, and one had the non-amputated leg amputated shortly after T2. Co-morbidity in general also impacted functioning negatively. The emotional impact of the amputation was often referred to negatively: depression, worries, the process of acceptance and the feeling of being observed in the real world. Factors of body functions and structures were, however, also positively articulated: pain relief owing to the amputation, gaining renewed physical possibilities, the experience of more automatism in walking and the perception of having a better physical condition. It is important to note that some of the above-mentioned operations initially acted as barriers, but ended up as facilitator through the removal of underlying physical problems.
Integrating functional outcomes and barriers and facilitators
Table II presents an overview of all individual data. The horizontal analysis of Table II, which integrates quantitative and qualitative data, resulted in 13 different individual stories, in which in some cases qualitative findings provided an explanation for the quantitative findings. Consider case 2: a deterioration in physical performance and a temporary decline in perceived autonomy indoors and outdoors could be directly ascribed to a fall at home, which led to a wound on the stump. The overall high incidence of medical conditions was very apparent in the patients who declined in functional performance. Four of the 5 patients who were unable to carry out the performance tests at T1 and /or at T2 had severe medical conditions, the other patient experienced prosthetic problems.
The horizontal analysis also illustrated how multifaceted individual functioning is. Consider case 10: although this patient improved in functional performance and in several IPA domains, he experienced a decline in emotional well-being. Case 13 illustrates, in contrast, a decline in functional performance over time along with improvements in autonomy indoors and outdoors and in social life and relationships in the IPA. This patient indicated that improved emotional well-being and acceptance was attained after an initial moment of emotional distress post-discharge.
Vertical analysis of Table II provided insight into which barriers and facilitators were most prominent at which time. It revealed that, although many patients indicated similar barriers and facilitators after discharge (for example, outdoor mobility, prosthetic problems and housing situation issues), a collective time pattern could not be discerned.
Personal factors were particularly prominent within the group of patients who showed improvement in functional performance and participation and autonomy. They noted being strong-willed, persevering, goal-oriented, confident and highly motivated.
Discussion
The integration of quantitative and qualitative methodology in a single study provided us with in-depth information on the post-rehabilitation period for patients with LLA. This study showed that 9 of our 13 patients declined in functional performance after discharge. The main participation limitations were perceived in the “autonomy outdoors” and “family role” domains. Changes in outcomes on functional performance were, however, not always in line with those observed in participation and autonomy. Many diverse factors were found to affect functional performance and participation post-discharge, acting sometimes as barriers for some individuals and as facilitators for others. We realize that our sample size was small and consisted of a convenience sample of participants from a single rehabilitation centre. Our results are therefore not generalizable to all patients with LLA and to all rehabilitation settings.
The large percentage of patients that declined in functional performance in our study contrasts with results for stability or improvement in functional outcomes post-discharge seen in previous studies (6, 7, 9). Our study design provided insight into the factors that explained the individual decline, such as medical complications and prosthesis problems. It is also important to note that 3 of the 4 patients who decreased from T0 to T2 started at very high 2MWTlevels at discharge and deteriorated to a level that can still be considered high compared with the outcomes of Brooks et al. (16). When we relate our ranges on the L test to the mean score and standard deviation of the study by Miller & Deathe (7), we can conclude that our subgroup, that performed the test at T0, T1 and T2, performed better as our maximum score equals their mean score. Both groups show a large variability in outcome.
With regard to participation, the IPA was chosen to identify person-perceived participation and autonomy rather than just measuring functional independence (21). Many patients experienced more limitations in autonomy outdoors, and are somehow restricted in their family role. “Getting heavy tasks done”, “Getting minor repairs done”, “Fulfilling my role at home”, “Going on trips and holidays” and “Living the life I want” were thereby items that scored fair to poor. Individual fluctuations over time were also observed for these outcomes. The outcomes on the IPA gave insight into which items were of importance and/or changing over time for each individual. Thus, this questionnaire is of great value for clinicians. In order to measure effect, there is need for comparable data measured in groups with different diagnoses, analysed as prescribed in the IPA manual.
With respect to barriers and facilitators, our study did not detect new factors affecting functional performance and participation, but provided a better understanding of how factors influenced the functioning of patients, and the individual diversity in these interactions. Factors such as a changing stump volume, climate and environmental factors caused problems for some patients, while others coped adequately with these circumstances. The presence of barriers and facilitators also appeared to fluctuate over time. No clear collective time pattern became apparent.
Our analysis of outcomes at an individual level revealed distinguishing fluctuations in functional performance, in IPA domains and in the presence of barriers and facilitators over time. This is in striking contrast with the stability and improvements in outcomes outlined in previous studies, in which individual patterns were averaged out. This pattern of fluctuations is an extremely important insight for rehabilitation professionals. We believe it is up to these professionals to prepare patients for the distinctive fluctuations in functioning post-discharge and the upcoming barriers patients can encounter. Our studied patients were confident they would continue to improve after discharge; however, the reality was different. It is inevitable that patients will encounter barriers; climate conditions are foreseeable and a changing stump volume is a known phenomenon (24). Due to the great diversity in individual reactions to perceived barriers, it would be helpful to teach patients a generic approach to dealing with problematic situations.
In a previous study we proposed integrating self-management principles and task and context-specific training principles to teach patients problem-solving to enhance functional carry-over from the clinical to the home setting (5). Others have also emphasized the need for self-management interventions for this diagnosis group (25). The results of this study confirm our previous line of reasoning and provide concrete issues that patients need to cope with. Integrating problem-solving principles and techniques in the rehabilitation phase to enhance the patients’ confidence in their own capacities in problem-solving could prepare patients for the post-rehabilitation phase and, it is hoped, will contribute to less decline in outcome. In addition to changes in clinical practice during prosthetic rehabilitation, we propose that regular follow-ups are carried out after discharge, as recommended in guidelines (2). The focus should then be on perceived barriers and the patients’ capacity for coping with these barriers.
With respect to future research, we hope that the added value of mixed methods that emerged in this study will inspire researchers to combine quantitative and qualitative methodology, despite the resulting length of publications. In our study we distinguished which quantitative outcomes were most pertinent to our research question, in order to have sufficient article length to present the integration findings, given that this is the key reason for conducting mixed-methods research (26–28). The justification for undertaking mixed-methods studies is to engage with the complexity of health(care) by adopting a more comprehensive approach than a single set of methods would allow (26). Therefore our results contribute to a better understanding of the post-discharge phase of patients with LLA, providing professionals with insights and tools to prepare patients for the challenges they will face in everyday life.
Acknowledgements
This project was supported by grants from Stichting OIM and Stichting Beatrixoord NN, neither of which had any influence on the interpretation of the data or the final conclusions. Special thanks go to all the patients who participated in this study.
References
