Peter Währborg, MD, PhD1, Ingemar F. Petersson, MD, PhD2 and Patrik Grahn, PhD1
From the 1Swedish University of Agricultural Sciences, Department of Work Science, Business Economics and
Environmental Psychology, Alnarp and 2Epi-Center Skåne, Department of Orthopedics, Clinical Sciences Lund,
Lund University, Lund, Sweden
OBJECTIVE: To determine the effect of a nature-assisted rehabilitation programme in a group of patients with reactions to severe stress and/or mild to moderate depression. Changes in sick-leave status and healthcare consumption in these patients were compared with those in a matched population-based reference cohort (treatment as usual).
DESIGN: Retrospective cohort study with a matched reference group from the general population.
SUBJECTS: A total of 118 participants referred to a nature-assisted rehabilitation programme, and 678 controls recruited from the Skåne Health Care Register. For both groups, information on sick leave was extracted from the National Social Insurance Register and on healthcare consumption data from the Skåne Health Care Register.
METHODS: The interventional rehabilitation programme was designed as a multimodal programme involving professionals from horticulture and medicine. The programme was conducted in a rehabilitation garden, designed especially for this purpose.
RESULTS: A significant reduction in healthcare consumption was noted among participants in the programme compared with the reference population. The main changes were a reduction in outpatient visits to primary healthcare and a reduction in inpatient psychiatric care. No significant difference in sick-leave status was found.
CONCLUSION: A structured, nature-based rehabilitation programme for patients with reactions to severe stress and/or depression could be beneficial, as reflected in reduced healthcare consumption.
Key words: nature; horticultural therapy; burnout professional; psychological stress; depression.
J Rehabil Med 2014; 46: 00–00
Correspondence address: Peter Währborg, Swedish University of Agricultural Sciences, Department of Work Science, Economics and Environmental Psychology, PO Box 88, SE-230 53 Alnarp, Sweden. E-mail: Peter@Wahrborg.se
Accepted Sep 9, 2013; Epub ahead of print 28 jan, 2014
INTRODUCTION
The global burden of neuropsychiatric diseases is substantial, and will continue to be a major threat to public health long into the future (1). Each year, more than one-third of the total population of the European Union experience mental disorders, and less than one-third of all cases receive any treatment or rehabilitation, suggesting a considerable level of unmet need (2). In addition to the resulting suffering and the years lost to disability, the costs are considerable. Gustavsson et al. (3) calculated that the costs for all neuropsychiatric disorders in Europe in 2010 were €798 billion. They found that direct costs constituted the majority (with 37% reflecting direct healthcare costs and 23% direct non-medical costs), whereas the remaining 40% were indirect costs associated with patients’ production losses.
In Sweden, as well as in other countries, the contribution of psychiatric disorders to sickness absence has increased markedly (4–6). It has been claimed that stress-related factors, especially in work, account for a significant part of this burden (7). The growing amount of sick leave attributed to stress- and work-related factors calls for increased demands for effective rehabilitation programmes. Psychological complaints, often provoked by mental stress, constitute a major rehabilitation issue.
The effects of rehabilitation on sickness absenteeism and work ability have been reviewed by Kuoppala & Lamminpää (8). They point out that the support for rehabilitation is mainly weak, but that there is moderate evidence that multimodal rehabilitation decreases the risk of disability pension and that return-to-work programmes decrease the amount of sick leave lasting longer than 6 months, whereas counselling, exercise, multimodal medical rehabilitation and return-to-work programmes do not have an effect on return to work at 1 year.
Patients defined as having reactions to severe stress and/or mild to moderate psychological complaints typically show a rate of termination from the sick-list or return to work at 1 year of 40–80% (9–11). However, the outcome of comparative and controlled studies shows no or only marginal differences between different rehabilitation strategies or in comparison with treatment as usual (TAU) (10, 12–14). In an extensive review of the literature concerning return to work after mild psychiatric illness, approximately 40 studies were identified (15). Only a small number of studies show superior effects of a rehabilitation programme compared with untreated controls (11, 16).
Nature-assisted therapy and rehabilitation has a long tradition in healthcare (17). Over the past 20 years, research in this area has increased progressively. Three review articles have been published in recent years (17–19). Annerstedt & Währborg (19) analysed 38 carefully selected and well-conducted scientific studies on the impact of nature-assisted therapy (NAT). They concluded that NAT leads to significant improvements in different outcomes in different diagnoses. Jang et al. (18) selected 108 well-performed studies regarding nature-assisted treatment and rehabilitation for a detailed meta-analysis. The mean effect size of NAT was 0.71 (Cohen’s d), of which the effect size was greatest (> 1.0 Cohen’s d) for children and for diagnoses related to mild to moderate mental illness. Furthermore, the effect size was highest at 20–30 treatment occasions and for groups of 6–10 participants. Several well-conducted RCTs and studies of similar design have been published recently. Nature-assisted therapy and rehabilitation has proven to be better, or at least as good, as usual treatment and rehabilitation, whether measured with different types of self-rating scales (20–23), function tests (20, 22, 24, 25), or samples of physiological markers (26, 27).
We define NAT as an intervention with the aim to treat, hasten recovery, and/or rehabilitate patients with a disease or a condition of ill health, with the fundamental principle that the therapy involves plants, natural material, and/or outdoor environment. The therapeutic programme comprises group as well as individual activities in a specially designed garden with the aim to offer unconditional, multi-sensory stimulation in an enriched environment to promote physical activity and soft fascination in a natural context. Soft fascination, i.e. effortless attention which provides a pleasing level of sensory input that involves no cognitive effort; it is deemed to occur when there is enough interest in the surroundings to hold attention but not so much that it compromises the ability to reflect. Individual activities are combined with group activities in a structured programme that includes physical therapy, psychotherapy and other usual features of a rehabilitation programme.
In this study we applied a nature-assisted rehabilitation programme in a group of patients with mild to moderate depression and/or reactions to severe stress. The aim was to investigate changes in sick-leave status and healthcare consumption in these patients compared with a control group (treatment as usual) in available healthcare registers. The hypothesis was that this intervention would show a favourable outcome.
METHODS
Study population
From late 2002 to early 2008 a total of 118 participants were referred to a nature-assisted rehabilitation programme at the Swedish University of Agricultural Sciences, Alnarp in southern Sweden. The referrals were issued by social insurance offices in Sweden due to long-term sick leave and a diagnosis of reactions to severe stress and/or depressive disorder. The participants were identified consecutively by social insurance officers from a register of ongoing sick-listings.
Inclusion criteria were: (i) being on sick leave for at least 3 months due to a diagnosis of reactions to severe stress (see below) and/or depression, defined as having an International Classification of Diseases (ICD-10, tenth revision, second edition, 2005) within the F43 and/or F32 category; (ii) understanding of spoken and written Swedish; and (iii) absence of any other severe psychiatric illness.
After oral and written information about the study were provided, and if the inclusion criteria were met, participants were asked for their consent and were thereafter included in the programme. The study was approved by the Research Ethics Committee at the Medical Faculty of Lund University (LU 107-02 and EPN Lund 2011/31).
All participants were seen by a psychiatrist within the programme and had their diagnosis reconsidered and confirmed before being included in the programme. Six patients did not fulfil the inclusion criteria and were therefore excluded. Sixty-nine of the participants included in the intervention programme were defined as primarily having (“main condition” according to ICD-10) from reactions to severe stress (F43. 8 or 9).
Twenty-seven participants primarily had (main condition) a mild to moderate depressive episode (F32.0 or F32.1), 3 participants had a severe depressive episode without psychotic symptoms (F32.2), and 4 participants had a severe depressive episode with psychotic symptoms. Furthermore, 8 participants had post-traumatic stress disorder (PTSD) (F43.1) and 1 adjustment disorder (F43.2). Ninety-six percent of the participants had more than 1 diagnosis, and 67% had more than 2 diagnoses. Twenty-nine percent of the participants had more than 3 diagnoses. The most frequently occurring other conditions were other mental or behavioural disorders (F00–F99), diseases of the musculoskeletal system and connective tissue (M00–M99) and diseases of the nervous system (G00–G99).
Of the 112 participants who fulfilled the inclusion criteria, 7 were excluded from further analysis and comparisons because they did not live in the geographical region (Skåne) and could therefore not be matched with proper controls in the available registers. Another 2 participants passed the age limit for retirement (65 years) during the rehabilitation programme, and it was therefore not possible to analyse them regarding sick leave. A final total of 103 participants remained for comparison with the reference group.
Reference group and registers
The control group was recruited from the Skåne Health Care Register (SHCR) in the Skåne Region in southern Sweden (28, 29), with an intent to recruit 8 controls per case. However, this was not possible in all cases, since a sufficient number of good matches were not found for some of the cases, especially the younger ones. Thus, the final number of controls, matched for main condition, age and sex, was 678. The controls were not matched for other conditions. Medical diagnoses (ICD-10) of controls were taken from the Skåne Health Care Register. Start of illness period was defined as the day the participant started his/her sick leave, i.e. the sick-leave episode which overlapped the day the participants started in Alnarp. This principle was applied to the participant, as well as to his/her matched control. Thus, the controls had to have their ongoing episode of illness during the same time-period as the cases began their participation in the rehabilitation programme. An attempt was made to match the initial dates of their illness periods with the cases’ respective initial dates. Each control subject was included only once in the comparisons. This methodology has been used extensively and has also been validated in other studies (28, 29).
The 678 matched control patients, as well as the 103 cases, were identified in the SHCR for the period between 2000 and 2009. In this register both outpatient and inpatient care, provided by all healthcare providers within the public health service, is recorded. The total material is gathered from databases covering more than 4 million entries per year, including private care. The number of private healthcare contacts which have not been recorded in any database constitute only a very small proportion of all contacts. Healthcare consumption was calculated 1 year before and 1 year after the first day of participation in the rehabilitation programme. For inpatient care, the day of registration was considered the first day of contact. Known clinical and demographic data for case and control groups are shown in Table I.
|
Table I. Baseline characteristics of intervention and control groups |
|||
|
Variable |
Intervention group (n = 103) |
Control group (n = 678) |
p-value |
|
Sex, female/male, n (%) |
92 (89)/11 (11) |
600 (88)/78 (12) |
ns |
|
Age, years, mean (SD) |
45.9 (9.7) |
46.3 (9.7) |
ns |
|
Family situation, n (%) |
|||
|
Living alone |
34 (33) |
213 (32) |
Distribution |
|
Living with another adult |
69 (67) |
462 (68) |
ns |
|
Socioeconomic classificationa, n (%) |
|||
|
(1) Manual worker |
9 (9) |
||
|
(2) Professional worker |
2 (2) |
||
|
(3) Subordinate official/employee |
14 (13) |
||
|
(4) Official/employee – intermediate position |
66 (64) |
||
|
(5) Official/employee – high ranking |
12 (12) |
||
|
Sick-listed until start of programme |
|||
|
Mean months (SD) |
43.3 (25.4) |
||
|
Median months (range) |
42 (3–107) |
||
|
Year included in the programme, n (%) |
|||
|
2002 |
8 (8) |
52 (8) |
|
|
2003 |
33 (32) |
212 (31) |
|
|
2004 |
13 (13) |
78 (11) |
Distribution |
|
2005 |
14 (14) |
93 (14) |
ns |
|
2006 |
18 (17) |
128 (19) |
|
|
2007 |
14 (13) |
91 (13) |
|
|
2008 |
3 (3) |
24 (4) |
|
|
Primary diagnosis, n (%) |
|||
|
Exhaustion syndrome |
67 (65) |
484 (71) |
|
|
Depression |
28 (27) |
194 (29) |
Distribution |
|
PTSD |
8 (8) |
0 |
ns |
|
On antidepressant medication, n (%) |
49 (47) |
||
|
On anxiolytic medication, n (%) |
11 (11) |
||
|
On other psychotropic medication |
18 (17) |
||
|
aAccording to Swedish socioeconomic classification (3). SD: standard deviation; PTSD: post-traumatic stress disorder; ns: not significant. |
|||
Outcome measures
Sick-leave status and healthcare consumption were primary outcome variables in this study.
Definitions
Social insurance is an integral part of the Swedish social security system. The Swedish social insurance covers basically everyone living or working in Sweden. If an insured citizen becomes sick for a shorter period of time, he/she is entitled to sickness benefit (SB). An insured citizen can also be entitled to SB if he/she is studying at school or participating in an internship at a workplace. If aged between 19 and 29 years, one might be eligible for activity compensation (AC) if one’s work capacity is reduced by at least 25% for at least 1 year. Persons aged between 30 and 64 years might be able to receive sickness compensation (SC) if their work capacity is permanently reduced by at least 25%.
The intervention method
The interventional rehabilitation programme was designed as a multimodal programme involving professionals from the “green sector”; that is, horticulturalists and landscape architects, as well as traditional medical professionals such as physiotherapists, occupational therapists, psychotherapists and medical doctors. The programme was conducted in a green setting (a rehabilitation garden), designed especially for this purpose (30, 31). The combination of restorative natural areas with horticultural activities and traditional rehabilitation has been shown to be an efficient setting in rehabilitation (19).
The method draws on supportive environment theory (SET) (32), which is based on the assumption that human beings, through evolution, are adapted to a life close to nature, in social and cultural interaction with a limited number of people. “Supporting environments” consist of physical (e.g. natural and built environments), social (e.g. work and leisure, including companion animals) and cultural (e.g. language, values, lifestyle) environments. SET claims that people need supportive environments to develop physically (body, senses, muscles, locomotion) and mentally (being able to feel and think) in immediate interaction with the physical, social and cultural environment.
The programme normally comprises 12 weeks, starting with individually adapted time for active participation in the activities. An individual plan is designed for each participant. The time spent in the garden or in the programme increases over time, depending on the participant’s condition. Most of the time is spent outdoors in gardening activities, relaxation exercises, psychotherapeutic activities, walking, etc. A more complete description of the programme can be found in Grahn (32).
In short, the advantages of the method are believed to be:
• A great deal of time is spent outdoors, thereby promoting natural physical activity.
• Nature in itself offers an enriched and secure environment, with multisensory stimulation.
• The natural attachment to nature.
• The symbolic and meaningful activities that can be carried out as part of the programme.
Statistical methods
A χ2 test and Welch’s t-test were applied for descriptive data. For comparisons of proportions, the standardized mortality rate (SMR) was calculated (33). The analysis of variance (ANOVA) test for regression was applied, and the risk ratios with 95% confidence interval (CI) were also calculated.
RESULTS
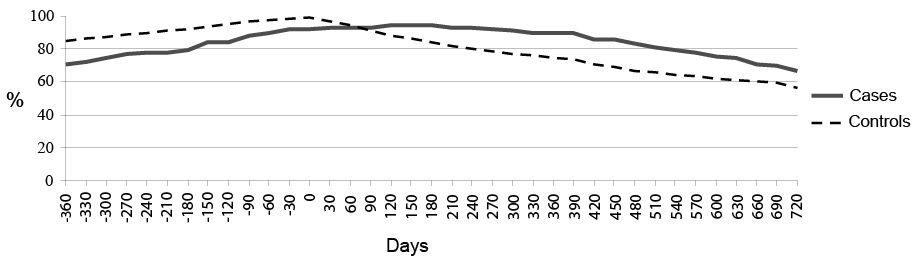
In the first outcome variable, the proportion of individuals on “sickness benefit or compensation” at baseline was higher for the controls than for those participating in the rehabilitation programme (cases). The reason for this was that 16% of the cases had other forms of economic support or compensation than those included in the regional social insurance register, and were therefore not included in the register-based comparison. However, none of them were available for the labour market due to ill health. Different types of financial compensation for patients, and difficulties finding controls that matched cases accurately with respect to day of illness, led to a shift in the curves in Fig. 1. We interpret this as there were no substantial differences between cases and controls regarding any kind of sickness benefit or compensation before or after the rehabilitation programme. Data for both cases and controls were obtained from the same regional social insurance register.
The second endpoint was healthcare consumption: both cases and controls had an ongoing sick-leave episode at the time of the start of a rehabilitation programme in Alnarp. Thus, they differed from the entire population, which also affected their healthcare consumption.
Fig. 1. Proportion of cases and controls with any kind of ongoing sickness benefit at different time-points from 360 days before to 720 days after inclusion (at 0 days) in the rehabilitation programme.
The mean number of healthcare contacts per person and per year in the entire population of the Skåne Region in 2005 (age group 45–64 years) was 6.8 (women 8.0 and men 5.5), and the mean number of hospital days per person and year was 0.9 (women 0.8 and men 1.0) (source: Skåne Health Care Register).
The population studied had a mean of approximately 26 healthcare contacts per person and year, and 7 hospital days per person and year, i.e. 4 times more healthcare contacts and approximately 8 times more hospital days than the entire population. This difference concerned all care areas, but was especially high for psychiatric care, where the number of cases was as much as 20 times more healthcare contacts per person and year compared with the population (10.6 vs 0.57). The equivalent for the number of patient days in psychiatric care was approximately 26 times higher (6.3 vs 0.24).
As shown in Table II, the number of healthcare contacts and the number of hospital days decreased after the start of a rehabilitation programme in Alnarp compared with before the start in Alnarp, for both cases and controls. The number of visits to any kind of healthcare contact was 28.7 for the cases 1 year before the programme and 24.1 1 year after the programme (a reduction of 16%) and the corresponding figures for the controls were 18.3 before and 16.8 visits after; a reduction of 8.2%. An ANOVA regression analysis proved that there were significant reductions in the number of healthcare contacts for the cases 1 year after compared with 1 year before (cases SMR 0.84, 95% CI 0.81–0.87; controls SMR 0.92, 95% CI 0.90–0.93).
|
Table II. Proportions of healthcare contacts 1 year after and 1 year before the rehabilitation programme: cases and controls |
||
|
Type of contact |
Cases 1 year after/ SMR/rate (95% CI) |
Controls 1 year after/1 year before SMR/rate (95% CI) |
|
Outpatients |
||
|
Somatic healthcare |
0.95 (0.86–1.04) |
0.94 (0.90–0.99) |
|
Psychiatric healthcare |
0.95 (0.89–1.01) |
0.90 (0.87–0.93) |
|
Primary healthcare |
0.72* (0.68–0.77) |
0.92 (0.90–0.95) |
|
Total |
0.84* (0.81–0.87) |
0.92 (0.90–0.93) |
|
Bed days |
||
|
Somatic healthcare |
8.40* (6.93–9.87) |
1.60 (1.42–1.78) |
|
Psychiatric healthcare |
0.35* (0.31–0.39) |
0.76 (0.69–0.82) |
|
Total |
0.47* (0.43–0.52) |
0.94 (0.87–1.00) |
|
*p < 0.05. CI: confidence interval; SMR: standard morbidity ratio; SMR/rate: ratio. |
||
The decrease was significantly greater, in total and especially in cases compared with controls concerning primary healthcare (cases SMR/rate 0.72, 95% CI 0.68–0.77; controls SMR 0.92, 95% CI 0.90–0.95) and inpatient days in psychiatric healthcare (cases SMR/rate 0.35, 95% CI 0.31–0.39; controls SMR 0.76, 95% CI 0.69–0.82). There was one exception; bed days in somatic care. However, the cases had comparatively very few bed days in somatic care before intervention (only 0.1 days per person, compared with 9.3 days in psychiatric care) (Table II).
For the entire period of 1 year before and 1 year after the start of rehabilitation in Alnarp, cases had 48% more healthcare contacts per person compared with the controls (Table III). For bed days, this number was approximately 5 times higher. Both before and after the start of rehabilitation in Alnarp cases had higher numbers than controls, but this difference declined significantly after the start compared with before. In primary healthcare, cases had 57% more healthcare contacts than expected before intervention and 23% more than expected 1 year afterwards. Concerning inpatient days in psychiatric healthcare, cases had almost 9 times more inpatient days than expected 1 year before intervention and 4 times more than expected 1 year afterwards (Table III).
|
Table III. Healthcare contacts, observed/expected values, 1 year after and 1 year before the rehabilitation programme |
|||
|
Type of contact |
1 year after Cases obs/ SMR/rate (95% CI) |
1 year before Cases obs/Cases exp SMR/rate (95% CI) |
1 year after+before Cases obs/Cases exp SMR/rate (95% CI) |
|
Outpatients |
|||
|
Somatic healthcare |
1.34 (1.21–1.48) |
1.34 (1.21–1.46) |
1.34 (1.25–1.43) |
|
Psychiatric healthcare |
1.70 (1.60–1.80) |
1.61 (1.51–1.70) |
1.65 (1.58–1.72) |
|
Primary healthcare |
1.23* (1.15–1.30) |
1.57 (1.49–1.65) |
1.40 (1.35–1.46) |
|
Total |
1.42* (1.36–1.47) |
1.54 (1.49–1.60) |
1.48 (1.44–1.52) |
|
Bed days |
|||
|
Somatic healthcare |
2.66* (2.19–3.12) |
0.51 (0.25–0.76) |
1.83 (1.53–2.13) |
|
Psychiatric healthcare |
4.09* (3.65–4.52) |
8.84 (8.28–9.40) |
6.79 (6.42–7.16) |
|
Total |
3.56* (3.24–3.89) |
7.05 (6.61–7.49) |
5.36 (5.08–5.64) |
|
*p < 0.05. CI: confidence interval; SMR: standard morbidity ratio; SMR/rate: ratio; obs: observed rate; exp: expected rate (controls). |
|||
DISCUSSION
No statistically significant reduction regarding any kind of sickness benefit or compensation after a nature-assisted rehabilitation programme for patients with mild to moderate psychological illness was found in this study. However, in patients who underwent the programme a significant reduction in healthcare consumption was evident the year after, especially concerning primary healthcare and inpatient days in psychiatric healthcare.
The intervention and control groups in this study were not exactly comparable. The former had far more healthcare contacts the year before the study start, indicating that this group experienced worse health than the matched controls. The reason for this imbalance involved difficulties in finding equally ill patients in the registers. There were also 8 cases with PTSD included in the intervention group, compared with none in the control group. PTSD might be regarded as a more severe stress-related disorder than the other diagnoses included in the F43 category.
Despite this imbalance, a significant reduction in clinically relevant variable healthcare consumption was found in the intervention group compared with controls. This could be interpreted as a favourable improvement in general health for the participants in the programme compared with the controls. Apart from this benefit, lower healthcare consumption is also associated with decreased costs for primary healthcare. The decreased healthcare consumption in the intervention group could be a result of either improved health or an improved capacity to cope with their long-lasting illness.
The findings in this study are in accordance with earlier studies on NAT (19). However, the specific intervention and/or outcome variables utilized in this study have not been subjected to any controlled or observational study of this kind before. Most rehabilitation programmes have not been successful regarding return to work as outcome variable, as described in the introduction.
This study has several limitations. First, the control group was not exactly comparable to the intervention group. Secondly, we lack data regarding type of sickness benefit. A change from normal sickness benefit to another form of support, when a person starts studying or participating in an internship at a workplace, could mean a great deal as regards return to work. Thirdly, the intervention programme was newly developed when inclusion in the programme started. It must be considered that there is normally a “learning curve” for this kind of intervention.
In conclusion, we found the programme to be beneficial to the participants in terms of decreased healthcare consumption. However, the proportion of ongoing sickness benefits was unchanged the year after participation in the programme. It was not possible to capture changes in type of sickness benefits in the available registers, which is a limitation of this study. We consider these findings important, and note that they need to be confirmed in a randomized controlled trial.
ACKNOWLEDGEMENTS
The authors would like to thank the participants in the programme and the staff at the Alnarp Rehabilitation Garden: Lena Welén-Andersson, Inga-Lena Bengtsson, Liselott Lindfors, Lillian Lavesson and Frederik Tauchnitz. We also thank Dr Thor Lithman and Dr Dennis Noreen for their invaluable statistical support.
The study was made possible by financial support from the Swedish Research Council Formas, the Skåne Region, and strategic funds from the Swedish University of Agricultural Sciences.
Conflicts of interest. Peter Währborg and Patrik Grahn are both shareholders in a research company that handles intellectual property rights: NAHC Holding AB, of which the Swedish University of Agricultural Sciences is the majority shareholder through its subsidiary SLU Holding AB. This company can further refine patents, etc., emerging from research studies.
REFERENCES
