Lucia Ramsey, BSc (Hons), OT, Robert John Winder, PhD and Joseph G. McVeigh, PhD
From the Centre for Health and Rehabilitation Technologies, University of Ulster, Ulster, Northern Ireland
OBJECTIVE: To evaluate the effectiveness of working wrist splints in people with rheumatoid arthritis.
Data sources and study selection: This review adhered to the Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines. Ten databases were searched from inception until September 2012 for quantitative and qualitative studies on the effectiveness of working wrist splints in rheumatoid arthritis.
DATA EXTRACTION: Data was extracted on participants, interventions, outcome measures and results. Experimental studies were evaluated using the van Tulder scale and the Cochrane Risk of Bias tool. Data was extracted by a single reviewer and all studies were reviewed by two blind reviewers.
DATA SYNTHESIS: Twenty-three studies were included in the review (n = 1,492), 13 experimental studies including 9 randomized controlled trials (RCTs) and 2 qualitative studies. Data was summarized using best evidence synthesis and a meta-ethnographical approach guided qualitative evidence synthesis. There is strong quantitative evidence (including 9 RCTs), supported by conclusions from qualitative literature, that working wrist splints reduce pain (d = 0.7–0.8), moderate evidence that grip strength is improved (d = 0.3–0.4) and dexterity impaired and insufficient evidence of their effect on function.
CONCLUSIONS: Working wrist splints reduce pain and improve grip in rheumatoid arthritis. The effect of splints on function is not yet clear.
Key words: working wrist splint; rheumatoid arthritis; mixed methods systematic review.
J Rehabil Med 2014; 46: 00–00
Correspondence address: Lucia Ramsey, Centre for Health and Rehabilitation Technologies (CHaRT), School of Health Sciences, University of Ulster, Shore Road BT370QB UK. E-mail: l.ramsey@ulster.ac.uk
Accepted Jan 16, 2014; Epub ahead of print Apr 8, 2014
INTRODUCTION
Rheumatoid arthritis (RA) is a chronic, systemic, inflammatory disease (1) affecting 400,000 people in the UK (2). Early intervention is emphasized in RA in order to maintain function, inhibit joint damage and improve patients’ quality of life. National Institute for Health and Clinical Excellence (NICE) guidelines (1) recommend a combination of pharmacological and non-pharmacological therapy (3).
Sixty percent of patients with RA have hand and wrist problems (1) that could benefit from occupational therapy (OT) and these patients are routinely referred for splinting (4, 5, 6). Several terms are used to describe wrist splints which are thought to support the wrist, restrict movement and thereby reduce pain and allow for greater functional use of the hand. For the purpose of this review the term working wrist splint will be used to define splints which support the wrist and allow for functional use of the hand. Treatment guidelines (1, 7, 8) recommend that working wrist splints should be offered to patients with RA, however, they also highlight the lack of rigorous analysis of their effectiveness. Only one Cochrane review (9), one systematic review (10) and two narrative reviews (5, 11) have exclusively examined the evidence for splinting in patients with RA.
Egan et al. (9) examined the use of splints and orthosis in the treatment of RA and included 14 studies of which 8 were randomized controlled trials (RCTs). Five studies examined working wrist splints, and Egan et al. (9) concluded that they have no positive effect on pain. However, this review included a wide range of splint types, and overall the quality of studies was rated as ‘fair’. Steultjens et al. (12) explored the evidence for a range of OT interventions used in treating patients with RA, 16 studies, including 7 RCTs, focused on a range of upper limb splints. The authors concluded that there were indicative findings that splints decrease pain, however, they rated the overall methodological quality of the studies as poor.
Previous literature reviews have not examined the full breadth of literature, most have been unsystematic in their approach and frequently have failed to adequately report results or present conflicting interpretation of the same studies. Consequently there is no clear guidance for clinicians on the effectiveness and use of working wrist splints in RA.
When attempting to answer questions of effectiveness, the statistical combination of reported data, as is common in systematic reviews, could be criticized as lacking context and explanation (13). Similarly, qualitative studies can only provide insight to develop an understanding of lived experiences. Theories generated from these insights however, can be examined for evidence of their effect in the quantitative literature and a deeper understanding of the impact of splinting can be gained through a combined synthesis of the breadth of literature available. By including evidence from diverse study types this review aimed to provide a much richer and more meaningful answer (13) to the question: Are working wrist splints effective in the management of patients with RA? Effectiveness is defined as improvement in function, strength, pain and dexterity for the purpose of this review.
METHODS
Data sources and searches
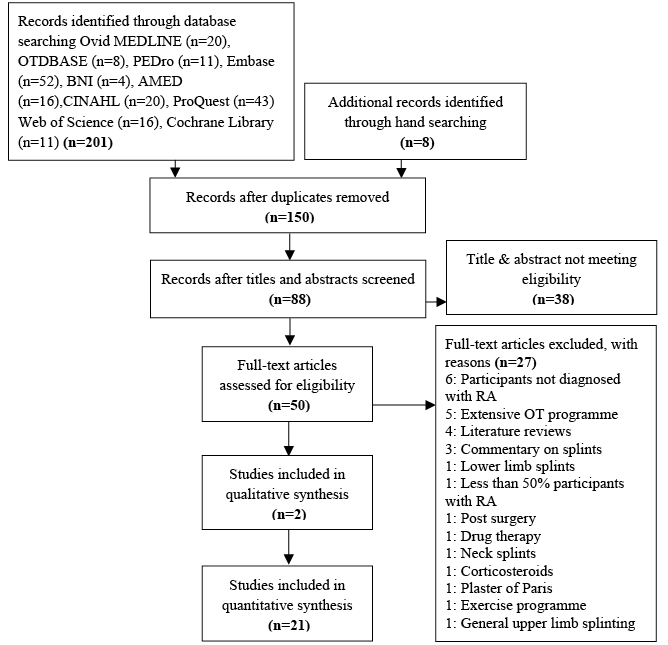
The protocol for this study was registered with the Centre for Review and Dissemination (CRD42012001946) and the review was conducted according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (14) (PRISMA) guidelines. A systematic electronic literature search was conducted using 10 databases (Fig. 1) from their date of inception to September 2012. Key-words used to search were dependent on the database (see Fig. 2 for an example of the Embase search). Article references were hand searched and a search of relevant print and electronic journals was also conducted. Titles and abstracts of potentially eligible studies were screened by one researcher (LR) and ambiguous studies were discussed with two additional researchers (JMcV and RJW) and consensus reached.
|
Database: EMBASE search strategy 1980–2012 week 39: |
|
1 orthopedic equipment/ or brace/ or splint/ (16852) 2 orthos$.mp. (37922) 3 orthot$.mp. (23413) 4 exp orthotics/ (2548) 5 support.mp. (567390) 6 exp brace/ (5027) 7 strap.mp. (1011) 8 exp immobilization/ (40475) 9 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 (677801) 10 exp rheumatoid arthritis/ (109454) 11 exp ARTHRITIS/ or exp CHRONIC ARTHRITIS/ (250935) 12 systemic arthritis.mp. (86) 13 RA.mp. (46042) 14 10 or 11 or 12 or 13 (271362) 15 HAND MOVEMENT/ or HAND/ or HAND STRENGTH/ or HAND FUNCTION/ or HAND MUSCLE/ or HAND GRIP/ (35213) 16 WRIST/ or WRIST DISEASE/ (13130) 17 arm/ (26046) 18 upper extremity.mp. (11573) 19 upper limb.mp. (9928) 20 wrist joint.mp. (1055) 21 exp CARPAL JOINT/ or exp CARPAL BONE/ (5361) 22 15 or 16 or 17 or 18 or 19 or 20 or 21 (87706) 23 9 and 14 and 22 (355) 24 from 23 keep 30,34,83,85,88,97,114-115,120,123,128-129,136-137,143,157-158,188,212,218-219,221,223,226,230,232,235,237,240,242,246,253,257,277,281-283,285,290,292-293,303,308,310,334,340,342,350-353,355 (52) *************************** |
Fig. 2. Embase keyword search strategy.
Study selection
Qualitative and quantitative studies published in English that examined the effectiveness of working wrist splints amongst people with RA or the experiences and/or perceptions of patients and/or therapists or carers involved in the provision of working wrist splints to people with RA were included. Studies where less than 50% of participants were diagnosed with RA and studies including children with juvenile idiopathic RA were excluded. Studies where splinting was included as part of an extensive OT treatment program were excluded as the effect of co-interventions could increase threats to internal validity. Studies where splints were used following surgery were also excluded as the primary purpose of splinting following surgery is to immobilize and facilitate healing. Studies addressing splints for the finger or thumb joints only or studies investigating pressure gloves were also excluded as these are not wrist splints. Outcomes of interest were identified as: pain, swelling, deformity, range of motion, dexterity, strength, function and quality of life with the most frequently occurring outcomes: function, strength, pain and dexterity being presented here.
Data extraction
The primary reviewer (LR) extracted data guided by the Cochrane Effective Practice and Organisation of Care Group data abstraction form (15).
Quality assessment and risk of bias
Each paper relevant for risk of bias assessment was independently assessed by two reviewers. A blinded rating of the methodological quality of the studies was carried out by the primary reviewer and then independently reviewed by a second reviewer (JMcV or JW). Any ambiguous issues were discussed and consensus reached. RCTs were analysed for methodological quality using the van Tulder Scale and risk of bias was assessed using the Cochrane Risk of Bias tool (16). Consensus was reached by discussion and the level of inter-rater agreement recorded as a Kappa coefficient.
RCTs were deemed to be of high quality if they scored at least 6/12 on the van Tulder Scale (1) and evidenced two of the following 4 criteria: 1. Inadequate randomization 2. Non-blinding of assessors 3. No intention to treat analysis 4. No measurement of compliance. Medium quality studies were classified as achieving at least 6/12 on the van Tulder Scale and satisfying at least one of the 4 criteria above. Studies were deemed to be of low methodological quality if they scored less than 6/12 on the van Tulder Scale and/or satisfied one or fewer of the 4 listed risks to bias. Quality classifications were then combined with the criteria in Table I to summarize the strength of evidence for each outcome. Clinical relevance of RCTs was summarized using Guidelines from the Cochrane Collaboration Back Review Group (16) modified by Dorrestijin et al. (19) (Table I) and tailored to reflect items deemed applicable for trials involving splinting.
|
Table I. Best evidence synthesis guidelines |
|
|
Strong evidence |
Provided by consistenta statistically significant findings in outcome measures in at least two high quality RCTsb |
|
Moderate evidence |
Provided by statistically significant findings in outcome measures in at least one high quality RCTb OR Provided by consistenta, statistically significant findings in outcome measures in at least two medium quality RCTsb |
|
Limited evidence |
Provided by statistically significant findings in at least one medium quality RCTb OR Provided by consistenta, statistically significant findings in outcome measures in at least two low quality RCTsb |
|
No or insufficient evidence |
If results of eligible studies do not meet the criteria for one of the levels of evidence listed above (e.g. no statistically significant findings) OR In case of conflicting (statistically significant positive and statistically significant negative) results among RCTs OR In case of no eligible studies |
|
aFindings are considered consistent if they point in the same direction. bIf the number of studies showing evidence is lower than 50% of the total number of studies found within the same category of methodological quality, ‘no evidence’ is stated. RCT: randomised controlled trial. Dorrestijn O, Stevens M, Winter J, van der Meer K, Diercks R. Conservative or surgical management for subacromial impingement syndrome? A systematic review. J Shoulder Elb Surg 2009; 18: 652–660. |
|
For studies of quasi-experimental and observational design (other design), methodological quality was assessed using the Cochrane Criteria of Methodological Quality (12). Methodological quality was judged as high if at least 4 internal validity measures, two descriptive and one statistical criterion scored affirmatively (12). Survey/questionnaire studies were assessed using the tool recommended by the Centre for Evidence Based Management (17). For qualitative studies an analysis of the research process and transparency in data analysis was guided by the Critical Appraisal Skills Programme (CASP) © Qualitative Critical Appraisal Tool (18).
Consequently, threats to bias were: inadequate randomization, non-blinding of assessors, no intention to treat analysis and no measurement of compliance. Medium quality studies were classified as achieving at least 6/12 on the van Tulder Scale and satisfying at least one of the 4 criteria above. Studies were deemed to be of low methodological quality if they scored less than 6/12 on the van Tulder Scale and/or satisfied one or fewer of the 4 listed risks to bias. Quality classifications were then combined with the criteria in Table I to summarize the strength of evidence for each outcome.
Data synthesis and analysis
Due to the heterogeneity of the studies in terms of settings, splint interventions and outcome measures it was not possible to carry out a meta-analysis. As recommended by the Centre for Reviews and Dissemination (20), a narrative approach to the synthesis of data from the quantitative studies was undertaken. A summary of the characteristics and findings of the included studies was tabulated (Table SI1) and analysis of the relationships within and between studies was combined with overall assessment of the robustness of evidence (20). Where appropriate and possible, the magnitude of the change between groups was measured using Cohen’s d (effect size) where d = 0.2 was considered a small effect size, d = 0.5 medium and d = 0.8 large effect size.
A meta-ethnographical approach involving the selection, comparison and analysis of studies was used to synthesize qualitative evidence (21). Quantitative and qualitative syntheses were then combined to compare and contrast the interventions evaluated in the quantitative studies with the qualitative data.
RESULTS
The database and hand search resulted in 150 titles which were reduced to 88 by application of the inclusion and exclusion criteria for eligibility screening. Following screening 23 studies (1981–2009), involving 1,492 participants were eligible for inclusion (Fig. 1).
Description of studies
Studies were classified as RCTs (n = 9) (22–30), experimental (n = 4) (31–34), observational (n = 3) (35–37), survey/questionnaires (n = 5) (38–42) and qualitative studies (20) (n = 2) (43, 44). Seventeen studies presented descriptive statistics relating to the age of the participants with a mean age of 55.5 years from 16 of these. One study (26) provided the median age, and 4 (36–39), did not state the age of the participants. Two studies did not specify participants’ gender (36, 39) and the gender of the rheumatologists surveyed in the study by Spoorenberg et al. (42) was not stated. From 12 studies (22, 23, 27, 28, 30–35, 40, 42) mean disease duration was 9.3 years, median was given for one study (26) as 3 years and in 6 not stated (25–27, 32, 39, 43).
The most frequently investigated outcomes throughout all studies were hand function or perception of hand function (n = 9 studies) (22, 23, 25–28, 20, 31, 34), grip or pinch strength (n = 9 studies) (23, 24, 25, 29–33), pain (n = 8 studies) (25–30, 33, 34), dexterity (n = 4 studies) (32, 34, 35, 37).
Five cohort surveys investigated: splint compliance (41), factors affecting patient compliance (38) and usage of wrist splints (40, 41, 42). Two qualitative studies using phenomenological methodology investigated the use and preference of wrist splints (44) and the determinants of the use of wrist splints (43).
With respect to outcome measures a total of 31 outcome measures were used to measure function, grip strength, pain, dexterity, ROM and disease activity. Follow up time varied across studies from immediate checking effects of the splint (24) to checking effects one year following use (39). In cross-over trials splint use was measured after one, two or four weeks use with a one week wash out between splints (22, 25, 28, 29, 34). Table II presents a summary of the splinting parameters showing inconsistency in the duration and frequency of splint wearing regimes.
|
Table II. Frequency and duration of splint use |
|
|
Frequency and duration (reference) |
(Reference) splint type(s) studied |
|
Frequency of splint wear (How often) Tested at Immediate wear (29, 33, 34, 36, 40) Daily (24, 28, 37, 38, 43) At least 4 h/day (22, 23, 44) As much as possible, day and night (42) As much as possible day only (31) At own discretion (32, 39) While performing everyday activities in accordance with therapists advice (26, 27) While resting (27) Not stated (25, 33, 35) |
(22, 23, 44) Smith & Nephew, Roylan® D-ring & Kendall-Future #33 pre-fabricated wrist splints (37, 38) Lightcast fibreglass splint (24) Rehband™ elastic wrist orthosis (25) Futuro™ and Spenser wrist splints (26) Custom made thermosplastic and custom made two-way stretch elastic fabric splints (27) Futuro™ cock-up splint, Orhoplast/Plaster of Paris wrist immobilisation splint (28) Roylan® wrist splint, Custom made leather splint, Anatomical technologies ©elastic wrist splint (29) Futuro™, Roylan®-D, Medical specialties wrist splints (30) Futuro™ splint (31) Roylan® D-ring, GM005H, GM008 or GM009 (GM Medical bracing) wrist splints (32) Custom made polyethylene gauntlet wrist splint (33) Liberty™ D ring, Dynamic hinged wrist resist, Dynamic spiral custom made (34) Camp soft volar wrist splint, Rehband ™ soft volar wrist splint (35) Futuro™ Kendall #33 (36) Leather carpometacrpal band, Transverse arch felt pad (39) Functional wrist splint (40) Dorsal sans splint XR, Palmar sans splint pink, Gauntlet plastazote®, pre-fabricated cotton elastic wrist splint (41) Leather gauntlet, elastic commercial gauntlet, custom made dorsal thermoplastic, Custom made volar thermoplastic (42) Synthetic thermolyn® wrist orthosis, Futuro ™ wrist splint (43) Pre-fabricated fabric working wrist splint |
|
Duration of each splint wearing period (For how long each time) For outcome measurement only (29, 33, 34, 36, 40) During pain or discomfort inducing activities (24, 28) Intermittent use (22, 23, 44) At least 2 h a day (31) Average of between 3–6 h with 1 subject wearing all night (32) On a daily basis (35) Range from 24h/day to never (25–27, 37–39, 43) Not stated (30, 42) |
|
|
Duration of overall splinting period (How long overall) For outcome measurement only (33, 34, 36, 40) 6 months (24, 28) 12 weeks (22, 23, 39, 44) 5 weeks (30, 42) 4 weeks (27, 31) 4 months (32) 1 week (35) Approximately 9 months (37) 12 months (40) Between 1 and 12 months (43) Not stated/insufficient detail (29a, 25, 38) |
|
|
aGiven a splint anything up to 24 months earlier, measurement with and without splint. |
|
Risk of bias assessment within studies
Results of the Cochrane Risk of Bias tool and the van Tulder Scale for the included RCTs are shown in Tables III and IV. The mean score for the van Tulder Scale was 5.6/12 (range 4–7, moderate quality (45). Using the Cochrane Risk of Bias tool 5 studies obtained a score of 6 or more, indicating a low risk of bias (22, 25, 27, 28, 30). Four studies scored less than 6, indicating substantial bias (23, 24, 26, 29).
|
Table III. Cochrane Risk of Bias for randomised controlled trials |
||||||
|
Authors, year (ref) |
Random Sequence generation |
Concealed allocation |
Blinding of key personnel |
Incomplete outcome data addressed |
Free of selective outcome reporting |
Free of other bias |
|
Anderson & Maas, 1987 (24) |
Yes |
Unclear |
No |
No |
No |
No |
|
Haskett et al., 2004 (25) |
Yes |
No |
No |
Yes |
Yes |
Yes |
|
Kjeken et al., 1995 (26) |
Yes |
Unclear |
No |
Yes |
Unclear |
Yes |
|
Pagnotta et al., 2005 (27) |
Yes |
Unclear |
No |
Yes |
Unclear |
No |
|
Stern et al., 1996 (22) |
Yes |
Unclear |
No |
No |
No |
Yes |
|
Stern et al., 1996 (23) |
Yes |
Unclear |
No |
Yes |
No |
Yes |
|
Thiele et al., 2009 (28) |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
|
Tijhuis et al., 1998 (29) |
Yes |
Unclear |
Yes |
Yes |
Yes |
Yes |
|
Veehof et al., 2008 (30) |
Yes |
Yes |
No |
Yes |
Yes |
Yes |
|
Table IV. The van Tulder Scale for randomised controlled trials |
|||||||||||||
|
Authors, year (ref) |
1 Adequate randomisation |
2 Concealed allocation |
3 Patient blinded |
4 Therapist blinded |
5 Assessor blinded |
6 Drop out accounted |
7 ITT |
8 Free of selective outcome report |
9 Similar baseline |
10 Co-interventi-ons avoided |
11 Compliance acceptable |
12 Outcome timing similar |
Total |
|
Anderson & Maas, 1987 (24) |
Yes |
Unclear |
No |
No |
No |
Yes |
Unclear |
No |
Yes |
Unclear |
Unclear |
Yes |
4 |
|
Haskett et al., 2004 (25) |
Yes |
Unclear |
No |
No |
Yes |
Yes |
Unclear |
Yes |
Yes |
Unclear |
Yes |
Yes |
7 |
|
Kjeken et al., 1995 (26) |
Yes |
Unclear |
No |
No |
No |
Yes |
Unclear |
Yes |
Yes |
No |
Unclear |
Yes |
5 |
|
Pagnotta et al., 2005 (27) |
Yes |
Unclear |
No |
No |
No |
Yes |
Unclear |
Yes |
Yes |
No |
Yes |
Yes |
6 |
|
Stern et al., 1996 (22) |
Yes |
Unclear |
No |
No |
No |
Yes |
Yes |
Yes |
Yes |
Unclear |
Yes |
Yes |
7 |
|
Stern et al., 1996 (23) |
Yes |
Unclear |
No |
No |
Unclear |
Yes |
Unclear |
Yes |
Yes |
Unclear |
Unclear |
Yes |
5 |
|
Thiele et al., 2009 (28) |
Yes |
Unclear |
No |
No |
Yes |
Yes |
Unclear |
Yes |
Yes |
Unclear |
Unclear |
Yes |
6 |
|
Tijhuis et al., 1998 (29) |
Unclear |
Unclear |
No |
No |
Yes |
Yes |
Unclear |
Yes |
Yes |
Unclear |
Unclear |
Unclear |
4 |
|
Veehof et al., 2008 (30) |
Yes |
Unclear |
No |
Unclear |
No |
Yes |
Unclear |
Yes |
Yes |
No |
Yes |
Yes |
6 |
|
ITT: Intention to treat. |
|||||||||||||
For the van Tulder Scale, inter-rater agreement between reviewers for all items on each scale was examined and average Kappa coefficients were calculated to be 0.57 (95% confidence interval; CI 0.43–0.71). The Kappa coefficient for the Cochrane Risk of Bias tool was 0.56 (95% CI to 1.33–2.24). Both indicate moderate agreement between reviewers (46).
Three studies (31, 33, 34) of quasi-experimental and observational design had high methodological quality and 4 (32, 35, 36, 37) low methodological quality (Table V). It was unclear in these 4 low-quality studies whether the outcome assessor was involved in treatment or if the timing of the outcome assessment in all participants was comparable.
|
Table V. Cochrane criteria of methodological quality for quantitative studies of other design |
||||||||||||||||
|
Authors, year (ref) |
Criteria |
|||||||||||||||
|
a |
b |
c |
d |
e |
f |
g |
h |
i (a) |
i (b) |
j |
k |
l |
m |
Score |
Methodological quality |
|
|
Backman & Deitz, 1988 (31) |
Yes |
Yes |
No |
No |
Unclear |
Yes |
Yes |
Yes |
Yes |
No |
Yes |
Yes |
No |
Yes |
4, 4, 2 |
High |
|
Burtner et al., 2003 (32) |
Yes |
Yes |
Unclear |
Yes |
Unclear |
Yes |
Yes |
Yes |
No |
No |
Unclear |
Yes |
No |
Yes |
3, 3, 2 |
Low |
|
Nordenskiold, 1990 (33) |
Yes |
Unclear |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
No |
Unclear |
Yes |
No |
Yes |
5, 2, 2 |
High |
|
Cytowitz-Kapilowska et al., 1999 (35) |
Yes |
Yes |
Yes |
Unclear |
Unclear |
Yes |
No |
Unclear |
No |
No |
Unclear |
Yes |
No |
Yes |
2, 2, 2 |
Low |
|
Gumpel & Cannon, 1981 (36) |
Yes |
Yes |
Unclear |
Yes |
Unclear |
Unclear |
Yes |
Yes |
No |
No |
Unclear |
Yes |
No |
No |
2, 3, 1 |
Low |
|
Nicholas et al., 1982 (37) |
No |
Yes |
Unclear |
Unclear |
Unclear |
Yes |
Yes |
No |
No |
No |
Unclear |
Yes |
No |
No |
1, 2, 1 |
Low |
|
Pagnotta et al., 1998 (34) |
Yes |
Yes |
Yes |
Yes |
No |
Yes |
Yes |
Yes |
No |
No |
Yes |
Yes |
No |
Yes |
5, 3, 2 |
High |
|
Patient selection a) were the eligibility criteria specified? Interventions b) was the intervention explicitly described? c) were co-interventions avoided? d) was the compliance acceptable? Outcome measurement e) Was the outcome assessor not involved in the treatment? f) were the outcome measures relevant? g) were adverse effects described? h) was the withdrawal/drop out rate described and acceptable? |
i) timing follow-up measurements: a) was a short-term follow-up measurement performed? b) was a long-term follow-up measurement performed? j) was the timing of the outcome assessment in all patients comparable? Statistics k) was the sample size of the patient group described? l) did the analysis include an intention-to-treat analysis? m) were point estimates and measures or variability presented for the primary outcome measures? Internal validity – c, d, e, f, h, j. Descriptive criteria – a, b, g, i. Statistical criteria – k, m. Occupational therapy for rheumatoid arthritis (13). |
|||||||||||||||
Risk of bias across studies
Fig. 3 displays the overall risk of bias across the RCTs. Common methodological shortfalls within RCTs were inadequately concealed treatment allocation (n = 9) (22, 23, 24–30) and lack of blinding of assessors (n = 6) (22, 23, 24, 26, 27, 30). Additional failings noted were a lack of intention to treat analysis (n = 8) (23, 24–30) and the non-avoidance of co-interventions (n = 9) (22, 23, 24–30) such as pharmacotherapy regimens or physiotherapy.

Fig. 3. Risk of bias across randomized controlled trials (n = 9).
Within the quasi-experimental and observational studies (n = 7) (31–37) only one study explicitly stated that the outcome assessor was not involved in treatment (33). Short and long-term follow up measurements were absent across most studies with only one (31) performing short-term follow-up measurements.
The two qualitative studies (43, 44) did not detail the relationship between the researcher and participants, it was also unclear whether ethical issues had been considered. However, the research was judged to be valuable overall, taking the findings into consideration in relation to existing knowledge and its contribution to that knowledge.
Function/perception of function
Nine studies evaluated the effectiveness of a variety of working wrist splints on a range of functional tasks (22, 23, 25–28, 30, 31, 34). Two studies reported improvement in function (23, 28) but only one reached statistical significance (p < 0.05) with a large effect size for leather splints (d = 0.8) and medium effect size for fabric splints (d = 0.5) (28). One high quality RCT (28) found that both a custom made leather splint and a pre-fabricated splint improved function, with the leather splint being superior to the pre-fabricated splint (p = 0.008, d = 0.8). A low quality RCT (23) comparing 3 pre-fabricated splints found no significant difference between the splints with respect to measures of function. However, there was a patient reported improvement in the ability to perform some tasks such as carrying heavy items and driving with the use of all 3 splints. Six studies reported no change in function with use of splints (25–27, 30–32), 4 of these were RCTs, 3 of high (25, 27, 30) and one of low methodological quality (26). Two quasi-experimental studies, one of high (31) and one of low methodological quality (34) reported both no change (coin manipulation, shears task) and a decrease (ability to write, screwdriver task) in function with the use of splints. The remaining high quality RCT (22), reported statistically significant findings between splinted and un-splinted hands in favour of the un-splinted hand on a range of functional tasks (e.g. writing, p < 0.001, d = 0.1) card turning, p < 0.001, d = 0.3).
Grip strength
Nine studies evaluated grip and/or pinch strength (23, 24, 26, 28–33). One low quality RCT (26) and one low quality quasi-experimental study (32) reported improved pinch strength with the use of a variety of pre-fabricated splint and custom made splints, with the magnitude of the effect of splinting on pinch ranging from d = 0.3 to d = 0.9 in one study (32). Five studies (26, 28, 30, 31, 33) reported an improvement in grip with the use of a splint, however, only in one of these studies was that difference statistically significant (p<0.001, d = 0.3 and d = 0.4) (28). Conversely, one low quality RCT (23) and low quality quasi-experimental study (32) reported significant decrease in grip strength with the use of splints. One study (23) found grip significantly reduced with the use of 3 different splint types compared to no splint (p = 0.001); another (32) reported similar findings with the use of a hinged splint (p = 0.03).
Effect of working wrist splints on pain
The effects of the most commonly investigated outcomes are summarized in Table VI. Of the 8 studies that evaluated pain, 4 were high (25, 27, 28, 30) and two were low quality RCTs (26, 29). High quality RCTs reported statistically significant between group, short-term (2–4 weeks) reductions in pain using a range of pre-fabricated and custom made splints. Two studies (25, 28) compared custom made leather with various pre-fabricated splints, although all reduced pain, the custom made leather splints in both studies were significantly more effective, (p = 0.001, d = 0.79). One high quality quasi-experimental study (33) reported an immediate reduction in pain of 39% (d = 0.7), 42% (d = 0.7) and 52% (d = 0.8) when carrying out 3 activities of daily living (ADL). One high quality RCT (27) reported a statistically significant reduction in pain (p < 0.05) with the use of a pre-fabricated splint in 5/13 functional tasks. The remaining low quality RCTs and quasi-experimental studies (26, 29, 34) all reported a decrease in pain with the use of various splints. Kjeken et al. (27) was the only study to assess pain with or without splinting at long-term follow up (6 months).
|
Table VI. Summary of findings for: impact of splinting on most common outcome measures |
||||
|
Outcomes |
Authors, year (Ref) |
Direction of finding |
Statistically significant |
Measures |
|
Function/ perception of function |
Backman & Deitz, 1988 (31) Haskett et al., 2004 (25) Kjeken et al., 1995 (26) Pagnotta et al., 2005 (27) Stern et al., 1996 (22) Stern et al., 1996 (23) Thiele et al., 2009 (28) Veehof et al., 2008 (30) Pagnotta et al., 1998 (34) |
– = = = = – + – + = – = |
N/R N/R N/R Yes Yes Yes No No Yes No Yes Yes |
Ability to write Coin manipulation Arthritis Hand Function Test Health Assessment Questionnaire BTE work simulator Jebsen-Taylor Test Farm chores, yard work & some housework Some self care tasks, writing & typing COPM DASH & SODA-S Screwdriver task (BTE work simulator) Shears task (BTE work simulator) |
|
Grip/pinch strength |
Anderson & Maas, 1987 (39) Kjeken et al., 1995 (26) Stern et al., 1996b (23) Thiele et al., 2009 (28) Tijhuis et al., 1998 (29) Veehof et al., 2008 (30) Backman & Deitz, 1988 (31) Burtner et al., 2003 (32) Nordenskiold, 1990 (33) |
– + – + = + + (Hinged) – (Spiral) + + |
No N/R Yes Yes No No No Yes Yes N/R |
Sphygmamometer (grip) Sphygmamometer, Mannerfelt Intrinsicmeter (Tripod) Jamar Dynamometer (grip) Jamar Dynamometer (grip) Martin Vigorimeter (grip) Martin Vigorimeter (grip) Martin Vigorimeter (grip, tip & tripod) Jamar Dynamometer (Grip) Jamar Dynamometer (2-point pinch) Grippit (grip) |
|
Pain |
Haskett et al., 2004 (25) Kjeken et al., 1995 (26) Pagnotta et al., 2005 (27) Veehof et al., 2008 (30) Nordenskiold, 1990 (33) Pagnotta et al., 1998 (34) Thiele et al., 2009 (28) Tijhuis et al., 1998 (29) |
+ + + + + + + + |
Yes N/R Yes 5/13 tasks Yes N/R No Yes No |
Visual Analogue Scale Visual Analogue Scale Visual Analogue Scale Visual Analogue Scale Visual Analogue Scale Visual Analogue Scale AUSCAN Visual Analogue Scale |
|
Dexterity |
Stern et al., 1996 (22) Backman & Deitz, 1988 (31) Burtner et al., 2003 (32) Pagnotta et al., 1998 (34) |
– – (Spiral) + = – |
Yes No Yes No Yes |
The Purdue Test Writing speed, coin manipulation Nine hole peg test Nine hole peg test (hinged, static and no splint) Jebsen Hand Function Test |
|
+: positive effect on outcome; –: negative effect on outcome; =: no effect on outcome; N/R: not recorded; BTE: Baltimore Therapeutic Equipment Co.; COPM; Canadian Occupational Performance Measure; AUSCAN: Australian/Canadian osteoarthritis Hand Index; DASH: Disabilities of the Arm, Shoulder and Hand; SODA-S: Sequential Occupational Dexterity Assessment (short version); ESR: erythrocyte sedimentation rate. |
||||
Dexterity
Four studies measured dexterity (22, 31, 32, 34), two of which found a statistically significant decrease in dexterity with the use of a splint (22, 34). One study (34) reported that the average time to complete all 7 tasks on the Jebsen Hand Function Test was longer (4.4 s) when wearing a pre-fabricated splint when compared to no splint (p = 0.0086, d = 0.2). Although Stern et al. (22) found no difference between 3 pre-fabricated splints, all 3 reduced finger dexterity (p < 0.001). There was no difference in dexterity in an alternating treatment design study (31), with and without a custom made splint on coin manipulation. However, conversely these authors found writing dexterity reduced with the use of the splint. Only one specific splint (spiral splint) within the study by Burtner et al. (33) was found to significantly improve dexterity (p = 0.03) measured using the 9-hole peg test.
Summary of strength of evidence
To construct best evidence synthesis for quantitative studies 5 RCTs were rated as high quality (22, 25, 27, 28, 30) and four as low quality (23, 24, 26, 29). There is strong evidence that working wrist splints reduce wrist pain, and the magnitude of this reduction was found to be medium. This is supported by consistent, statistically significant differences in three high quality RCTs (25, 28, 30). further supported by one high quality quasi-experimental study (33). There is moderate evidence that grip strength was improved and dexterity impaired with the use of a working wrist splints (22, 36). There is insufficient evidence in relation to the effect of working wrist splints on function due to conflicting results (27, 28, 30).
Meta-ethnographical analysis of qualitative studies
Two qualitative studies using a phenomenological design investigated the use and preference of wrist splints (44) and the determinants of wrist splint use (43). Additionally 5 cohort studies investigated wrist splint compliance (38, 39) and usage of wrist splints (40, 41, 42). Several experimental studies (23, 25, 30, 36, 37) provided additional qualitative data by reporting questionnaire results in addition to the primary outcomes measured.
Related themes and concepts from study participants and researchers within the studies were extracted, compared and interpreted to build key translations (Table VII).
|
Table VII. Meta-ethnographical analysis of qualitative studies. Reciprocal translation |
|||
|
Primary themes (views of participants) |
Secondary themes (interpretations of authors) |
Key translations |
|
|
Prescription & knowledge |
Purpose of splint (satisfied with information given, not enough information given, not returning to clinic to clarify information). Incorrect information about splint use and care. Choice of splint on prescription (no choice, choice of two types |
Clinical study results emphasise importance of informing patients the time taken to become accustomed to splint, benefits and drawbacks, effects on function. Health professionals should consider specific attributes when assessing different brands. No single style of splint suits all; single style decrease operating costs but limits the likelihood of optimally matching patient to splint. Should try on and perform functional tasks in clinic before deciding on a splint. Using an independently purchased splint may aggravate symptoms as each splint needs adjustment. Patients know their preferred splint within a few minutes |
• More time spent on initial prescription • Choice of splint on prescription • Functional assessment with splint • Detailed written and verbal information |
|
Splint use |
Linked to: perception of seriousness of symptoms (pain, swelling, tingling), perception of usefulness of splint (increase function, ability to decrease symptoms, immobilisation of wrist allows greater use of whole upper limb, increased strength, not enough range of motion allowed for dressing, how comfortable splint is). Balance between benefits and drawbacks |
Splint use dependent on seriousness of symptoms (use splint to primarily reduce symptoms). Other reasons for use (support and or immobilise wrist). Use related to intentional decisions. Detrimental and beneficial effects reported for functional ability largely in accordance with other studies. Conflicting results may be attributed to differences in daily activities and time between fitting splint and measurement. Perceived functional ability likely to be task dependent. Hierarchy of subjective attributes used to determine splint choice when choice of 3 given |
• Primary use of splint is to decrease symptoms of pain and swelling • Task dependent use • Patients seek varying degrees of mobilisation/immobilisation |
|
Compliance |
Daily use, nocturnal use, non-use. Linked to splint decreasing functional ability, performing dirty and or wet tasks, unable to fit gloves or long sleeved tops over splint, unable to wear a watch, decreased dexterity with use. Decreased driving ability. Perceived need for wrist support versus irritation of immobilisation. Do not wear all the time as afraid of wrist becoming stiff |
Non-compliance related to perceived disadvantages of splint (decreased functional ability, dirty/wet activities, concerns with comfort and or fit). Knowing the determinants of splint use allows measures to be taken to increase compliance. Educational and behavioural strategies should include: shared outcome expectations, verbal and written instructions, monitoring adherent behaviour, evaluation of the regime. Compliance less likely if only one choice of splint |
• Wide variance in amount of time used • Patient choice will affect compliance • Patient knowledge will affect compliance • Monitoring patients will affect compliance |
|
Splint attributes |
Gets wet and dirty easily, light colour dirties more easily, long drying time if wet, velcro sticks to and frayed clothing, stitching unravelled. Appearance (neutral on appearance as long as it works). Different opinions on different designs of splint (positive and negative, like and dislike padded material, heat increase with padding). Fit and comfort variable (positive about fit and comfort, hard metal bar uncomfortable, sweaty, loose or uncomfortable tight, cannot tighten at wrist, paresthesia after wearing). Metal bar (stay hems to deep or narrow to firmly fix metal strap or allow removal). Web space (too wide, chaffing 1st web space) |
Disadvantages (long drying time, unpleasant physical contact with the splint because of hard metal stay). Design elements evoked strong responses: contact with dorsal MCP’s, overcast finishing, wide adjustable web space. Critical of lack of material to allow closure at proximal forearm. Temperature less important to most but warmer splints rejected when heat was a critical issue. Appearance and ability to keep clean not a major concern and rarely cited for accepting or rejecting a splint. Patients are likely to take but not use an uncomfortable splint |
• Choice and will allow patient examination of individual attributes and less likely to lead to rejection of a splint • Patients more concerned with utility than appearance but will reject a splint on comfort • Design aspects could be improved (stay hems, length of forearm, width of web space, length of dorsum, straps) |
|
Social factors |
Prevents people squeezing hand when shaking hands. People offer to help when splint on. Attracts unwanted attention (staring, asking what is wrong). Reactions of society did not influence use. Able to lift grand/children without pain. Persuaded by partners to wear/not wear in some situations. Do not wear going to parties or visiting people. Skin bulging between straps (indication they were overweight) |
Social cognitive theory and theory of planned behaviour suggest social environment an important determinant – not a major influence in decision to wear/not wear in this study (Stern). Other people trying to prevent wrist overburdening (Less hand squeezing, opening doors). Overweight people did not bring up the fact that straps bulged – perhaps embarrassed or assumed unique to someone of their size |
Splint used as a warning to others of pain Social environment not a major influence on use |
|
Table VII. Contd. |
|||
|
Primary themes (views of participants) |
Secondary themes (interpretations of authors) |
Key translations |
|
|
Ease of use |
Difficultly don/doffing for some. Need support to put on (table to support arm, use teeth to undo straps, cannot remove independently). Difference in straps (d-rings difficult to re-thread with morning stiffness, difficulty lining straps up for correct tension d-rings easier). Choose not wear rather than continual on/off |
Questions the notion that additional forearm length and wide adjustable straps improve comfort and fit |
• Design aspects could be improved to affect compliance • Choice and assessment at prescription will clarify ease of use |
|
Side effects/additional effects |
Improved sleep (resting pain decreased), prevents wrist overloading, increased security, feeling of protection, decreased palmar sensation impairing grip, fatigue at shoulder and elbow due to immobilised wrist, distracting tactile stimulation on dorsum of MCP’s, distal edge constricting MCP’s |
Fear of weakening/stiffening the wrist. Advantages (rest resulting from immobilisation) |
• Day time use can decrease resting pain, in turn improving sleep • Clear written and verbal instructions needed • Design aspects could be improved |
|
Expectations |
Positive and negative expectations for splint reducing symptoms |
Importance of promoting realistic expectations to increase adherence. Check expectations are reasonable |
• Expectations discussed at initial assessment and prescription |
Themes
Prescription, knowledge and splint use. Spoorenberg et al. (43) found that 93% of rheumatologists advised patients to use their splints often or almost always during activity and 11% advised patients to use it at night. Another study (43) found that most participants were aware of the purpose of their splints, although those who had inaccurate knowledge tended not to return to the prescriber for further advice. Several studies found that splint use was explicitly linked to patients’ perceptions of the seriousness of their symptoms (38, 40, 41, 43, 44). Non-use was also evident in observational studies (37, 38). The most commonly cited reason for use of the splint was for the reduction of pain and swelling (25, 33, 40, 42, 43, 30, 38, 44).
The reported effect of splinting on function varied. In one study (43), the majority of participants experienced a decrease in function with use of the splint, however, others cited improved functional ability with splint use (39–44). Common functional tasks for which the splint was removed were ‘wet’ and ‘dirty’ tasks (43) with two studies reporting the inability to fit gloves over the splint a reason for non-use (23, 43). Contrary to this Agnew & Maas (39) found a high percentage (71.4%) of their respondents (n = 130) used their splint when washing dishes. One study (44) reported splint use for performing heavy tasks such as farm chores, mowing lawns and raking leaves, and another (41) found differences between the type of splint prescribed as a deciding factor for attempting to carry out tasks such as gardening or hanging out clothes.
The negative effect of working wrist splints on dexterity was commonly reported (38) where participants wore their splints for activities which required greater strength and less dexterity. Three studies reported increased strength (38, 43, 44). In another study no perceived change in grip strength was also reported (43).
Adherence and social factors. A survey of rheumatologists and RA patients (42) found that 16/21 participants advised to wear their splint when physically active adhered to this advice. Six participants were advised to wear at night with none complying. Another survey (39) found that over 70% of 265 Australian patients wore their splint as advised. However, non-adherence is common; 19.4% (7/36) of participants in one (38) and 42% (54/128) in another survey (40) did not wear their splint at all. Decreased functional ability (43), difficulty with using and having no symptoms (40), were cited as reasons for non-use.
The social environment was also a consideration (43, 44). The splint was felt to prevent people shaking hands, often attracted unwanted attention, staring and questions (44). Family and partners were also reported as influencing wear in some situations (44). Characteristics which deemed certain splints to be unsuitable for males were reported as appearance and poor suitability to ‘male’ tasks.
Splint attributes. Splint appearance was deemed to be largely irrelevant in some studies with participants more concerned with their effectiveness (39, 43, 44). However, 14 of 32 participants found their splint unwieldy and 9 thought it ugly (42). When participants in an RCT (28) (n = 47) comparing three splint types were questioned on satisfaction with splint appearance, 91%, 75% and 72% of participants were satisfied with the appearance of three different splints.
Combined synthesis. The use of working wrist splints was reported to be explicitly linked to the seriousness of symptoms such as pain. This appears to support the findings of the quantitative literature. The inconclusive effect of working wrist splints on function was also evident with patients giving variable accounts of use and non-use for particular functional activities. The impact of splint use on dexterity and strength was also highlighted in the qualitative literature and again supports findings from the quantitative literature that dexterity is impaired with splint use. Additional factors such as ease of use, cosmesis and the social environment appear to be linked to splint use, however, this requires further exploration in order to reach definitive conclusions.
DISCUSSION
The aim of this mixed methods systematic review was to determine the effectiveness of working wrist splints in adults with RA. The results of the analysis of the 23 studies in this review suggest that working wrist splints reduce pain in patients with RA. In addition, the synthesis of the qualitative studies confirmed that the primary use of splints by people with RA is to decrease pain and swelling. This finding is accepted with the caveat that results are based on relatively few studies which are of variable quality. The results also suggest that there is moderate improvement in grip but an inconclusive effect on function with splint use, and it appears that dexterity can be negatively affected. The synthesis of qualitative data suggests that splint use is task dependent. This may reflect the effect of splint use on dexterity and therefore use or non-use becomes a personal decision based on experience of use for individual functional tasks.
The wide variety of splint types and variability in disease duration coupled with often inadequate detail on precise wearing regimes, including immediate versus longer term wear, prevent definitive conclusions about which splint types and wearing regimes are associated with better outcomes.
Working wrist splints impact on function appears to be task specific. Tasks for which function was improved with splint use across studies were tasks where strength was required (lifting, pushing, and pulling) such as vacuuming, yard sweeping, lifting heavy objects. It can be argued that this is strongly linked to the studies which found that splints increase grip strength. The link between decreased dexterity and ability and reported use of splints for functional tasks which require finer manipulation is also apparent. Patients tended not to wear their splints for tasks where dexterous manipulation was required.
Of particular note, this review has identified that the terminology used to describe functional activity of the hand or upper limb as a whole is inconsistent across studies. Common terms included: hand related activities, dexterity, upper limb function, applied dexterity, applied strength, fine motor tasks, hand and upper extremity functions, and functional activities. Further, the subtle interconnection between hand function and upper limb function is not made explicit across studies and a gap in the literature with respect to the definition of upper limb function and its measurement is apparent. Stern et al. (22) differentiated between dexterity and hand function based on the size of objects being manipulated. Assessments using objects smaller than 2.5 cm are considered finger dexterity tests. Those using objects larger than 2.5 cm are considered manual dexterity and hand function tests and measure the speed of hand use across object sizes, often simulating functional activities including upper limb function. It could be argued the latter translates to primarily upper limb function rather than solely hand function. Difficulty in extracting the detail of working wrist splints’ impact on function and in particular upper limb function is further complicated by the intricate link between pain and ability to carry out functional activities.
There was a diverse range of outcome measures used, including both standardised and non-standardised measures, which, to some extent, hampered meaningful comparisons to be made.
The range in disease duration within and between the investigated studies does not allow definitive conclusions to be drawn about the optimum time for splint prescription. Treatment guidelines (2, 8, 9) highlight the need for early intervention and as evident in the qualitative synthesis improved education and prescription protocols.
This is the first mixed methods systematic review to evaluate the effectiveness of working wrist splints in the treatment of people with RA. Previous reviews evaluating a range of upper and lower limb splints have concluded that working wrist splints have no positive effect on pain relief (10), that splints in general can decrease pain (12, 13, 49) and improve strength (13, 49), but that they may decrease hand movements (13). In agreement with the current review, previous systematic reviews (11, 12, 47–49) highlight the limited evidence for the effectiveness of working wrist splints in improving range of motion, grip strength or slowing down of deformity. Methodological weaknesses such as small sample sizes, large variations in duration of disease within studies and inconsistencies in reporting are reinforced.
Strength and limitations of current review
Restricting the search to English language articles, and excluding conference proceedings may have resulted in the omission of relevant research. Further no formal mechanisms, such as funnel plots, were used to identify if publication biases affected results. A narrative approach to the synthesis of quantitative studies provides an auditable process to address potential bias in relation to the identification and synthesis of studies. This has been argued as producing reliable and generalizable conclusions (50) and highlights key messages from the literature. However, over-interpretation of the data is recognized as a limitation of this approach. Also of note is the inclusion of cross-over studies which may lead to inconclusive or biased results if the methodology is not carefully analyzed or the number of participants is very few (29), since it does not truly compare interventions between groups but within subjects.
There are a wide range of splints used with patients with RA. However, the focus of this literature review is on working wrist splints and therefore other splint types were excluded. Studies investigating splints used following surgical procedures were excluded as the use of this splint following surgery is primarily to allow for healing of anatomical structures. Splints used as part of extensive OT treatment programmes were also excluded as the inherent effect of co-interventions would increase the likelihood of threats to internal validity.
While there have been previously published reviews on this topic (10, 11, 12, 13, 18, 48, 49), this current review has systematically examined the full breadth of the literature, allowing for additional studies, of all methodologies to be included, which give a richer, more contextualized interpretation of the data. Also included are studies which have been carried out since the completion of previous reviews (28, 30, 40, 43).
Implications for future research
Future studies should meet basic requirements that minimize selection and detection bias (adequate randomization and assessor blinding). Studies should be adequately powered with a combination of validated outcome measures in order to accurately capture effect. Objective measures of global upper limb functional activity should be considered and combined with subjective measures of pain and functional activity. There is also a need for more studies examining the human dimensions and experiences of both the consumers and providers of working wrist splints.
Conclusion
This review has demonstrated that working wrist splints reduce pain in patients with RA. In addition, the synthesis of the qualitative studies confirmed that the primary use of splints by people with RA is to decrease pain and swelling. Results also suggest that there is moderate improvement in grip, inconclusive effect on function and a negative impact on dexterity. However, there have been few rigorously conducted clinical trials, and many with methodological shortcomings, and little homogeneity between studies in relation to splints. Outcome measures and the population studied prove problematic in providing definitive answers for clinicians on which to base clinical practice.

1http://www.medicaljournals.se/jrm/content/?doi=10.2340/16501977-1804
REFERENCES
