Jesper Knoop, MSc, PT1, Marike van der Leeden, PT, PhD1,2, Leo D. Roorda, PhD, MD, PT1, Carina A. Thorstensson, PT, PhD3, Martin van der Esch, PT, PhD1, Wilfred F. Peter, PT1, Mariette de Rooij, PT1, Willem F. Lems, PhD, MD4,5, Joost Dekker, PhD2,6 and Martijn P. M. Steultjens, PhD7
From the 1Amsterdam Rehabilitation Research Center, Reade, 2Department of Rehabilitation Medicine/EMGO-institute, VU University Medical Center, Amsterdam, The Netherlands, 3Department of Clinical Neuroscience and Rehabilitation, Institute of Neuroscience and Physiology, University of Gothenburg, Gothenburg, Sweden, 4Jan van Breemen Research Institute, Reade, Departments of 5Rheumatology and 6Psychiatry, VU University Medical Center, Amsterdam, The Netherlands and 7School of Health and Life Sciences, Institute for Applied Health Research, Glasgow Caledonian University, Glasgow, UK
OBJECTIVE: To test whether knee stabilization therapy, prior to strength/functional training, may have added value in reducing activity limitations only in patients with knee osteoarthritis who have knee instability and (i) low upper leg muscle strength, (ii) impaired knee proprioception, (iii) high knee laxity, or (iv) frequent episodes of knee instability.
DESIGN: Subgroup analyses in a randomized controlled trial comparing 2 exercise programmes (with/without knee stabilization therapy) (STABILITY; NTR1475).
Patients: Participants from the STABILITY-trial with clinical knee osteoarthritis and knee instability (n = 159).
METHODS: Effect modification by upper leg muscle strength, knee proprioception, knee laxity, and patient-reported knee instability were determined using the interaction terms “treatment group*subgroup factor”, with the outcome measures WOMAC physical function (primary), numeric rating scale pain and the Get up and Go test (secondary).
RESULTS: Effect modification by muscle strength was found for the primary outcome (p = 0.01), indicating that patients with greater muscle strength tend to benefit more from the experimental programme with additional knee stabilization training, while patients with lower muscle strength benefit more from the control programme.
CONCLUSION: Knee stabilization therapy may have added value in patients with instability and strong muscles. Thus it may be beneficial if exercises target muscle strength prior to knee stabilization.
Key words: knee osteoarthritis; exercise therapy; knee stability; muscle strength; laxity; proprioception; subgroup analysis.
J Rehabil Med 2014; 46: 703–707
Correspondence address: Jesper Knoop, Amsterdam Rehabilitation Research Center, Reade, NL-1056AB Amsterdam, The Netherlands. E-mail: j.knoop@reade.nl
Accepted Jan 21, 2014; Epub ahead of print Jun 4, 2014
Introduction
The majority (> 60%) of patients with knee osteoarthritis (OA) report knee instability (i.e. buckling, shifting or giving way) (1, 2), which is associated with pain and activity limitations (1–3). The knee joint is stabilized by a combination of active neuromuscular control, provided by muscles and proprioceptive stimuli, and by passive restraint, provided by the ligaments and capsule (4).
In an earlier randomized controlled trial (STABILITY) (5), we tested the hypothesis that patients with knee OA who have knee joint instability benefit more from a tailored exercise programme that focuses initially on knee stability, and subsequently on muscle strength and performance of daily activities, compared with a control programme that focuses only on muscle strength and performance of daily activities. Unexpectedly, the two programmes were found to be similarly effective in reducing activity limitations (~30% improvement), pain (~40%) and knee instability (~30%). It is possible that initial knee stabilization therapy may be effective only in patients in whom knee instability is most severe (i.e. those with lowest muscle strength, worst proprioception, highest laxity, or most frequent episodes of instability).
The aim of the study was therefore to test whether knee stabilization therapy, prior to strength/functional training, has added value in reducing activity limitations in patients with knee OA who have knee instability and (i) low upper leg muscle strength, (ii) impaired knee joint proprioception, (iii) high knee joint laxity, or (iv) frequent episodes of knee instability.
Material AND Methods
Methods
Design. A single-blind, randomized controlled trial (STABILITY; Dutch Trial Registry NTR1475) (5) to compare two exercise programmes was conducted previously in an outpatient rehabilitation centre (Reade, The Netherlands). Participants were measured at baseline and at 6-week (i.e. mid-treatment), 12-week (i.e. directly post-treatment) and 38-week follow-up (FU) (i.e. 6 months post-treatment), by a trained research assistant blinded for group allocation. This study was approved by the medical ethics review board (Reade/Slotervaart Hospital). For the present study, pre-planned subgroup analyses were performed.
Participants. Inclusion criteria were: (i) diagnosis of knee OA according to the clinical American College of Rheumatology (ACR) criteria, (ii) age between 40 and 75 years, and (iii) presence of self-reported knee instability in the past 3 months and/or biomechanically assessed knee instability (using cut-off points for upper leg muscle weakness, and proprioceptive accuracy and varus-valgus laxity of the knee joint (5)). Exclusion criteria for the trial have been described in our previous publication (5). All participants provided written informed consent.
Experimental and control intervention
The interventions have been described in detail previously (5). In summary, both the experimental and control intervention comprised a supervised exercise programme of 12 weeks, with two 60-min sessions per week, in groups of approximately 8 participants. In addition, home exercises were provided for 5 days per week (on non-treatment days only). Each group was supervised by two physical therapists, who were specifically trained to supervise only one of both treatments. Training intensity, which gradually increased during the programme, and amount of attention from the physical therapists were similar in both groups (5).
The experimental programme consisted of 3 phases: (i) week 1–4, focusing on knee stabilization, (ii) week 5–8, focusing on muscle strengthening, in addition to knee stabilization, and (iii) week 9–12, focusing on performance of daily activities, in addition to muscle strengthening and knee stabilization. During the entire programme, but explicitly in the first 4 weeks, patients in the experimental group received instructions during exercising to focus on their knee position (i.e. proprioception) and to control this position (i.e. neuromuscular control). For this purpose, verbal and tactile feedback from physical therapists and visual feedback from mirrors were provided. Furthermore, patients received specific exercises challenging them to maintain adequate knee position.
The control programme consisted of only two phases: (i) week 1–8, focusing on muscle strengthening, and (ii) week 9–12, focusing on performance of daily activities, in addition to muscle strengthening. Physical therapists in the control group were not allowed to give instructions and feedback on knee position.
Outcome measures
Primary outcome. Self-reported activity limitations were assessed by the Dutch translation of the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) subscale physical function, with a total score ranging from 0 (no limitations) to 68 (maximally limited) (6, 7).
Secondary outcomes. Self-reported knee pain severity was assessed on a numeric rating scale (NRS), ranging from 0 (no pain) to 10 (worst imaginable pain), by the question “What was your average knee pain during the last week?” (8). The Get Up and Go (GUG) test was used as a measure for observed activity limitations. The GUG test is a performance-based test in which a patient is asked to rise from a chair and walk as fast as possible over a distance of 15 m (9).
Subgroup factors
Baseline values of upper leg muscle strength, proprioceptive accuracy of the knee joint, varus-valgus knee joint laxity and patient-reported knee instability were used as subgroup factors.
Upper leg muscle strength. Muscle strength was assessed for knee flexion and extension using an isokinetic dynamometer (EnKnee, Enraf-Nonius, Rotterdam, The Netherlands). Patients performed 3 maximal test repetitions, which were averaged per leg and then divided by patient’s weight. This normalized measure (in Nm/kg) was used for the analyses (10). Excellent intra-rater reliability (intraclass correlation coefficient [ICC] 0.93) has been reported in knee OA patients (11).
Proprioceptive accuracy. Proprioceptive accuracy (motion sense) was assessed using a knee joint motion detection task (with motion at 0.3°/s in the extension direction). The mean of 3 measurements was calculated for each knee (10). Intra- and inter-rater reliability (ICC) in knee OA patients is 0.88 and 0.91, respectively (12).
Varus-valgus laxity. Laxity was operationalized as the total amount of passive movement in the frontal plane after fixed varus and valgus load of 7.7 Nm. The mean of 3 measurements was calculated for each knee (10). Intra- and inter-rater reliability (ICC) in healthy persons is 0.80 and 0.88, respectively (13).
Patient-reported instability. The number of episodes of buckling, shifting, or giving way of the knee in the past 6 weeks was assessed on an ordinal scale (i.e. “none”, “seldom” [1–2 episodes], “regularly” [3–5], and “very often” [> 5]), as part of a questionnaire (10) based on literature (1, 3). This scale was dichotomized as follows: none/seldom vs regularly/very often.
Other measures
In addition, multiple other variables were measured at baseline, including demographics (e.g. sex, age, body mass index (BMI)), radiographic knee OA severity [Kellgren/Lawrence grade], knee joint alignment as measured by goniometer in standing position) (5).
Statistical analysis
Data were analysed using PASW Statistics 18.0 (SPSS Inc., Chicago, IL, USA). Generalized estimating equation (GEE) analyses, based on intention-to-treat (ITT) approach, were performed to compare the effectiveness of experimental with control intervention over the 38-week study period (14). Effect modification by each of the subgroup factors was estimated by including treatment group (0 = control; 1 = experimental), the subgroup factor, and an interaction term of “treatment group × subgroup factor” into the GEE model, where a significant interaction term indicates effect modification (15). Outcome measures were WOMAC physical function (primary), NRS pain, and the GUG test (secondary). We adjusted for the outcome measure at baseline, relevant baseline characteristics that were different between treatment groups (i.e. proprioceptive accuracy, instability affecting daily functioning [yes/no], and varus malalignment [yes/no] [5]), as well as for demographics (i.e. age, gender, BMI, and radiographic knee OA severity). Unstandardized regression coefficients (B) with adjunctive 95% confidence intervals (CI) and p-values were estimated. Statistical significance was accepted at p-values < 0.05.
Results
Descriptives of the study sample (n = 159) are shown in Table I. During the study period, 5 participants (1 from the experimental group and 4 from the control group) were lost to follow-up before the first follow-up measurement and therefore could not be analysed. In addition, 2 participants discontinued the intervention (both from experimental group) and 4 underwent knee surgery after treatment (2 from each group). Participants attended a mean of 21 out of 24 sessions and performed home exercises for a mean of 4 days a week, similarly in the 2 treatment groups. As reported previously (5), no overall difference in effectiveness between experimental and control intervention could be demonstrated.
|
Table I. Baseline characteristics of experimental and control group |
|||||
|
Experimental group (n = 80) |
Control group (n = 79) |
||||
|
Mean (SD) |
n (%) |
Mean (SD) |
n (%) |
||
|
Demographics |
|||||
|
Age, years |
62.1 (7.6) |
61.8 (6.6) |
|||
|
Gender, female |
53 (66) |
44 (56) |
|||
|
BMI, kg/m2 |
28.8 (4.8) |
28.3 (4.5) |
|||
|
Radiographic severity of kneea, K/L grade ≥ 2 |
59 (61) |
54 (68) |
|||
|
Outcome measures WOMAC (physical function, 0–68) |
25.2 (11.8) |
27.1 (12.7) |
|||
|
NRS (knee pain severity, 0–10) |
4.8 (2.2) |
5.2 (2.0) |
|||
|
Get Up and Go test, s |
10.6 (1.8) |
10.8 (2.5) |
|||
|
Subgroup factors |
|||||
|
Upper leg muscle strength, Nm/kga |
0.83 (0.35) |
0.85 (0.43) |
|||
|
Proprioceptive accuracy of knee, °a |
2.7 (2.2) |
3.7 (2.6) |
|||
|
Varus-valgus laxity of knee, °a |
7.0 (3.1) |
7.1 (4.5) |
|||
|
Patient-reported knee instability in previous 6 weeks, yes |
24 (30) |
24 (30) |
|||
|
aData from index knee. SD: standard deviation; BMI: body mass index; K/L: Kellgren/Lawrence; WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index; NRS: numeric rating scale. |
|||||
For the primary outcome WOMAC physical function, a significant interaction term of “treatment group*upper leg muscle strength” (p = 0.01) was found (Table II). This indicates that, in persons with higher muscle strength at baseline, the experimental intervention may be more effective than the control intervention (Fig. 1a, right-hand side), while the control intervention may be more effective in persons with lower muscle strength (Fig. 1a, left-hand side).
|
Table II. Interaction terms of treatment group (experimental vs control) |
||||||||
|
Primary outcome |
Secondary outcomes |
|||||||
|
WOMAC, physical functiona |
NRS, paina |
GUG-testa |
||||||
|
B (95% CI) |
p-value |
B (95% CI) |
p-value |
B (95% CI) |
p-value |
|||
|
Interaction of treatment group with |
||||||||
|
Baseline upper leg muscle strength |
–7.07 (–12.39 to –1.75) |
0.01 |
–0.67 (–1.82 to 0.49) |
0.26 |
–0.04 (–0.70 to 0.62) |
0.90 |
||
|
Baseline knee joint proprioception |
–0.25 (–1.35 to 0.86) |
0.66 |
–0.03 (–0.23 to 0.16) |
0.74 |
–0.08 (–0.21 to 0.06) |
0.25 |
||
|
Baseline varus-valgus knee joint laxity |
0.66 (–0.09 to 1.40) |
0.09 |
0.18 (0.07 to 0.29) |
< 0.001 |
0.00 (–0.08 to 0.08) |
0.97 |
||
|
Baseline patient-reported knee instability |
0.73 (–5.76 to 7.22) |
0.83 |
–0.95 (–1.92 to 0.01) |
0.05 |
–0.58 (–1.13 to –0.02) |
0.04 |
||
|
Subgroup factor in association with outcome measure (n = 154). aAdjusted for relevant baseline characteristics that were different between groups (i.e. proprioceptive accuracy, instability affecting daily functioning, and varus malalignment) in addition to demographics (i.e. age, gender, body mass index, radiographic severity of knee OA) and baseline score of outcome measure. ITT: intention-to-treat; WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index; NRS: numeric rating scale; GUG: Get up and Go: CI: confidential interval. |
||||||||
For the secondary outcome measures only, we found significant interactions with laxity (p < 0.001 for pain) and patient-reported knee instability (p = 0.05 for pain and 0.04 for the GUG test). These interactions suggest that the experimental intervention may be more effective than the control intervention in those persons with lower laxity (Fig. 1b, right-hand side) or more frequent knee instability (Fig. 1c, left-hand side). Per-protocol analyses excluding protocol violators yielded similar results. Furthermore, similar results were yielded in analyses of data from the 12-week treatment period only.
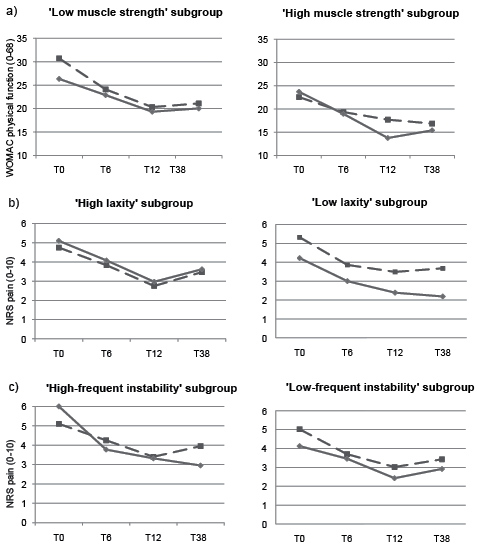
Fig. 1. Outcomes of control (- - -) and experimental (–––) groups during study period, stratified for subgroups based on baseline value of: (a) upper leg muscle strength, (b) knee joint laxity, and (c) number of patient-reported episodes of knee instability, with higher scores meaning more severe activity limitations/pain. Subgroups were formed using gender-specific medians for upper leg muscle strength and knee joint laxity, or a cut-off of 3 episodes for knee instability.
Discussion
The main finding of this study is that initial knee stabilization training may have added value over standard exercises (i.e. strength/functional training) in patients with strong muscles, but not in those with weak muscles. This was based on a significant interaction between treatment group and baseline upper leg muscle strength for the primary outcome WOMAC physical function. Stratified analyses showed that in the “high muscle strength subgroup”, the experimental programme was a mean of 2.0 points more effective, whereas in the “low muscle strength subgroup”, the control programme was a mean of 2.8 points more effective. This total difference of 4.8 points, which is 18% of the mean baseline WOMAC score, can be considered a clinically important difference (16). Therefore, adequately allocating patients over the exercise groups based on baseline muscle strength could optimize treatment outcome. Although this main finding is in contrast to our hypothesis, it confirms our explanation for the negative finding from our trial (5), as well as from others (17, 18). We proposed that muscle strengthening exercises are highly effective for the majority of patients with knee OA who have knee instability, without necessarily adding specific knee stabilization training. The present subgroup analysis further indicates that, in patients with knee instability, and especially those with weak muscles, exercises should focus on muscle strengthening, whereas in patients with knee instability and (already) strong muscles, initial knee stabilization training can be beneficial. Thus, for optimal treatment effects, strength training may need to be provided first, prior to knee stabilization training.
Secondly, knee stabilization training may also have added value over strength/functional training in patients with knee instability, who have adequate passive restraint (i.e. minimal laxity). This conclusion is based on the significant interaction between treatment group and laxity for pain. It is possible that, in patients with high laxity, interventions such as knee bracing (19) to support the passive restraint system may need to be added to enable them to benefit from knee stabilization training.
Finally, we found significant interactions between treatment group and patient-reported knee instability for pain and the GUG test. This result confirmed our hypothesis that initial knee stabilization training has added value over strength/functional training in patients reporting more frequent episodes of knee instability. This effect seems to apply mainly to the first half of the exercise programme (Fig. 1c, left-hand side), which is the period in which the experimental group received knee stabilization training most extensively. For patients reporting knee instability only occasionally, standard exercises seem to be sufficient.
We need to emphasize that our findings should be interpreted with caution, as our study was not powered to perform subgroup analyses. On the other hand, the subgroup analyses were pre-planned and executed by using the interaction term method, which carries a much smaller risk of false-positive results compared with stratified analyses (15). Furthermore, we used only a minimal number of subgroup factors, as recommended (15).
In conclusion, initial knee stabilization therapy may have added value in patients with knee instability and strong muscles. Thus, it may be beneficial if exercises target muscle strength prior to knee stabilization. In addition, knee stabilization therapy may have added value in patients with knee instability and minimal laxity, or in those reporting more frequent episodes of knee instability.
Acknowledgements
The authors gratefully acknowledge Dr Gerritsen and Dr Voorneman for examining patients, S. Romviel for assessing all patients, and all physical therapists for professionally supervising treatment groups.
The study was funded by the Dutch Arthritis Association, which had no role in project implementation, analysis, interpretation, or manuscript writing.
REFERENCES
