Seung Bae Yoon, MD
From the Department of Internal Medicine, National Rehabilitation Center, Seoul, Korea
OBJECTIVE: To determine the prevalence of, and risk factors for, highly resistant microorganisms (HRMO) in urinary isolates from newly admitted patients in a rehabilitation hospital.
SUBJECTS: A total of 906 patients transferred to a rehabilitation hospital from other hospitals.
METHODS: A screening study was performed from June 2012 through May 2013. Urine samples were collected from transferred patients on admission day.
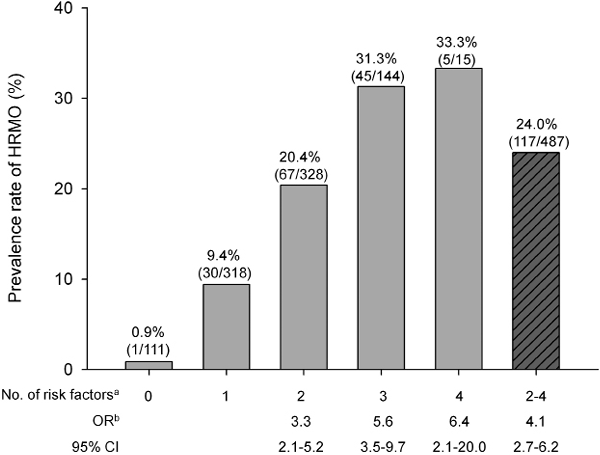
RESULTS: Of the total of 916 patients, 148 (16.2%) displayed growth of HRMO in urine cultures. Gram-negative species had a higher number and ratio of HRMO compared with Gram-positive species (141/325 (43.4%) vs 9/97 (9.3%)). Multivariate analysis revealed that age over 60 years, female sex, recent surgery, and use of urinary catheters were risk factors for HRMO among all admitted patients. Even among patients with bacteriuria, recent surgery and an indwelling urinary catheter were significant risk factors for HRMO colonization. The odds ratio for prevalence of HRMO in patients with 2 or more risk factors was 4.1 (95% confidence interval 2.7–6.1), compared with those with single or no risk factors.
CONCLUSION: The prevalence of HRMO in rehabilitation patients was higher than expected. Routine screening of urine culture for HRMO is therefore recommended in rehabilitation patients with multiple risk factors.
Key words: antibiotic resistance; rehabilitation centres; prevalence; risk factors.
J Rehabil Med 2014; 46: 00–00
Accepted Mar 18, 2014; Epub ahead of print May 21, 2014
Correspondence address: Seung Bae Yoon, Department of Internal Medicine, National Rehabilitation Center, 58 Samgaksan-ro, Gangbuk-gu, Seoul, Korea. E-mail: sbyoon@catholic.ac.kr
INTRODUCTION
Over the past several decades hospitals have experienced rapid and ongoing spread of antimicrobial-resistant bacteria and resultant serious infections (1). In rehabilitation hospitals, the threat of antimicrobial-resistant microorganisms is a serious problem (2, 3). Patients in rehabilitation facilities are typically transferred from an acute care setting, where a high prevalence of multiple drug-resistant organisms exist (4). These patients also tend to have risk factors for nosocomial colonization or infection with antimicrobial-resistant organisms, such as advanced age, use of urinary catheters, and previous surgery or a history of antimicrobial therapy (5).
The urinary tract is one of the main sources of nosocomial infection and transmission of antimicrobial-resistant organisms in rehabilitation patients, because they generally use devices for urinary voiding due to functional or structural urological abnormalities (2, 6). Asymptomatic urinary colonization may not be a serious clinical problem for the patients themselves; however, because patients in rehabilitation hospitals share communal areas, such as physical therapy rooms, the transmission of resistant organisms can cause serious problems of nosocomial infection (7).
Previous studies of routine screening or active surveillance for antimicrobial-resistant strains in rehabilitation hospitals have focused on methicillin-resistant Stayphylococcus aureus (MRSA) and vancomycin-resistant Enterococcus (VRE), because these species are the main targets for preventing antimicrobial-resistance in hospitals (3, 8, 9). However, the current study used the definition of highly resistant microorganisms (HRMO) (10). The term HRMO was first introduced by the Dutch Working Party on Infection Control in 2005, in order to meet the need to control other pathogens with antibiotic resistance. In this respect, monitoring HRMO can be a more effective way of controlling hospital infections.
In the National Rehabilitation Center (NRC) of Korea, urine cultures are routinely requested on admission in order to screen for the presence of HRMO and to determine the need for surveillance and isolation of the patient. The aim of this study was to determine the prevalence and risk factors for HRMO in urinary isolates from patients who were newly transferred from other hospitals. This knowledge may help us to understand the epidemiology of antibiotic resistance and to develop effective policies for infection control and prevention.
METHODS
Setting and design
This study was performed at the NRC of Korea, which has a capacity of 300 beds. The institution is a freestanding hospital that specializes in rehabilitation treatment. It is a referral hospital that accepts patients from other hospitals throughout Korea.
The study design was a prospective screening of patients who were newly admitted to the centre during the 1-year period from June 2012 through May 2013. The study was approved by the Institutional Review Board of the NRC.
Patients and data collection
A total of 1,150 patients over 18 years of age were admitted to the NRC during the research period. Of these, 234 patients admitted from the community, mainly comprising patients with spinal cord injury (SCI) for annual urological examination, were excluded from the study. A total of 916 patients who were newly admitted from the other hospitals were included in the study.
Patients were largely categorized as patients with or without SCI. In patients with SCI (n = 232) the main cause of SCI was trauma, and other causes were spinal stenosis with myelopathy, spinal ischaemia, spinal tumour, infectious or transverse myelitis, and spina bifida. In patients without SCI (n = 634) the most common reason was brain injury associated with cerebrovascular accident, followed by traumatic brain injury, and peripheral neuromuscular diseases.
Urine samples for culture were collected from all patients on admission day. A clean-catch midstream technique was used for patients who were able to void (spontaneous voiding patients), and a sterile catheterization technique was used for patients who were incapable of voluntary bladder voiding (patients using condom, intermittent, or indwelling catheters). All specimens were cultured and isolates were identified at the authorized institute (Seoul Clinical Laboratories, Seoul, Korea). Significant bacteriuria was defined as presenting with 104 or more colony forming units (CFU) per ml. If urine culture exhibited less than 104 CFU/ml, the result was regarded as negative. Bacterial identification and antibiotic susceptibility testing were performed using the Vitek 2 system (BioMérieux, Durham, USA). Data were also collected on demographic characteristics, types of injury, presence of chronic illness, history of recent surgery, and types of urinary drainage systems.
Definition of highly resistant microorganisms
The definition of HRMO given by the Dutch Working Party on Infection Control in 2005 (10) was used in this study. The designation of HRMO is dependent on the bacterial species and their antimicrobial resistance. The criteria for the definition HRMO used in this study are summarized in Table I (11).
|
Table I. Definition of highly resistant microorganisms (HRMO) used in this study |
||||||||||
|
Organism |
ESBL |
IMI |
LEV |
AMK |
CFT |
PIP |
TMP-SMZ |
VAN |
PEN |
OXA |
|
Escherichia coli |
A |
A |
B |
B |
||||||
|
Klebsiella species |
A |
A |
B |
B |
||||||
|
Other Enterobacteriaceae |
A |
A |
B |
B |
B |
|||||
|
Acinetobacter species |
A |
B |
B |
B |
||||||
|
Pseudomonas species |
C |
C |
C |
C |
C |
|||||
|
Stenotrophomonas maltophilia |
A |
|||||||||
|
Enterococcus faecium |
B |
B |
||||||||
|
Staphylococcus aureus |
A |
|||||||||
|
Streptococcus pneumoniae |
A |
A |
||||||||
|
A: presence of ESBL production or resistance against this antibacterial agent is sufficient to define the HRMO; B and C: resistance against at least 2 and 3 of these antibacterial agents are required to define the HRMO, respectively. ESBL: extended-spectrum beta-lactamase; IMI: imipenem; LEV: levofloxacin; AMK: amikacin; CFT: ceftazidime; PIP: piperacillin; TMP-SMZ: trimethoprim-sulfamethoxazole; VAN: vancomycin; PEN: penicillin; OXA: oxacillin. |
||||||||||
Statistical analysis
Continuous data are presented as means (standard deviations (SD)) and categorical data as quantities and proportions. Factors potentially associated with HRMO were investigated using adjusted logistic regression analysis. A χ2 test was used to calculate odds ratios (OR) and 95% confidence intervals (95% CI) according to the number of risk factors associated with HRMO. Analysis was performed using STATA version 12.1 (StataCorp, College Station, TX, USA), and statistical significance was accepted for p-values < 0.05.
RESULTS
A total of 916 patients were included in the study. The mean age of the study group was 58.1 years (SD 15.7) and 60.9% were male. The baseline characteristics of the study group are summarized in Table II. At least one bacterial species was cultured in 413 (45.1%) patients and HRMO were isolated from 148 (16.2%) patients.
|
Table II. Characteristics and prevalence of highly resistant microorganisms (HRMO) in study population (n = 916) |
|
|
Variables |
Values |
|
Age, years, mean (SD) |
58.1 (15.7) |
|
Sex, n (%) Male Female |
558 (60.9) |
|
358 (39.1) |
|
|
Types of injury, n (%) SCI Non-SCI |
232 (25.3) |
|
684 (74.7) |
|
|
Underlying conditions, n (%) Hypertension Diabetes |
493 (53.8) |
|
243 (26.5) |
|
|
Recent surgery, n (%) Surgery in past 1 year |
383 (41.8) |
|
Voiding method, n (%) No catheter Condom catheter Intermittent catheterization Indwelling catheter |
660 (72.1) |
|
46 (5.0) |
|
|
91 (9.9) |
|
|
119 (13.0) |
|
|
Number of urinary isolates, n (%) Negative Single organism Double organisms |
503 (54.9) |
|
404 (44.1) |
|
|
9 (1.0) |
|
|
Prevalence of HRMOa, positive n (%) |
148 (16.2) |
|
aHRMO prevalence was positive if the subject had at least 1 of the HRMO in urinary isolates. SCI: spinal cord injury; SD: standard deviation. |
|
Among 422 urinary isolates, which comprised 404 single cultures and 9 double cultures from 413 patients, 150 (35.5%) were identified as HRMO (Table III). Gram-negative species had a higher number and ratio of HRMO, compared with Gram-positive species (141/325 (43.4%) vs 9/97 (9.3%)). Among 118 HRMO of the Enterobacteriaceae family, 97 isolates (82.2%) produced extended-spectrum beta-lactamase (ESBL), whereas there were no cases of carbapenem-resistant Enterobacteriaceae. In particular, more than half of the cultured isolates were identified as HRMO in Klebsiella (51/88, 58.0%) and Acinetobacter species (16/31, 51.6%).
|
Table III. Bacterial strains of urinary isolates (n = 422) and highly resistant microorganisms (HRMO) (n = 150) |
||
|
Bacterial strains |
Urinary isolates n |
HRMO n (%)a |
|
Gram-negative species |
325 |
141 (43.4) |
|
Enterobacteriaceae family |
268 |
118 (44.0) |
|
Escherichia coli |
130 |
56 (43.1) |
|
Klebsiella species |
88 |
51 (58.0) |
|
Other Enterobacteriaceae |
50 |
13 (26.0) |
|
Gram-negative non-fermentous |
57 |
23 (40.4) |
|
Acinetobacter species |
31 |
16 (51.6) |
|
Pseudomonas species |
22 |
6 (27.3) |
|
Stenotrophomonas maltophilia |
4 |
1 (25.0) |
|
Gram-positive species |
97 |
9 (9.3) |
|
Enterococcus species |
65 |
5 (7.7) |
|
Staphylococcus species |
21 |
4 (19.0) |
|
Streptococcus species |
11 |
0 (0) |
|
Total |
422 |
150 (35.5) |
|
aPercentage of HRMO among the cultured isolates of each strain. |
||
Multivariate logistic regression models are summarized in Table IV. First, the risk factors for HRMO among all admitted patients were investigated. The risk factors were: age over 60 years (OR = 1.9; 95% CI 1.2–2.9), female sex (OR = 2.3; 95% CI 1.5–3.4), surgery in the past year (OR = 1.6; 95% CI 1.9–2.4), and use of any type of urinary catheters. OR of condom catheter, intermittent catheterization, and indwelling catheter were 3.4 (95% CI 1.6–7.6), 2.8 (95% CI 1.4–5.6) and 5.4 (95% CI 3.2–9.4), respectively. Next, the risk factors for HRMO only among the patients with bacteriuria were investigated. The factors in this case were: surgery in the past year (OR = 1.6; 95% CI 1.0–2.6) and use of indwelling catheter (OR = 1.9; 95% CI 1.0–3.5).
|
Table IV. Multivariate analysis for factors associated with highly resistant microorganisms (HRMO) in urine cultures |
|||||
|
Factor |
Among all admitted patients (n = 916) |
Among patients with bacteriuria (n = 413) |
|||
|
ORa (95% CI) |
p-value |
ORb (95% CI) |
p-value |
||
|
Age > 60 years |
1.9 (1.2–2.9) |
0.003* |
1.4 (0.9–2.3) |
0.177 |
|
|
Female |
2.3 (1.5–3.4) |
< 0.001* |
1.1 (0.71–0.7) |
0.725 |
|
|
Spinal cord injury |
0.7 (0.5–1.5) |
0.631 |
0.7 (0.4–1.3) |
0.256 |
|
|
Hypertension |
0.7 (0.5–1.1) |
0.114 |
0.7 (0.4–1.2) |
0.133 |
|
|
Diabetes |
1.1 (0.7–1.7) |
0.801 |
1.0 (0.5–1.5) |
0.731 |
|
|
Surgery in the past year |
1.6 (1.9–2.4) |
0.019* |
1.6 (1.0–2.6) |
0.035* |
|
|
Condom catheter |
3.4 (1.6–7.6) |
0.002* |
1.4 (0.5–3.3) |
0.514 |
|
|
Intermittent catheterization |
2.8 (1.4–5.6) |
0.004* |
1.1 (0.5–2.4) |
0.789 |
|
|
Indwelling catheter |
5.4 (3.2–9.4) |
< 0.001* |
1.9 (1.0–3.5) |
0.042* |
|
|
*p < 0.05. a148 patients with HRMO (case group) were compared with 768 patients without HRMO (control group). b148 patients with HRMO (case group) were compared with 265 patients with non-HRMO (control group). OR: odds ratio; 95% CI: 95% confidence interval. |
|||||
The prevalence of HRMO increased with the number of risk factors involved: (i) age over 60 years; (ii) female sex; (iii) surgery in the past year; and (iv) use of any type of urinary catheters (Fig. 1). The OR for prevalence of HRMO in patients with 2 or more risk factors was 4.1 (95% CI 2.7–6.1), compared with those with single or no risk factors.
DISCUSSION
The aim of this study was to investigate the prevalence and risk factors of HRMO in urinary isolates from newly admitted patients to the rehabilitation hospital. We found that 16.2% of patients were colonized with HRMO, and HRMO were predominantly composed of Gram-negative species. Age over 60 years, female sex, recent surgery, and use of any type of urinary catheter were risk factors, and patients with 2 or more risk factors were at approximately 4 times the risk for HRMO, compared with those with single or no risk factors.
Approximately one-sixth of admitted patients were positive for HRMO in urine cultures, and approximately one-third of the isolates cultured were HRMO. Patients in the rehabilitation hospitals had a somewhat higher risk for colonization with HRMO. However, it was difficult to compare the prevalence of HRMO in this study with the findings of other studies because of the variation in the definition of the resistant organisms. Previous studies of the prevalence of antibiotic-resistant organisms in rehabilitation hospitals or long-term care facilities mostly focused on individual species, such as MRSA, VRE, or multidrug-resistant Gram-negative rods (MDR-GNR), whereas HRMO in this study cover the entire spectrum of clinically relevant bacteria (3, 8, 12–14). Futures studies should use a uniform definition of the resistant organisms in order to compare the degrees of antibiotic-resistance between hospitals.
Although Gram-positive species, such as MRSA or VRE, have been a major concern in infection control and prevention, this study showed that Gram-negative species predominantly accounted for HRMO in a rehabilitation hospital. Recently, there has been marked increase in the number of patients in tertiary care hospitals who harbour MDR-GNR (15). Another recent study demonstrated that healthcare costs in patients with MDR-GNR were even higher than those in patients with MRSA (16). Rehabilitation hospitals need to consider highly-resistant Gram-negative organisms as well as MRSA and VRE in active surveillance or contact isolation programmes.
Gram-negative species accounted not only for the majority of total HRMO, but also contained a high proportion of HRMO in each strain. ESBL was the most relevant determinant of resistance in the Enterobacteriaceae family in our study. This is of particular concern because infections with ESBL-producing strains have a significant impact on increased morbidity, mortality and healthcare-associated costs (17). In particular, the numbers of HRMO among Klebsiella and Acinetobacter species were more than half of the total cultured organisms. The prevalence of ESBL has been known to be higher in Klebsiella species than in other Enterobacteriaceae family including E. coli (18). Quinolone and carbapenem resistance rates in Acinetobacter species also increased drastically in Korea (19). These factors might contribute to the high prevalence of HRMO in Klebsiella and Acinetobacter species.
In this study, age over 60 years, female sex, recent surgery, and use of urinary catheters were found to be risk factors for HRMO colonization. Some of these factors, such as age over 60 years or female sex, may be attributed to the high prevalence of bacteriuria in these patients. However, recent surgery and indwelling urinary catheters remain the significant risk factors, even among patients with bacteriuria, and these findings are consistent with previous studies (20–22). Thus, reducing the inappropriate use of catheters may be helpful, not only in the prevention of urinary tract infection, but in decreasing the reservoir of HRMO (23). The factors of surgical history and urinary catheter reflect the fact that many HRMO-colonized patients required intensive procedures and therapies with antibiotics. The prevalence of HRMO increased with the number of risk factors. The identification of risk factors can therefore help in determining which patients need an active surveillance programme.
Study limitations
This study has several limitations. First, patients underwent HRMO screening cultures of the urine only. Cultures from other sites, such as the nasal and perianal areas, were not performed, thus there was a lower rate of detection of Gram-positive species, including MRSA and VRE. Secondly, the study did not investigate the prior use of antibiotics, due to lack of records from previous hospitals. Antimicrobial therapy is the single most important factor for colonization by resistant organisms (5). Prior surgery or urinary catheters as risk factors may indirectly reflect the effect of antibiotic use on resistance manifestation; however, the direct relationship between prior antimicrobial therapy and HRMO colonization was not clearly identified in this study. Thirdly, the presence of urinary symptoms was not investigated on admission; therefore we could not perform analysis of HRMO related to urinary symptoms. Finally, the present study did not address the consequences of HRMO colonization. A further prospective study is therefore needed to verify the clinical impact of HRMO colonization on patients’ clinical outcomes and hospital infection.
Conclusion
In general, active surveillance for HRMO is recommended for selected patients, particularly in intensive care units (10). Based on the results of this study, we recommend that routine screening of urine culture should be performed in rehabilitation patients with 2 or more of the following risk factors: age over 60 years, female sex, recent surgery, and use of urinary catheters. In addition, further studies are needed to develop effective infection control programmes for reducing the transmission of HRMO among rehabilitation patients.
Conflicts of interest
No financial supports or grants were received for this study, and the authors have no conflicts of interest to declare.
REFERENCES
