Federica Menotti, PhD1, Luca Laudani, PhD1, Antonello Damiani, MD2, Paola Orlando, MD2 and Andrea Macaluso, MD, PhD1
From the 1Department of Human Movement, Social and Health Sciences, University of Rome Foro Italico and 2Unione Italiana Lotta alla Distrofia Muscolare (UILDM), Sezione Laziale, Rome, Italy
OBJECTIVE: To compare walking energy cost between an anterior and a posterior ankle-foot orthosis in people with foot drop.
DESIGN: Within-group comparisons.
PARTICIPANTS: Twenty-three adults (14 women, 9 men; mean age 56.8 years (standard deviation 15.4)) with foot drop.
METHODS: Participants were asked to walk for 5 min at their self-selected walking speed under 3 conditions: (i) with shoes only; (ii) with a posterior ankle-foot orthosis; (iii) with an anterior ankle-foot orthosis. Spatio-temporal gait parameters (speed, step length and step frequency) and walking energy cost per unit of distance were assessed for each walking condition. A visual analogue scale was used to quantify participants’ level of perceived comfort for the 2 orthosis.
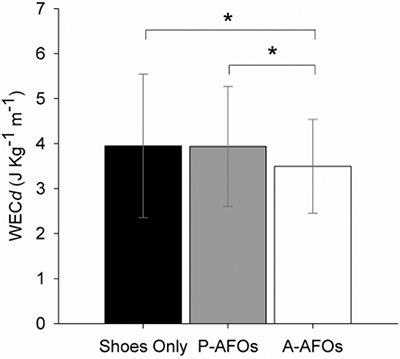
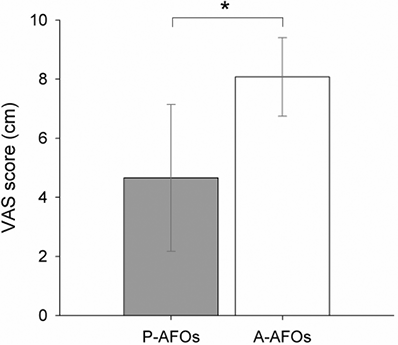
RESULTS: Gait spatio-temporal parameters were higher with anterior ankle-foot orthoses than with posterior ankle-foot orthoses or shoes only. Walking energy cost per unit of distance was lower with anterior than posterior ankle-foot orthosis or shoes only ((mean ± standard error) 3.53 ± 1.00 vs 3.94 ± 1.27 and 3.98 ± 1.53 J·kg–1·m–1 respectively; p < 0.05) and level of perceived comfort was higher with anterior ((mean ± standard error) 8.00 ± 1.32) than with posterior ankle-foot orthosis ((mean ± standard error) 4.52 ± 2.57; p < 0.05).
CONCLUSION: In people with foot drop the use of anterior ankle-foot orthoses resulted in lower energy costs of walking and higher levels of perceived comfort compared with posterior ankle-foot orthoses. Anterior ankle-foot orthoses may enable people with foot drop to walk further with less physical effort than posterior ankle-foot orthoses.
Key words: walking economy; neuromuscular disorders; gait impairment.
J Rehabil Med 2014; 46: 00–00
Guarantor’s address: Andrea Macaluso, Department of Human Movement, Social and Health Sciences, University of Rome Foro Italico, Piazza Lauro De Bosis 6, IT-00135, Rome, Italy. E-mail: andrea.macaluso@uniroma4.it
Accepted Mar 17, 2014; Epub ahead of print Jun 19, 2014
INTRODUCTION
Ankle-foot orthoses (AFOs) are commonly prescribed in people with paretic ankle dorsiflexor muscles in order to improve quality of walking and reduce the risk of stumbling and falling during the swing phase of gait (1). Various designs, features and materials of AFOs exist, although posterior leaf spring AFOs (P-AFOs) are the most commonly used (2). Positive effects of P-AFOs on walking performance have been demonstrated in people with different neuromuscular disorders, such as hemiplegia (2–9), facioscapulohumeral dystrophy (10), Charcot-Marie-Tooth disease (11–15) and cerebral palsy (16–18). Walking with P-AFOs results in an increase in walking speed (2, 4, 6, 9, 11–14), step length and step frequency (2, 9, 11, 15) compared with walking with shoes only. Moreover, improvements in gait kinematics have been demonstrated, such as a reduction in the compensatory hip and knee flexion in the middle phase of swing (13, 19), an increase in ankle dorsiflexion during the swing phase and the initial heel contact (5, 13) and an increase in the knee extensor moment at the early stance phase (5). The use of P-AFOs has been demonstrated to improve gait efficiency (16–18, 20–21). However, there are concerns about the comfort and appearance of P-AFOs (2, 22) and thus usually only people with a high level of walking impairment would use them on a regular basis (23).
Anterior elastic AFOs (A-AFOs) are designed to improve comfort and adaptability to ready-made shoes. A few recent studies have evaluated the effect of different types of A-AFOs, and found that they improved walking performance of people with foot drop. The use of A-AFOs significantly increased ankle dorsiflexion (19), decreased compensatory hip flexion during the swing phase (19), enhanced step length (15), improved postural stability (24), and decreased the energy cost of walking (25) compared with shoes only. All these imply that A-AFOs help reduce physical effort on walking.
Previous studies comparing walking performance between A-AFOs and P-AFOs in people with foot drop reported that A-AFOs were of less (26) or similar (19) effectiveness in maintaining ankle dorsiflexion on the sagittal plane during the swing phase of gait than P-AFOs. While there were no differences in walking speed and step length (15), a higher level of perceived comfort was found with A-AFOs than with P-AFOs (26). To the best of our knowledge, no studies have compared the metabolic cost of walking between A-AFOs and P-AFOs in people with foot drop. The measurement of walking energy cost per unit of distance (WECd), also referred to as walking economy, is a valid indicator of walking performance (27, 28). Moreover, WECd is a quantitative and reliable method to detect walking impairment even when it is minor (29). The purpose of this study was therefore to compare walking energy cost, level of perceived comfort, walking speed, step length and step frequency in people with foot drop between A-AFOs and P-AFOs. We hypothesized that walking with either A-AFOs and P-AFOs in people with foot drop would reduce metabolic energy cost compared with walking with shoes only, and A-AFOs would be more comfortable than P-AFOs. As a secondary outcome, we hypothesized that individuals with A-AFOs would walk at a similar speed to that of individuals with P-AFOs, with no changes in step length and step frequency, as reported previously (15).
METHODS
Participants
Twenty-three participants with foot drop (14 females, 9 males; mean age 56.8 years (standard deviation; SD 15.4); mean body mass 70.7 kg (SD 11.6) were recruited from the “Unione Italiana Lotta alla Distrofia Muscolare” (UILDM) Rehabilitation Centre in Rome. The inclusion criteria were: (i) Medical Research Council (MRC) score of the ankle dorsiflexors ≤ 3 (30); (ii) Barthel Index > 70 (31); and (iii) no clinical signs of heart or pulmonary disease. Five of the participants had muscular dystrophy, 7 had peripheral nerve disorders and 11 had central nervous system (CNS) disorders. The median Barthel Index was 98/100 (interquartile range; IQR 95–100); the median Tinetti score (32) was 19/28 (IQR 17–21): 11/16 for balance (IQR 10–13) and 8/12 for walking (IQR 7–8), as described in Table I. In addition, no participants had spasticity, joint limitations or proximal muscle weakness (MRC of hip extensors and hip flexors 5/5, 4–5; knee extensors 5/5, 5–5; knee flexors 5/5, 4–5; median, IQR). The clinical scores were assigned by a single clinician who was employed in the clinical centre in which participants were recruited. The study was approved by the ethics committee of the University of Rome La Sapienza, and carried out in accordance with the principles of the Declaration of Helsinki. Informed consent was obtained from all participants.
|
Table I. Clinical characteristics of participants |
||||||||||
|
Subject/gender |
Diagnosis |
Orthosis |
Medical Research Council (MRC) score |
Barthel Index |
Tinetti Scale score |
|||||
|
Dorsiflexors |
Plantarflexors |
|||||||||
|
Right |
Left |
Right |
Left |
Balance |
Walking |
|||||
|
P1/M |
Traumatic brain injury |
Right |
0 |
5 |
5 |
5 |
97 |
10 |
7 |
|
|
P2/F |
Myelomeningocele |
Right |
0 |
4 |
0 |
5 |
100 |
10 |
7 |
|
|
P3/F |
Multiple sclerosis |
Left |
5 |
1 |
5 |
5 |
100 |
11 |
7 |
|
|
P4/F |
Post-vaccination encephalomyelitis |
Both |
0 |
0 |
5 |
5 |
98 |
6 |
8 |
|
|
P5/F |
Charcot-Marie-Tooth disease |
Both |
0 |
0 |
0 |
0 |
90 |
10 |
5 |
|
|
P6/F |
Lateral popliteal nerve injury |
Left |
5 |
3 |
5 |
5 |
89 |
12 |
7 |
|
|
P7/F |
Cerebral palsy |
Right |
3 |
5 |
5 |
5 |
100 |
14 |
10 |
|
|
P8/F |
Cerebral palsy |
Right |
0 |
5 |
4 |
5 |
97 |
10 |
7 |
|
|
P9/F |
Lateral popliteal nerve injury |
Left |
5 |
0 |
5 |
5 |
100 |
11 |
8 |
|
|
P10/F |
Lateral popliteal nerve injury |
Left |
5 |
0 |
5 |
5 |
100 |
14 |
8 |
|
|
P11/F |
Post-polio |
Right |
2 |
5 |
4 |
5 |
100 |
13 |
9 |
|
|
P12/M |
Facioscapulohumeral dystrophy |
Right |
2 |
4 |
4 |
5 |
91 |
10 |
7 |
|
|
P13/F |
Lateral popliteal nerve injury |
Right |
0 |
5 |
5 |
5 |
100 |
14 |
8 |
|
|
P14/M |
Lateral popliteal nerve injury |
Left |
5 |
0 |
5 |
5 |
100 |
11 |
8 |
|
|
P15/F |
Lateral popliteal nerve injury |
Right |
3 |
5 |
5 |
5 |
89 |
12 |
7 |
|
|
P16/F |
Cerebral palsy |
Left |
5 |
1 |
5 |
4 |
98 |
10 |
8 |
|
|
P17/M |
Cerebral palsy |
Right |
2 |
5 |
3 |
5 |
81 |
10 |
7 |
|
|
P18/M |
Cerebral palsy |
Left |
5 |
3 |
5 |
5 |
100 |
14 |
10 |
|
|
P19/M |
Myotonic dystrophy |
Both |
2 |
2 |
5 |
5 |
96 |
11 |
7 |
|
|
P20/F |
Facioscapulohumeral dystrophy |
Both |
2 |
2 |
5 |
5 |
95 |
12 |
8 |
|
|
P21/F |
Amyotrophic lateral sclerosis |
Both |
2 |
2 |
4 |
4 |
95 |
13 |
10 |
|
|
P22/F |
Facioscapulohumeral dystrophy |
Both |
2 |
2 |
5 |
5 |
74 |
5 |
7 |
|
|
P23/F |
Facioscapulohumeral dystrophy |
Both |
3 |
3 |
5 |
5 |
98 |
13 |
10 |
|
|
M: male; F: female. |
||||||||||
Instrumentation and measurements
The oxygen uptake (V.O2) and carbon dioxide production (V.CO2) were measured by means of a telemetric, portable gas analysis system (K4b2, COSMED, Rome, Italy). The system has been proved to be valid, accurate and reproducible, during rest and exercise at various intensities (33). V.O2 was first measured with participants sitting for 5 min to reach a steady state. Participants were then requested to walk on an oval-shaped 26.5-m walkway circuit under 3 conditions that occurred in random order: (i) A-AFOs (Taloelast®, Ortopedia Mancini, Rome, Italy), (ii) P-AFOs (Ortopedia Mancini, Rome, Italy) and (iii) shoes only (Fig. 1). Taloelast® consists of a polypropylene leaf positioned above the anterior part of the leg, ankle and foot. The proximal part is fixed by means of a Velcro® strap at the leg level and the distal part is placed underneath the shoelaces. An elastic-adjustable Velcro® strap goes from the distal part to the proximal part of the polypropylene leaf. The elastic strap provides resistance to plantarflexion, which is sufficient to maintain adequate ankle dorsiflexion and allows ground clearance during the swing phase. P-AFOs consist of a lightweight polypropylene-based plastic in the shape of an “L”, with the upright portion behind the calf and the lower portion placed under the foot. They are attached to the calf with a strap, and are made to fit inside accommodative shoes. In each condition participants were asked to walk at their comfortable self-selected walking speed. Each condition lasted 5 min in order to reach a steady-state, followed by 5 min of rest to provide adequate recovery time, which was verified by visually inspecting V.O2 prior to beginning the next trial. The V.O2 obtained during the final minute was used for further analysis. At the end of each AFO walking condition, the level of perceived comfort was assessed using a 10-cm visual analogue scale (VAS) (34).
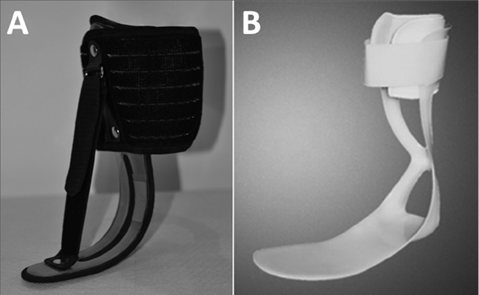
Fig. 1. (A) Taloelast® (Ortopedia Mancini, Rome, Italy) ankle-foot orthosis; (B) posterior plastic ankle-foot orthosis.
Data analysis
As primary outcome, we calculated the net walking energy cost per unit distance (WECd), normalized by body mass, expressed in J∙kg–1∙m–1. The following formula was used: WECd = (WECt – SECt)/S, where WECt is the energy cost during walking per unit of body mass and per unit of time (J∙kg–1∙min–1), SECt is the energy cost during sitting (J∙kg–1∙min–1) and S is walking speed in m∙min–1. Both WECt and SECt were calculated as the product between the amount of oxygen uptake (ml∙kg–1∙min–1) and the energy equivalent of oxygen (J) (28, 35). The respiratory gas-exchange ratio (RER) of the last minute was taken into account to adjust the energy equivalent of oxygen (33). Scores about comfort perception were assessed with a ruler by measuring the distance between zero and the point drawn by each volunteer on the 10-cm VAS.
As secondary outcomes, speed, step length and step frequency were calculated. Mean walking speed was obtained by dividing the total walking distance (m) by the time taken to cover it (s). Step length (m), was computed as the total distance walked by the individual divided by the total number of steps counted by the experimenter. Step frequency, expressed in steps/s, was computed as mean walking speed divided by step length.
Statistics
All data were normally distributed in terms of skewness and kurtosis (all values less than |2|). Statistical comparisons of the parameters (WECd, speed, step length, step frequency), between the 3 conditions (A-AFOs, P-AFOs and shoes only) and were carried out using a 1-way analysis of variance (ANOVA), followed by Student’s t-tests with Bonferroni correction. Statistical comparison of the VAS scores between the 2 AFOs conditions (A-AFOs and P-AFOs) was carried out by Student’s t-test.
Statistical significance level was set at p < 0.05.
RESULTS
Primary outcomes
There were significant differences in walking energy cost among the walking conditions (Fig. 2). The WECd was lower in A-AFOs compared with both P-AFOs and shoes only (p < 0.05).
The level of perceived comfort was higher for A-AFOs than P-AFOs (p < 0.05), as shown in Fig. 3.
Secondary outcomes
There were significant differences in walking speed and step length among the walking conditions (p < 0.05; Fig. 4). Walking speed was significantly higher in the A-AFOs condition compared with the P-AFOs condition (Fig. 4A), whilst step length was significantly higher in the A-AFOs condition than in the shoes only condition (Fig. 4B).
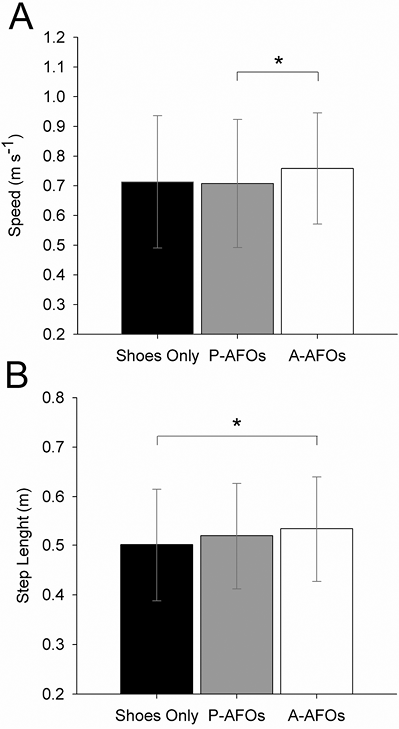
There were no differences in step frequency among the 3 walking condition (shoes only: 1.42 ± 0.32 step/s; P-AFOs: 1.36 ± 0.30 step/s and A-AFOs: 1.43 ± 0.30 step/s; p > 0.05).
DISCUSSION
This was the first study to compare walking energy cost and level of perceived comfort between A-AFOs and P-AFOs in a group of people with foot drop. The results show that walking with A-AFOs requires less energy than walking with P-AFOs, and level of perceived comfort was higher with A-AFOs than P-AFOs.
This finding is in line with previous studies that also showed that AFOs reduced the energy cost of walking compared with shoes in a sample of subjects with Charcot-Marie-Tooth 1A with foot drop (25). It is likely that AFOs reduce the energy cost by normalizing walking pattern towards a reduction in steppage gait (25, 36). The design, weight and structural characteristics of the 2 orthoses could also explain the differences in metabolic energy cost of walking. The P-AFOs cover the plantar aspect of the foot and may reduce the mechanoreception of the foot on walking. A study has suggested that the reduction in plantar sole mechanoreceptor sensitivity increases lower limb muscles activity (37) and agonist and antagonist muscles co-contraction around the knee and ankle joints (38). This may be another reason for the difference in the energy cost of walking between A-AFOs and P-AFOs. Our findings appear to contradict the gait analysis findings of Ramdharry et al. (19), who observed no differences between A-AFOs and P-AFOs in hip flexion and ankle dorsiflexion during the swing phase, which should theoretically lead to a similar energy cost. However, comparisons are difficult due to the different measuring techniques.
In our study, self-selected speed was higher in the A-AFOs condition than the P-AFOs condition. The step length in the A-AFOs condition was higher than in the shoes only condition, but not higher than in the P-AFOs condition. No difference was found between step frequencies in the 3 walking conditions. The higher walking speed with A-AFOs than P-AFOs is in contrast with the hypothesis of our study and the finding of Guillebastre et al. (15), who showed no differences in walking speed between the 2 orthoses. The higher step length in both A-AFOs and P-AFOs compared with shoes is consistent with the results of Guillebastre et al. (15), but in constrast to Ramdharry et al.’s study (19). The discrepancy between studies may be due the different clinical populations and levels of walking impairment.
The level of perceived comfort was significantly higher when walking with A-AFOs compared with P-AFOs, which is consistent with the results of Park et al. (26). As observed by a previous study, people’s willingness to use AFOs depends more on the comfort level than the effect of AFOs on gait and balance (22). Since A-AFOs are more comfortable, they are likely to have higher levels of compliance than P-AFOs.
The limitation of this study is that the data were derived from a single walk trial. A follow-up study to asses function, compliance and satisfaction will be useful to determine long-term effects and efficacy. Moreover, the clinical importance of these findings could not be determined.
In conclusion, A-AFOs provide better walking economy and are more comfortable than P-AFOs. Therefore, A-AFOs are more likely to improve compliance and walking ability than P-AFOs.
ACKNOWLEDGEMENT
The authors would like to thank Dr Jacqueline Mair for reviewing the paper.
REFERENCES
