Sonja de Groot, PhD1,2, Riemer J. K. Vegter, MSc2, Coen Vuijk, BASc3, Frank van Dijk, MSc2, Corien Plaggenmarsch, MSc2, Maurits Sloots, OT, PhD1, Janneke Stolwijk-Swüste, MD, PhD1, Ferry Woldring, PT4, Marga Tepper, MD4 and Lucas H. V. van der Woude, PhD2,4
From the 1Amsterdam Rehabilitation Research Center, Reade, Amsterdam, 2University of Groningen, University Medical Center Groningen, Center for Human Movement Sciences, 3Motion Matters, Wapserveen and 4Center for Rehabilitation, University of Groningen, University Medical Center Groningen, Groningen, The Netherlands
OBJECTIVE: To describe the enabling factors and barriers experienced in the Wheelchair Expert Evaluation Laboratory – implementation (WHEEL-i) project, in which scientific knowledge, tools and associated systematic analyses of hand-rim wheelchair propulsion technique, user’s wheelchair propulsion capacity, wheelchair-user interface, and wheelchair mechanics were implemented in 2 rehabilitation centres.
DESIGN: Implementation project.
Patients: Spinal cord injury.
METHODS: In this implementation project standardized tests were performed: wheelchair skills tests, 2 questionnaires, and a steady-state exercise test on a treadmill in which propulsion technique (forces and torques) and physical strain (oxygen uptake, heart rate and mechanical efficiency) were measured.
RESULTS: Good interpretation of the test outcomes was the most important barrier. In order to discuss individual wheelchair performance results with patients and clinicians, reference data were developed, smallest detectable differences were calculated and software was developed to simultaneously show video recordings and force and torque signals.
CONCLUSION: Based on pilot results, the greatest barrier to systematic monitoring of the individual wheelchair fitting and learning process in rehabilitation with, among others, instrumented measurement wheels, was interpretation of outcomes. For proper interpretation of individual outcomes, the availability of reference data, smallest detectable differences and visualization of outcomes is of utmost importance.
Key words: wheelchair; physical strain; propulsion technique; rehabilitation; clinical testing; smallest detectable difference; reference data.
J Rehabil Med 2014; 46: 493–503
Correspondence address: S. de Groot, Amsterdam Rehabilitation Research Center, Reade, PO Box 58271, NL-1040 HG Amsterdam, The Netherlands. E-mail: s.d.groot@reade.nl
Accepted Jan 21, 2014; Epub ahead of print May 8, 2014
INTRODUCTION
Wheeled mobility is of crucial importance to a growing population of lower-limb impaired and often ageing individuals worldwide. The vast majority of this population in the Western world will use hand-rim wheelchairs. Upper-body exercise, especially hand-rim propulsion, is far more straining and less mechanically efficient than leg work (1, 2). This low efficiency, together with the often low physical capacity of the user, leads to high physical strain in daily life and, subsequently, a limited radius of action. Furthermore, hand-rim wheelchair propulsion often leads to upper-body overuse complaints. For example, 30–40% of people with a spinal cord injury indicated shoulder pain during and in the year after rehabilitation (3). This is probably due to the high mechanical strain on the glenohumeral joint during wheelchair propulsion and wheelchair-related activities, such as making a transfer, which may lead to joint damage in the long term (4).
To prevent overuse injuries and to obtain and maintain mobility and develop an active lifestyle, both wheelchair (e.g. mass, tyre pressure) and user (e.g. fitness, skills in terms of negotiating a slope or mounting a kerb, propulsion technique in terms of force application on the rim) must be in the best condition. Furthermore, the wheelchair-user interface (e.g. seat height, rim and wheel diameter) needs to be ergonomically tuned to the best wheeling performance in different environments for the specific individual (5) (Fig. 1).
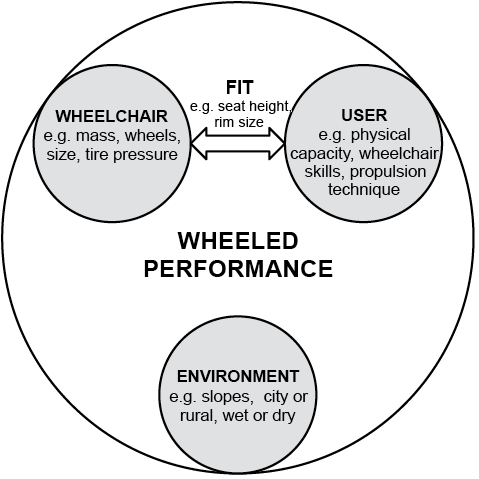
Fig. 1. Model indicating that wheelchair performance is dependent on a number of different factors.
Despite a considerable number of studies by several research groups into wheelchair propulsion over the last 30 years (6–11), to date wheelchair fitting is a personalized professional skill that has little scientific foundation. Furthermore, monitoring the propulsion technique and physical strain of new wheelchair users in Dutch rehabilitation is not common practice. However, this approach can be useful to optimize the wheelchair, the interface, and to educate the user in establishing the best propulsion technique, to improve physical capacity and skill and prevent upper-extremity overuse injuries. This essentially points towards a global aim whereby wheelchair users can engage more actively in society.
The use of objective standardized measurements at an individual level, to quantify the results of rehabilitation and as part of evidence-based rehabilitation practice, is seen as an increasingly important part of good clinical practice. Therefore, monitoring patients with different tests is increasingly common in rehabilitation practice (12), even with very sophisticated measurement techniques. Nowadays, many rehabilitation centres have a gait analysis laboratory to investigate and optimize the walking pattern (e.g. ground reaction force, muscle activity, joint angles) and capacity of individual patients. Similar measurements can be performed in a wheelchair propulsion analysis laboratory, the only difference is that the focus is on the upper body and the applied forces and torques are, therefore, measured on the hand-rim. Today, these forces can be measured quite easily with commercially available measurement wheels, such as the SmartWheel (Three Rivers Holdings, Mesa, AZ, USA) and the Optipush (Max Mobility, LLC, Antioch, TN, USA) (Fig. 2). These wheels can be attached easily to most wheelchairs.
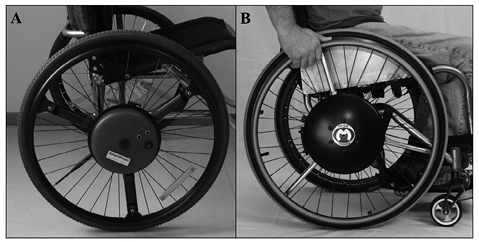
Fig. 2. Two commercially available measurement wheels. (A) SmartWheel and (B) Optipush.
In several clinics in the USA measurements with an instrumented wheel (SmartWheel) are implemented (13). They use a standard protocol that consists of 4 basic elements (propulsion over tiles, carpet, up a ramp, and through a figure-of-8). Unfortunately, the protocol is not standardized regarding velocity and power output, which makes it difficult to interpret differences in propulsion technique and physical strain due to interventions at the level of the wheelchair or user. For this reason the clinical SmartWheel User Group (SWUG) protocol was not employed; instead a standardized protocol with a steady-state wheelchair exercise test on a treadmill, in addition to skill testing and questionnaires to measure shoulder pain and self-efficacy in wheeled mobility, was employed. All Dutch specialized spinal cord injury rehabilitation units have had a wheelchair-specific treadmill since the start of this century (14).
In the context of today’s scientific knowledge and understanding in wheelchair propulsion linked to the availability of measurement wheels, the Wheelchair Expert Evaluation Laboratory – implementation (WHEEL-i) project was undertaken. The objective of this project was to implement a systematic analysis of the user, the wheelchair-user interface as well as the wheelchair mechanics in the clinical setting of two Dutch rehabilitation centres analogous to gait analysis, using evidence-based techniques and experimental strategies. The aims of the present study were to describe: (i) the test protocol that is used in WHEEL-i; and (ii) the enabling factors and barriers to successful implementation of WHEEL-i.
METHODS
Implementation
Two Dutch rehabilitation centres participated in the WHEEL-i “innovation in rehabilitation” project. Within each centre a WHEEL-i work group was formed to discuss how the project could best be implemented in the specific centre. These work groups consisted of a rehabilitation physiatrist, physical therapist, occupational therapist, rehabilitation technician, human movement scientist in the field of wheelchair propulsion and a professional in wheelchair fitting. These work groups defined the test protocol, how the project could best be implemented in the rehabilitation centres and discussed the implementation process.
Tests protocol
After several meetings with the work group, the following tests were chosen for WHEEL-i: a wheelchair circuit, two questionnaires to assess shoulder pain and self-efficacy of wheeled mobility and a submaximal exercise test on a treadmill to measure propulsion technique and physical strain. Since it is important to perform the test in a standardized manner on each test occasion (e.g. regarding speed and resistance), a manual with information about the test procedure and the execution of the different test protocols was developed specifically for the WHEEL-i project (available to download from www.scionn.nl). Furthermore, clearly defined explanations of the meaning of each test variable are provided in the manual, and examples of these can be seen in Figs 3 and 4 and Table I.
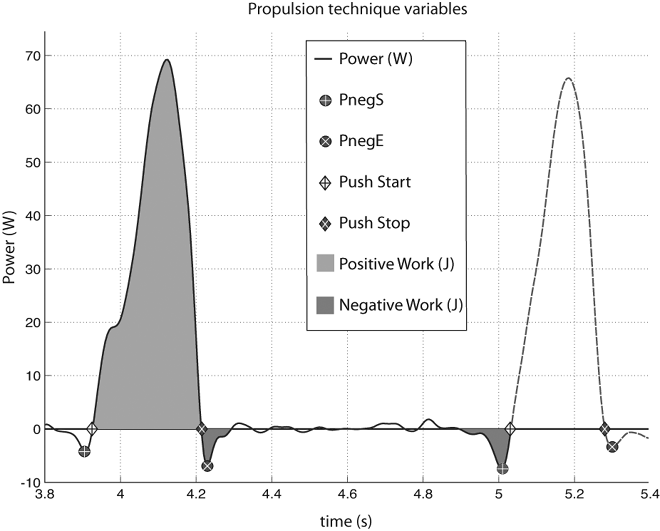
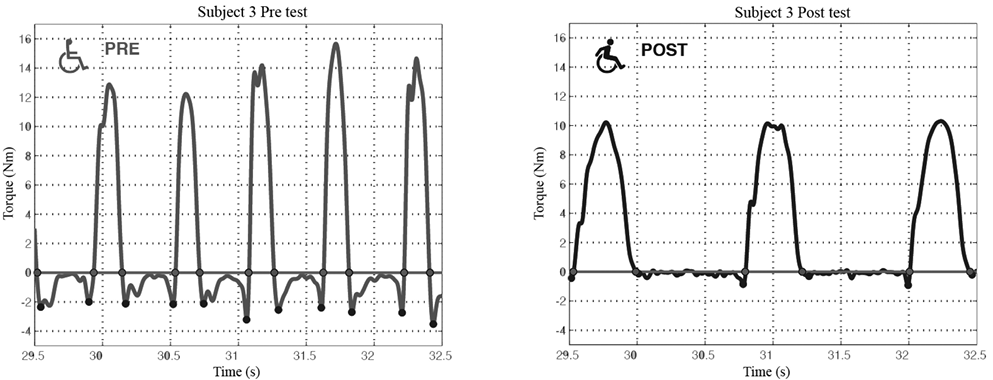
Fig. 4. Torque around the wheel axle. Typical example of changes from pre- to post-test over a learning period (3 weeks, 3 times a week, 80 min in total): e.g. a lower push frequency, higher push time and cycle time, less braking torque before and after the push, and a lower peak torque.
|
Table I. Possible outcome variables from measurement wheels |
|
|
Variable |
Description |
|
Push time, s |
Time from the start of positive torque to the stop of positive torque for an individual push |
|
Cycle time, s |
Time from the start of positive torque to the next start of positive torque |
|
Relative push time, % |
Push time expressed as percentage of the cycle time |
|
Push frequency, push/min |
Number of complete pushes per minute |
|
Contact-angle, º |
Angle at the end of a push minus the angle at the start |
|
Fpeak, N |
3D peak force within the push phase |
|
Fmean, N |
3D mean force within the push phase |
|
FEFmean, % |
Mean fraction effective force |
|
FEFmax, % |
Maximum fraction effective force |
|
Slope, Nm/s |
Rate of rise from the start of the push phase to the maximum delivered torque around the axle |
|
Negative dip before push phase, N |
Minimum torque preceding the push phase |
|
Negative dip after push phase, N |
Minimum torque following the push phase |
|
Work/push, J |
The power integrated over the push. |
|
POmean push phase, W |
Mean power output within the push phase |
|
POmax push phase, W |
Maximum power output within the push phase |
|
Power output 2-sided, W |
Mean power output of 2 wheels during the sample period |
|
Energy expenditure, W |
Calculated from the oxygen uptake and respiratory exchange ratio according to Garby & Astrup (21) |
|
Mechanical efficiency, % |
Percentage of internal power used for external power delivered at the wheels |
Tests were always performed twice in order to investigate the effect of change over the course of an intervention. When the intervention was a learning or training period the time between the pre- and post-test could be weeks (Fig. 5). When different wheelchair configurations were tested, the time between test conditions was shorter, i.e. on the same day or within a few days, in order to diminish the possible confounding effect of learning or training on the outcome measures (Fig. 5). Prior to all testing, the wheelchair users were screened by a physician for any contra-indications regarding the exercise tests. Furthermore, the wheelchair users signed an informed consent before undertaking any testing.
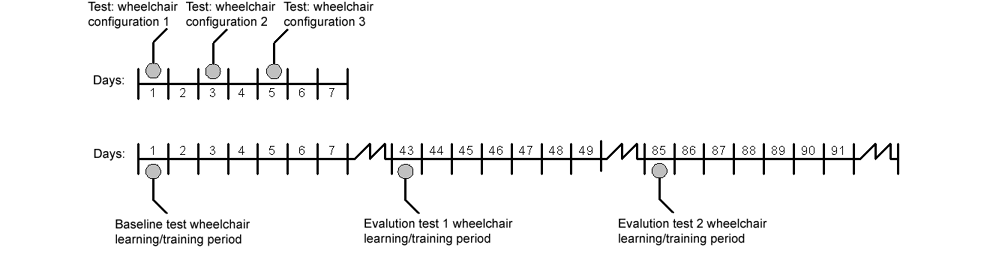
Fig. 5. Difference in time schedule when testing different wheelchair configurations (within days, upper time line) or the effect of a learning/training intervention (over weeks, lower time line).
Wheelchair circuit
The wheelchair circuit (15, 16) is a test to assess manual wheelchair skill performance. The research version of the wheelchair circuit consists of 8 different standardized tasks. The 8 tasks are: (i) figure-of-8 shape, (ii) crossing a doorstep (height 0.04 m), (iii) mounting a platform (height 0.10 m), (iv) 15-m sprint, (v) transfer, (vi) negotiating a 3% slope on a treadmill, (vii) negotiating a 6% slope on a treadmill, (viii) propelling the wheelchair for 3 min on a treadmill at a constant velocity of 0.56, 0.83, or 1.11 m/s, depending on the participant’s ability. The wheelchair circuit leads to an ability score and performance time score. All standardized tasks are scored on the ability to perform the task. When the task is performed independently and within a certain time 1 point is assigned, otherwise the score is 0. Three items (crossing a doorstep, mounting a platform, transfer) can also be scored as partially able and can be given half a point. Points for all 8 tasks are summed to give an overall ability score, ranging from 0 to 8. The performance time score is the sum of the performance times of the figure-of-8 shape and the 15-m sprint. Participants are instructed to perform these two tasks at their maximum speed. The wheelchair circuit outcome measures have been shown previously to be sensitive to change (17).
Questionnaires
The Dutch versions of the Wheelchair User Shoulder Pain Index (WUSPI) (18) and Self-Efficacy in Wheeled Mobility Scale (SEWM) (19, 20) were selected and administered during the pre- and post-tests when a longer (i.e. learning/training) intervention is evaluated. The WUSPI is a 15-item self-report survey specifically designed to assess shoulder pain in wheelchair users during daily functional activities with a 10-point visual analogue scale (18).
The SEWM is a 10-item scale on which respondents rate how confident they are with regard to the performance of specific and general wheeled mobility skills on a 4-point Likert scale (1 = not at all true, 2 = rarely true, 3 = moderately true, 4 = always true) (19, 20).
Steady-state exercise test
With a steady-state exercise test the propulsion technique and physical strain can be determined. It was decided to perform this test on a treadmill because the velocity and resistance, which both have an effect on propulsion technique and physical strain, can be standardized under different test conditions.
The submaximal exercise test protocol of the Dutch multi-centre prospective cohort study “Restoration of mobility in SCI rehabilitation” was used (14). This protocol consists of two 3-min submaximal exercise blocks with 2-min rest between blocks. The velocity of the exercise blocks is dependent on lesion level as well as overall functional status and is set to 0.56, 0.83 or 1.11 m/s. For each person the same test conditions are applied on all test occasions.
In the first 3-min exercise block, the person propels the wheelchair with a pre-determined velocity and 0º treadmill slope. After completion, the person rests for 2 min before starting the second 3-min exercise block, which is performed at the same velocity and a 0.36º treadmill slope. Metabolic cost and heart rate are continuously measured during the exercise blocks using a metabolic cart (Oxycon Delta, CareFusion, San Diego, USA) and Polar Sport Testers (Polar Electro Oy, Kempele, Finland), respectively. Calibration with standardized gases and a 3-litre volume syringe is performed prior to testing.
During the last minute of each exercise block the forces and torques applied on the right-hand rim are measured by the Optipush. The patient performs the test in his own wheelchair with the Optipush wheel attached (24-, 25- and 26-inch options available) on the right-hand side and a regular wheel with extra mass, with similar inertia as the Optipush wheel, on the left-hand side. After the measurement, the Optipush software can automatically generate a report with the averaged values of several propulsion technique variables, such as cadence, braking torque, peak force and torque, contact angle and power. This report was used by the rehabilitation professionals.
The energy expenditure (En) is calculated from the oxygen uptake and the respiratory exchange ratio (RER) according to Garby & Astrup (21). Energy expenditure is calculated over the last minute of each exercise block. To obtain the gross mechanical efficiency (ME) of wheelchair propulsion, the ratio power output (PO)/energy expenditure (En) is calculated according to the following equation:
ME = PO × En–1 × 100 (%)
The power output is calculated from the Optipush, as the product of the torque around the wheel axle and the angular velocity, and is expressed as the mean power output during the last minute of the exercise block (from start of the first push until start of the last push in that minute). This power output is multiplied by 2 to calculate the overall power output (for 2 wheels).
The measures of physical strain are the submaximal oxygen uptake, heart rate and ME during the last minute of the exercise blocks.
Reference values and smallest detectable difference
To interpret the individual test results, previously collected data were used for calculating reference values and the smallest detectable differences (SDD) of different test outcomes (Table II).
|
Table II. Characteristics of the wheelchair–user combination and their influence on rolling friction (26) |
|
|
Characteristics |
Effect on rolling friction |
|
Body mass↑ |
↑ |
|
Wheelchair mass↑ |
↑ |
|
Tyre pressure↓ |
↑ |
|
Wheel size↑ |
↓ |
|
Hardness floor↓ |
↑ |
|
Camber angle ↑ |
? |
|
Toe-in/out↑ |
↑↑ |
|
Castor shimmy↑ |
↑ |
|
Centre of mass over large rear wheels |
↓ |
|
Folding frame (vs box frame) |
↑ |
|
Maintenance↓ |
↑ |
Reference values regarding wheelchair skills were calculated from the data of the Dutch multi-centre study “Restoration of mobility in SCI rehabilitation” (22). Ethics approval for the multi-centre SCI study was received from the medical ethics committee of SRL/iRv Hoensbroeck. The protocols for the wheelchair circuit (15, 16) and gross mechanical efficiency (23) in WHEEL-i were identical to the protocols in the multi-centre SCI study. Reference values were calculated as percentiles (20th, 40th, 60th, and 80th, percentile) besides the mean and standard deviation for different lesion groups (motor complete and incomplete paraplegia or tetraplegia).
For the calculation of the SDD, data of a study on able-bodied participants was used. This study was approved by the local ethics committee, of the Center for Human Movement Sciences, University Medical Center Groningen, University of Groningen, The Netherlands.
The intraclass correlation (ICC), standard error of the measurement (SEM) and SDD were determined with data of experienced able-bodied person (n = 56) who practiced wheelchair propulsion on a treadmill for 3 weeks (68 min in total). Physiological and propulsion technique data were collected after this practice period with a protocol that consisted of 3 4-min wheelchair propulsion on a treadmill at a power output of 0.18 W/kg with 2 min rest in between. With variance component analysis the ICC, SEM and SDD were calculated (24) when using one exercise test, or 2 or 3 exercise tests and using the mean.
Participants in both studies provided written informed consent.
RESULTS
Reference data
For the wheelchair circuit (performance time score (Table III), ability score (Table IV)) and gross mechanical efficiency (Tables V–VI), reference values for 4 test occasions during and after rehabilitation are shown in Tables III–VI. The reference values are shown for people with tetraplegia or paraplegia and with a motor complete or incomplete lesion at the start of active rehabilitation (when people can sit for ≥ 3 h), 3 months after the start, at discharge of inpatient rehabilitation and 1 year after discharge. It is important to note that not every participant was able to perform the test on each test occasion. The percentage of participants within the lesion groups that was able to perform the test at a specific test occasion is visualized in the table by the column “% all part”. For example, only 10 persons with a complete tetraplegia, i.e. 19% of all participants with a complete tetraplegia in the study, were able to perform the submaximal exercise block at the start of active rehabilitation (Table V). Thus, if a person with a complete tetraplegia is able to perform the exercise test at the start of active rehabilitation, then they are already very good at that task and the reference data should be used with caution.
|
Table III. Reference values for persons with spinal cord injury (SCI) for the performance time score of the wheelchair circuit at different times after the start of active spinal cord injury rehabilitation (22) |
|||||||
|
|
n |
% all part |
20th percentile Excellen–Good |
40th percentile Good–Average |
60th percentile Average–Fair |
80th percentile Fair–Poor |
Mean (SD) |
|
Performance time score start active rehabilitation |
|||||||
|
Tetraplegia |
|||||||
|
Complete |
18 |
34.0 |
28.8 |
40.4 |
48.0 |
68.4 |
48.9 (21.9) |
|
Incomplete |
16 |
51.6 |
22.4 |
27.0 |
38.0 |
66.2 |
43.3 (28.0) |
|
Paraplegia |
|||||||
|
Complete |
66 |
77.7 |
17.4 |
21.0 |
24.2 |
33.8 |
26.2 (11.7) |
|
Incomplete |
30 |
83.3 |
18.0 |
22.4 |
28.0 |
36.8 |
30.5 (19.5) |
|
Performance time score 3 months after the start of active rehabilitation |
|||||||
|
Tetraplegia |
|||||||
|
Complete |
21 |
60.0 |
24.2 |
31.0 |
37.6 |
56.6 |
39.6 (17.9) |
|
Incomplete |
14 |
51.9 |
25.0 |
27.0 |
33.0 |
42.0 |
34.3 (12.7 |
|
Paraplegia |
|||||||
|
Complete |
49 |
92.5 |
15.0 |
17.0 |
20.0 |
26.0 |
20.7 (8.3) |
|
Incomplete |
19 |
95.0 |
16.0 |
21.0 |
26.0 |
38.0 |
25.1 (10.3) |
|
Performance time score at discharge of inpatient rehabilitation |
|||||||
|
Tetraplegia |
|||||||
|
Complete |
24 |
72.7 |
19.0 |
25.0 |
29.0 |
38.0 |
28.3 (10.3) |
|
Incomplete |
22 |
73.3 |
18.0 |
24.2 |
27.0 |
34.8 |
28.7 (13.1) |
|
Paraplegia |
|||||||
|
Complete |
64 |
91.4 |
14.0 |
16.0 |
18.0 |
22.0 |
19.1 (7.8) |
|
Incomplete |
26 |
92.9 |
13.4 |
15.0 |
17.0 |
20.6 |
17.2 (4.6) |
|
Performance time score at 1 year after discharge of inpatient rehabilitation |
|||||||
|
Tetraplegia |
|||||||
|
Complete |
9 |
75.0 |
13.0 |
29.0 |
35.0 |
43.0 |
30.3 (13.7) |
|
Incomplete |
10 |
71.4 |
22.0 |
25.0 |
30.2 |
33.8 |
27.2 (7.2) |
|
Paraplegia |
|||||||
|
Complete |
39 |
90.7 |
13.0 |
15.0 |
17.0 |
19.0 |
18.9 (10.4) |
|
Incomplete |
17 |
81.0 |
13.0 |
15.4 |
17.0 |
24.4 |
19.9 (10.7) |
|
% all part: percentage of participants who were able to perform the test from the total number of participants (within the specific lesion group) of the study. E.g. only 34% of all participants with a complete tetraplegia in our study were able to perform the 15-m sprint and figure-of-8 at the start of active rehabilitation; SD: standard deviation. |
|||||||
|
Table IV. Reference values for persons with spinal cord injury (SCI) for the ability score of the wheelchair circuit at different times after the start of active spinal cord injury rehabilitation (22) |
|||||||
|
|
n |
% all part |
20th percentile Poor–Fair |
40th percentile Fair–Average |
60th percentile Average–Good |
80ß percentile Good–Excellent |
Mean (SD) |
|
Ability score start active rehabilitation |
|||||||
|
Tetraplegia |
|||||||
|
Complete |
37 |
69.8 |
0.0 |
0.0 |
2.0 |
2.7 |
1.3 (1.3) |
|
Incomplete |
20 |
64.5 |
1.2 |
2.0 |
3.3 |
4.0 |
2.7 (1.3) |
|
Paraplegia |
|||||||
|
Complete |
71 |
83.5 |
2.0 |
3.0 |
3.6 |
4.5 |
3.2 (1.3) |
|
Incomplete |
30 |
83.3 |
3.0 |
3.2 |
4.0 |
4.4 |
3.6 (0.8) |
|
Ability score 3 months after the start of active rehabilitation |
|||||||
|
Tetraplegia |
|||||||
|
Complete |
30 |
85.7 |
0.0 |
2.0 |
2.3 |
3.4 |
2.0 (1.6) |
|
Incomplete |
20 |
74.1 |
0.0 |
2.2 |
3.0 |
3.9 |
2.3 (1.7) |
|
Paraplegia |
|||||||
|
Complete |
49 |
92.5 |
3.0 |
4.0 |
4.5 |
5.0 |
4.0 (1.3) |
|
Incomplete |
19 |
95.0 |
3.0 |
4.0 |
4.5 |
5.0 |
4.0 (1.0) |
|
Ability score at discharge of inpatient rehabilitation |
|||||||
|
Tetraplegia |
|||||||
|
Complete |
28 |
84.9 |
2.0 |
2.5 |
3.0 |
4.5 |
2.8 (1.4) |
|
Incomplete |
27 |
90.0 |
1.6 |
3.6 |
4.0 |
4.5 |
3.3 (1.6) |
|
Paraplegia |
|||||||
|
Complete |
68 |
97.1 |
3.5 |
4.5 |
5.0 |
5.0 |
4.2 (1.3) |
|
Incomplete |
25 |
89.3 |
4.5 |
4.5 |
5.0 |
5.0 |
4.7 (0.4) |
|
Ability score at 1 year after discharge of inpatient rehabilitation |
|||||||
|
Tetraplegia |
|||||||
|
Complete |
10 |
83.3 |
2.0 |
2.7 |
4.3 |
4.9 |
3.4 (1.6) |
|
Incomplete |
11 |
78.6 |
0.8 |
2.0 |
4.1 |
4.5 |
3.0 (1.8) |
|
Paraplegia |
|||||||
|
Complete |
40 |
93.0 |
4.0 |
5.0 |
5.0 |
5.0 |
4.5 (1.1) |
|
Incomplete |
17 |
81.0 |
4.3 |
4.5 |
5.0 |
5.0 |
4.7 (0.4) |
|
% all part: percentage of participants who were able to perform the test from the total number of participants (within the specific lesion group) of the study; SD: standard deviation. |
|||||||
|
Table V. Reference values for persons with spinal cord injury (SCI) for the gross mechanical efficiency during submaximal exercise block 1 at different times after the start of active spinal cord injury rehabilitation (22). The velocity was set at 0.56 m/s for people with a tetraplegia, at 1.11 m/s for those with paraplegia and, if that was too fast, at 0.83 m/s. The velocity was standardized within a patient for all test occasions. The mean power output is shown in the table |
|||||||
|
n |
% all part |
20th percentile Poor–Fair |
40th percentile Fair–Average |
60th percentile Average–Good |
80th percentile Good–Excellent |
Mean (SD) |
|
|
Gross mechanical efficiency at start of active rehabilitation, mean: 6W |
|||||||
|
Tetraplegia |
|||||||
|
Complete |
10 |
19 |
2.1 |
2.8 |
3.0 |
4.1 |
3.0 (1.1) |
|
Incomplete |
11 |
37 |
1.8 |
2.6 |
3.9 |
4.0 |
3.0 (1.1) |
|
Paraplegia |
|||||||
|
Complete |
54 |
56 |
3.4 |
4.7 |
5.0 |
5.4 |
4.6 (1.4) |
|
Incomplete |
28 |
72 |
2.5 |
3.4 |
4.1 |
5.6 |
4.0 (1.8) |
|
Gross mechanical efficiency 3 months after the start of active rehabilitation, mean: 6W |
|||||||
|
Tetraplegia |
|||||||
|
Complete |
16 |
33 |
1.6 |
2.2 |
3.0 |
4.6 |
2.9 (1.4) |
|
Incomplete |
6 |
29 |
2.4 |
2.5 |
2.8 |
3.3 |
2.7 (0.4) |
|
Paraplegia |
|||||||
|
Complete |
52 |
81 |
3.9 |
4.8 |
5.4 |
6.3 |
5.1 (2.0) |
|
Incomplete |
18 |
86 |
3.1 |
3.5 |
4.3 |
5.1 |
4.1 (1.2) |
|
Gross mechanical efficiency at discharge of inpatient rehabilitation, mean: 11W |
|||||||
|
Tetraplegia |
|||||||
|
Complete |
23 |
47 |
2.2 |
2.9 |
3.3 |
4.2 |
3.2 (1.0) |
|
Incomplete |
12 |
52 |
1.8 |
2.2 |
3.2 |
4.1 |
3.0 (1.4) |
|
Paraplegia |
|||||||
|
Complete |
67 |
77 |
3.7 |
4.5 |
5.2 |
6.1 |
4.9 (2.1) |
|
Incomplete |
28 |
85 |
2.8 |
4.2 |
4.7 |
5.7 |
4.4 (1.5) |
|
Gross mechanical efficiency at 1 year after discharge of inpatient rehabilitation, mean: 10W |
|||||||
|
Tetraplegia |
|||||||
|
Complete |
9 |
24 |
2.5 |
2.8 |
2.9 |
5.3 |
3.4 (1.3) |
|
Incomplete |
6 |
38 |
1.9 |
2.0 |
3.0 |
5.0 |
3.0 (1.5) |
|
Paraplegia |
|||||||
|
Complete |
55 |
76 |
3.9 |
4.9 |
5.5 |
6.6 |
5.3 (2.0) |
|
Incomplete |
16 |
57 |
3.0 |
4.3 |
4.9 |
6.0 |
4.5 (1.7) |
|
% all part: percentage of participants who were able to perform the test from the total number of participants (within the specific lesion group) of the study; SD: standard deviation. |
|||||||
|
Table VI. Reference values for persons with spinal cord injury (SCI) for the gross mechanical efficiency during submaximal exercise block 2 at different times after the start of active spinal cord injury rehabilitation (22). The velocity was set at 0.56 m/s for people with a tetraplegia, at 1.11 m/s for those with paraplegia and, if that was too fast, at 0.83 m/s. The velocity was standardized within a patient for all test occasions. The mean power output is shown in the table |
|||||||
|
n |
% all part |
20th percentile Poor–Fair |
40th percentile Fair–Average |
60th percentile Average–Good |
80th percentile Good–Excellent |
Mean (SD) |
|
|
Gross mechanical efficiency at start of active rehabilitation, mean: 8W |
|||||||
|
Tetraplegia |
|||||||
|
Complete |
9 |
17 |
2.9 |
3.6 |
4.4 |
5.6 |
4.1 (1.1) |
|
Incomplete |
11 |
37 |
2.8 |
3.1 |
5.0 |
5.4 |
4.1 (1.4) |
|
Paraplegia |
|||||||
|
Complete |
48 |
49 |
5.2 |
6.2 |
6.5 |
7.2 |
6.3 (1.5) |
|
Incomplete |
27 |
69 |
4.1 |
5.1 |
6.4 |
7.3 |
5.7 (1.8) |
|
Gross mechanical efficiency 3 months after the start of active rehabilitation, mean: 9W |
|||||||
|
Tetraplegia |
|||||||
|
Complete |
18 |
38 |
3.2 |
4.1 |
4.4 |
5.4 |
4.3 (1.4) |
|
Incomplete |
6 |
29 |
3.5 |
3.7 |
5.1 |
5.7 |
4.5 (1.0) |
|
Paraplegia |
|||||||
|
Complete |
50 |
78 |
5.3 |
6.2 |
7.0 |
7.9 |
6.9 (3.8) |
|
Incomplete |
18 |
86 |
4.6 |
5.3 |
6.1 |
6.5 |
5.9 (2.1) |
|
Gross mechanical efficiency at discharge of inpatient rehabilitation, mean: 16W |
|||||||
|
Tetraplegia |
|||||||
|
Complete |
23 |
47 |
3.3 |
3.7 |
4.6 |
5.8 |
4.4 (1.4) |
|
Incomplete |
12 |
52 |
3.0 |
3.4 |
3.9 |
5.1 |
4.0 (1.2) |
|
Paraplegia |
|||||||
|
Complete |
65 |
75 |
5.8 |
6.6 |
7.2 |
8.1 |
7.3 (3.7) |
|
Incomplete |
27 |
82 |
4.5 |
6.1 |
6.8 |
7.5 |
6.2 (1.7) |
|
Gross mechanical efficiency at 1 year after discharge of inpatient rehabilitation, mean: 15W |
|||||||
|
Tetraplegia |
|||||||
|
Complete |
10 |
27 |
3.4 |
4.0 |
4.4 |
6.4 |
3.4 (1.3) |
|
Incomplete |
6 |
38 |
3.1 |
3.9 |
5.1 |
6.8 |
4.7 (1.8) |
|
Paraplegia |
|||||||
|
Complete |
55 |
76 |
5.6 |
6.4 |
7.5 |
8.9 |
7.0 (2.1) |
|
Incomplete |
16 |
57 |
5.1 |
6.2 |
7.4 |
8.0 |
6.5 (1.8) |
|
% all part: percentage of participants who were able to perform the test from the total number of participants (within the specific lesion group) of the study; SD: standard deviation. |
|||||||
Smallest detectable difference
Table VII shows the results for the ICC, SEM and SDD of the propulsion technique variables and gross mechanical efficiency in able-bodied wheelchair users.
|
Table VII. Intraclass correlation (ICC), standard error of the measurement (SEM) and smallest detectable difference (SDD) of the propulsion technique variables and gross mechanical efficiency (ME) in able-bodied wheelchair users (n=56). The test was performed at 1.11 m/s and a resistance of 0.20 W/kg (18.4 W on average for the whole group) |
||||||||||||||
|
Variables |
Mean |
ICC |
SEM |
SDD |
SDD % |
Case |
||||||||
|
24-inch |
25-inch |
|||||||||||||
|
1 block |
2 blocks |
3 blocks |
1 block |
2 blocks |
3 blocks |
1 block |
2 blocks |
3 blocks |
Mean |
Mean |
Delta |
|||
|
Push time, s |
0.35 |
0.93 |
0.02 |
0.01 |
0.01 |
0.05 |
0.03 |
0.03 |
13.80 |
9.76 |
7.97 |
0.48 |
0.52 |
0.03 |
|
Cycle time, s |
1.20 |
0.88 |
0.12 |
0.08 |
0.07 |
0.33 |
0.23 |
0.19 |
27.32 |
19.32 |
15.78 |
1.10 |
1.24 |
0.14 |
|
Relative push time, % |
29.82 |
0.84 |
1.54 |
1.09 |
0.89 |
4.27 |
3.02 |
2.46 |
14.32 |
10.12 |
8.26 |
44.11 |
42.22 |
–1.89 |
|
Frequency, pushes/min |
53.99 |
0.91 |
3.83 |
2.71 |
2.21 |
10.63 |
7.51 |
6.13 |
19.68 |
13.92 |
11.36 |
55.12 |
49.12 |
–5.99 |
|
Contact angle, ° |
72.30 |
0.94 |
3.34 |
2.36 |
1.93 |
9.27 |
6.55 |
5.35 |
12.82 |
9.06 |
7.40 |
92.00 |
96.00 |
4.00 |
|
Fpeak, N |
71.78 |
0.87 |
5.47 |
3.87 |
3.16 |
15.17 |
10.73 |
8.76 |
21.14 |
14.95 |
12.21 |
43.69 |
43.09 |
–0.60 |
|
Fmean, N |
43.58 |
0.89 |
2.97 |
2.10 |
1.71 |
8.22 |
5.81 |
4.75 |
18.87 |
13.34 |
10.89 |
28.71 |
29.44 |
0.73 |
|
FEFmean, % |
70.08 |
0.89 |
3.62 |
2.56 |
2.09 |
10.02 |
7.09 |
5.79 |
14.30 |
10.11 |
8.26 |
47.10 |
50.03 |
2.93 |
|
FEFmax, % |
101.98 |
0.81 |
7.80 |
5.52 |
4.50 |
21.62 |
15.29 |
12.48 |
21.20 |
14.99 |
12.24 |
73.33 |
78.47 |
5.14 |
|
Slope, n/s |
69.38 |
0.83 |
7.98 |
5.64 |
4.61 |
22.12 |
15.64 |
12.77 |
31.88 |
22.54 |
18.41 |
26.91 |
27.14 |
0.22 |
|
Negative dip before push phase, n |
–2.80 |
0.72 |
0.56 |
0.40 |
0.32 |
1.55 |
1.10 |
0.90 |
–55.38 |
–39.16 |
–31.97 |
–3.15 |
–2.53 |
0.62 |
|
Negative dip after push phase, n |
–1.16 |
0.89 |
0.25 |
0.18 |
0.15 |
0.71 |
0.50 |
0.41 |
–61.15 |
–43.24 |
–35.31 |
–1.19 |
–0.36 |
0.82 |
|
Work per push, J |
11.00 |
0.92 |
1.07 |
0.76 |
0.62 |
2.97 |
2.10 |
1.71 |
27.01 |
19.10 |
15.59 |
5.92 |
6.63 |
0.71 |
|
Power output 2-sided, W |
18.40 |
0.99 |
0.49 |
0.34 |
0.28 |
1.35 |
0.96 |
0.78 |
7.35 |
5.20 |
4.24 |
10.29 |
10.34 |
0.05 |
|
Energy expenditure, W |
310.19 |
0.91 |
18.48 |
13.07 |
10.67 |
51.23 |
36.23 |
29.58 |
16.52 |
11.68 |
9.54 |
|||
|
Gross ME |
5.99 |
0.81 |
0.41 |
0.29 |
0.24 |
1.14 |
0.81 |
0.66 |
19.05 |
13.47 |
11.00 |
|||
|
Case: a 25-year-old man with a motor complete lesion at C6. Standardized 3-min propulsion test on a treadmill at 1.11 m/s with 24-inch and 25-inch wheels; Delta: difference in outcome between the 24-inch and 25-inch wheels. |
||||||||||||||



The ICC varied between 0.72 (negative dip before push phase) and 0.99 (power output 2-sided) for the propulsion technique variables and was 0.81 for the gross mechanical efficiency and 0.91 for the energy expenditure. When measuring a participant once the individual improvement in propulsion technique variables have to be 14% (push time) or even 61% (negative dip) in order to conclude that the change is greater than the measurement error.
The effects of design optimization are also shown in Table VII. Using the mean of two exercise blocks instead of one improves the SDD of, for example, the negative dip after the push phase from 0.71 (SDD% –61) to 0.50 (SDD% –43). Using the mean of 3 exercise blocks improves the SDD of the propulsion technique variable even further to 0.41 (SDD% –35).
DISCUSSION
The results of this 1-year implementation project clearly showed that there are many factors that determine the success of such a project in a positive (enabling factors) or negative (barriers) sense. As discussed earlier, the use of objective standardized measurements to quantify the results of rehabilitation is seen as an increasingly important part of good clinical practice. However, the most important factor in this project is the understanding of the test results by the clinical professionals involved. Therefore, a description of some barriers regarding the interpretation of the test outcomes, and the subsequent spin-off projects to help overcome these barriers, is given below.
Interpretation of test outcomes
For most tests and outcomes it is important to become experienced with the testing, but, even more importantly, with the meaning of the test outcomes. However, clinicians do not have much time to become familiar with the testing and interpretation of the test outcomes. In addition, they are not specifically trained on these (bio)mechanical, ergonomic and/or physiological phenomena. Although it is helpful to educate clinicians through, for example, presentations, it is also important that they are involved in testing and discussion about the outcomes under the supervision of skilled embedded human movement scientists. On the other hand, for the researchers it is difficult to draw conclusions based on individual data. Current theory is based on group-based experimental data. As such, their conclusions are normally based on modelling and statistical analyses of these group data. Having individual data and the requirement to judge relevant change, requires at least reference data and/or prediction models.
Evidence
Based on the wheelchair propulsion studies performed in the last 30 years, general (non-individualized) recommendations can be given for optimizing wheelchair propulsion with respect to physical strain and propulsion technique.
Regarding physical strain, it is important to strive for the highest mechanical efficiency or the lowest oxygen uptake and heart rate at a submaximal steady-state exercise test at the same power output and resistance. With training and learning this lower physical strain can be achieved (25), but also by changing the mechanics of the wheelchair or its ergonomic set-up and fitting (26).
Wheelchair users are able to change their propulsion technique with natural practice, i.e. just by practicing without any intervention. Fig. 4 illustrates the changes due to a learning process: at the same power output and velocity, the push frequency will diminish and subsequently the push time, cycle time, contact angle and work per push will increase (27). The power losses before and after the push (negative dips), probably caused by unskilled coupling/uncoupling of hands to the rim, will be lower after learning (27). Furthermore, mean forces and torques and the rate of force application (i.e. the slope) can diminish due to learning (27). During the early stage of motor learning, all these changes in propulsion technique variables relate to the change in mechanical efficiency, with the percentage negative work per cycle and the contact angle showing the strongest relationship (27).
Regarding wheelchair mechanics and the interface between wheelchair and user, in general it can be recommended to strive for the lowest rolling resistance (thus required power output; PO), which has an effect on both the physical strain and the propulsion technique. Table II gives an overview of the effects of different wheelchair characteristics on the rolling resistance (26). For example, a higher tyre pressure leads to a lower power output and oxygen uptake and to a longer cycle time and contact angle and subsequently lower push frequency (28). Seat height also has an effect on physical strain and propulsion technique. Physical strain seems to be optimal at 100–130º elbow angle, while increasing the seat height (smaller elbow angle) leads to lower forces in people with a spinal cord injury (29).
In summary, the recommendations of the Consortium of Spinal Cord Medicine (30) can be followed. They recommend, based on direct and indirect evidence, reducing peak forces, decreasing the rate of application of force and minimizing the frequency of propulsive strokes.
Reference data
The SWUG has described a clinical protocol for the objective assessment of manual wheelchair propulsion (13). Furthermore, they collect wheelchair propulsion data from the different institutes that use the SmartWheel with that clinical protocol. From this data pool, reference values are generated for several groups, e.g. wheelchair users with a high and low spinal cord injury. These reference values will be very helpful for interpretation of the data of an individual patient when the velocity and power output are known and constant. The data collected during our WHEEL-i protocol will also be pooled and used to calculate reference values in the future. For the wheelchair skills and gross mechanical efficiency we have developed reference values (Tables III–VI) and prediction models for the wheelchair skills (31) (available for download at www.scionn.nl), based on data from a multi-centre study in which patients with a spinal cord injury were followed during and after inpatient rehabilitation.
Synchronously viewing video
Since clinicians are not used to the biomechanical outcomes of the measurement wheel, it is helpful also to see a synchronized video of the actual test performance and, when possible, simultaneous video of the pre- and post-test performance. Specific software (MoXie Viewer, VU medical center, Amsterdam, The Netherlands), developed by Out et al. (32), for that purpose is available in Dutch gait laboratories. The MoXie Viewer allows the synchronous viewing of video and concurrently acquired signals, such as force and torque data (32) (Fig. 6). In addition, a frontal and/or sagittal view of the sitting posture of the wheelchair user, a very important aspect when choosing the optimal wheelchair configuration, can be viewed simultaneously on video and discussed. As a result of the WHEEL-i project, the MoxieViewer has been adapted and can now show the Optipush data together with video. Electromyograms (EMG) or joint angles, signals that are often analysed in gait analysis and clearly are also of relevance in optimizing wheelchair propulsion (33–35), can be added in the future.

Fig. 6. MoXie Viewer (VU medical center, Amsterdam, The Netherlands): software for synchronously viewing video and concurrently acquired signals such as force and torque data.
Smallest detectable difference
To determine whether an intervention has led to a real change in propulsion technique or physiology, it is important to determine the SDD of the different propulsion technique and physiology test outcomes. We omitted this information during the implementation of WHEEL-i. Therefore, we assembled the SDDs from already existing data for wheelchair propulsion in experienced able-bodied persons (Table VII). The SEM and SDD of many propulsion technique variables are rather large in the able-bodied group, but can be improved substantially by performing 2 or 3 exercise blocks and taking the average over the blocks. When taking the average over 3 blocks, the timing variables have to change by 7–16%, the forces by 8–12% and the gross ME by 11% to indicate a real improvement. However, the dips before and after the push have to improve by 32–35% to indicate a real improvement.
For example, we tested a 25-year-old man with a motor complete C6-lesion (height 1.91 m; body mass 81 kg) while he was propelling his own wheelchair on a treadmill with a set of 24-inch or 25-inch wheels and at a velocity of 1.11 m/s. The test outcomes for both wheel sizes are shown in the last columns of Table VII. Since we have an indication for the SDDs of the propulsion technique variables, we can conclude for this individual wheelchair user that there is an improvement, above the measurement error, in the negative dip after the push phase when using the larger wheel. Of course, we have to be careful with this interpretation, since the SEM and SDD were based on a slightly different protocol and on able-bodied participants, i.e. among others with a good arm/hand function in contrast to our patient. Therefore, a project is set up and performed in collaboration with research groups in Miami, USA and Vancouver, Canada to determine the SDDs of the same variables in wheelchair users with a spinal cord injury performing the WHEEL-i exercise protocol.
Although reference values and knowing the SDDs for the propulsion technique variables will be helpful, the interpretation of a good or bad propulsion technique, as stated in the “evidence” paragraph will be a combination of research knowledge and clinical experience. An embedded scientist, who really understands the data, signals and outcomes, together with a clinician and/or rehabilitation technician, would make the ideal combination to perform and interpret the tests. Since it is important to become familiar with the tests and outcomes, not too many testers should be appointed for this.
Future work
Introducing new measurement techniques in clinical practice automatically triggers new dialogues among researchers and clinicians. In the work groups, specific aspects of the wheelchair prescription process were discussed. There are some guidelines for wheelchair prescription (36–38) that can be followed. However, new research questions were raised by the clinicians, such as what is the effect of tyre pressure, tyre profile, wheelchair mass, rear wheel diameter, and castor wheel material, on propulsion technique and physical strain. To answer these questions, we reviewed the literature and started a research project to answer some of these issues (28).
An additional question was whether we could educate patients using the outcomes. By testing the patients multiple times and making them aware of how they propel their wheelchair, by showing them the video and test outcomes, these tests may prove helpful to educate patients. Furthermore, the Optipush and SmartWheel and their software have a feedback function. Biofeedback can be given on all test parameters while the patient is propelling the wheelchair (39). Richter et al. (39) found that biofeedback can be used to improve specific aspects of wheelchair propulsion and may be useful for clinical propulsion training. However, they also pointed out that clinicians should be aware, when training with feedback on a single variable, that other propulsion technique variables will also change.
Measurements of wheelchair propulsion technique and physical strain are not only important for patients during rehabilitation. Sport for people with a disability, including wheelchair users, is increasingly common. Monitoring the propulsion technique of (elite) wheelchair athletes and evaluating changes in their sport wheelchair and interface, such as in the “Practical guidelines for wheelchair selection in the court sports” (38), can also be performed in the wheelchair propulsion laboratory. The overall goal is performance enhancement: getting better, yet staying fit. This applies for all users, from new wheelchair users in rehabilitation to elite wheelchair athletes.
Methodological considerations
It is important to realize that using measurement wheels leads to a 3.5–4.5 kg increase in wheel mass (7–9 kg in total when using a dummy wheel on the other side with the same mass). In a spin-off project we investigated, among others, the effect of the measurement wheels on power output, propulsion technique and physical strain (28). A higher power output was found when the measurement wheels were attached compared with using regular wheels, which led to changes in physical strain and, probably, propulsion technique. Furthermore, it must be kept in mind that, for good force and torque measurements, wheelchair users have to apply force on the rim and not on the tyre. In addition, the rim coating and the distance between the rim and the tyre may differ from the user’s own wheels. However, if the test conditions between interventions are exactly the same, i.e. with the same measurement wheels, this may not be an issue in terms of pre/post comparability.
Conclusion
After describing and implementing the WHEEL-i test protocol, the largest barrier for systematic monitoring of the individual wheelchair fitting and learning process in rehabilitation with, among others, instrumented measurement wheels was interpretation of the outcomes by professionals. Good interpretation of the outcomes is vital and requires an embedded scientist in rehabilitation who continuously collaborates with science. Other important facilitators are the availability of reference data, knowledge of the smallest detectable difference, and visualization of the outcomes.
ACKNOWLEDGEMENTS
Funding. Zon-Mw Innovation Program Rehabilitation, grant number 335020016.
The authors declare no conflicts of interest.
References
