Chia-Yu Hsu, MD1, Chu-Ming Wu, MD1, Shih-Wei Lin, MD2 and Kui-Lin Cheng, MD3
From the Departments of 1Physical Medicine and Rehabilitation, 2Orthopedic Surgery and 3Radiology, Ten-Chan General Hospital, Zhongli, Taiwan
OBJECTIVE: We report here a rare case of anterior superior iliac spine avulsion fracture that presented initially as meralgia paraesthetica.
CASE REPORT: A 14-year-old male sprinter presented with anterior superior iliac spine avulsion fracture, which was not observed on initial plain radiograph of the hip, but was diagnosed by ultrasound. Both clinical presentations and electrophysiological studies indicated meralgia paraesthetica. The lateral femoral cutaneous nerve of the thigh was probably compressed by an inguinal haematoma resulting from sartorius muscle strain, which was detected on musculoskeletal ultrasound. Computed tomography of the pelvis confirmed anterior superior iliac spine avulsion fracture.
CONCLUSION: Meralgia paraesthetica in adolescents can be due to anterior superior iliac spine avulsion fracture. Sonography is a valuable tool for screening for muscular haematoma and occult fractures, which may allow clinicians to diagnose the nature of the muscle injury, and thus guide the most appropriate therapeutic strategy.
Key words: anterior superior iliac spine; avulsion fracture; meralgia paraesthetica; musculoskeletal ultrasound; adolescence.
J Rehabil Med 2014; 46: 00–00
Correspondence address: Chia-Yu Hsu, Department of Physical Medicine and Rehabilitation, Ten-Chan General Hospital, No.155, Yanping Road, Zhongli City, Taoyuan County 320, Taiwan. E-mail: f927kimo@gmail.com
Accepted Aug 27, 2013; Epub ahead of print Oct 24, 2013
INTRODUCTION
Meralgia paraesthetica is an entrapment neuropathy of the lateral femoral cutaneous nerve, resulting in a painful, burning, numb sensation in a skin patch over the anterior and lateral thigh (1). Rare initial presentation of anterior superior iliac spine (ASIS) fracture as meralgia paraesthetica has been reported (2–4). We describe here an adolescent sprinter with an ASIS avulsion fracture presenting clinically as meralgia paraesthetica.
CASE REPORT
A 14-year-old boy presented to our clinic because of right anterolateral thigh numbness for 3 days. The patient had been well 3 days earlier, and symptoms of meralgia paraesthetica developed after a running competition at school. The initial X-ray scan of the right hip (anterior-posterior view), obtained immediately after the injury in the emergency department of a local hospital, was unremarkable (Fig. 1). Physical examination revealed mild tenderness around the ASIS and parasthesia over the right anterolateral thigh under sensory testing of light-touch and pin-prick. Straight leg raising was normal. No pain was noted during passive or active range of motion of his right hip joint. The patient was able to walk with little discomfort with a mild limping gait.
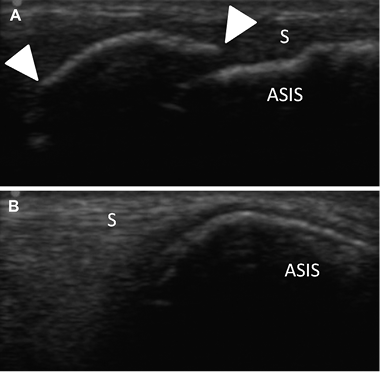
An ultrasound machine (MicroMaxx, SonoSite, FujiFilm, USA) with a 10-5 MHz linear-array transducer was utilized for scanning the right inguinal area. In transverse view, a mixed hyperechoic and hypoechoic haematoma was noted just medial and inferior to the tender area of the right ASIS and beneath the right internal and external oblique abdominal muscles. The haematoma, measuring 3.8 cm in diameter, had no internal increased vascularity (Fig. 2). Along the axis of the sartorius tendon, a separated bony fragment with minimal displacement was detected over the tender point of his right ASIS, measuring 1.6 cm (Fig. 3). Ultrasound indicated avulsion fracture of the ASIS and a muscular haematoma at the groin area.
Fig. 1. Initial X-ray of the right hip (anterior–posterior view), obtained immediately after the injury, was interpreted as normal.

Fig. 2. Ultrasonographic imaging using a transducer at the transverse plane of the abdominal muscles showed a mixed echoic haematoma (arrowheads) without internal increased vascularity, just medial and inferior to the right anterior superior iliac spine. E: external oblique abdominal muscle; I: internal oblique abdominal muscle.
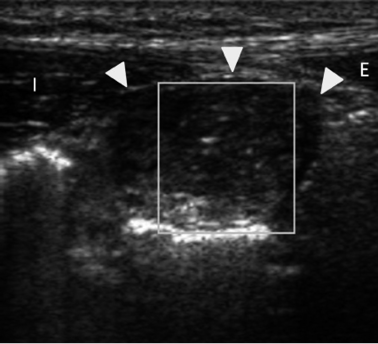
Fig. 3. Ultrasonographic imaging using a transducer along the axis of sartorius tendon showed (A) an abnormal bony fragment (arrowheads) at the lower part of right anterior superior iliac spine around the inguinal area, compared with (B) that of the left side. ASIS: anterior superior iliac spine; S: sartorius tendon.
The fracture was confirmed by a computed tomography (CT) scan without contrast medium. A bony fragment was seen in the inferior part of the right ASIS with minimal displacement in the axial (Fig. 4A) and coronal views (Fig. 4B). A possible haematoma with increased CT signals was detected 1 cm caudal to the axial plane of the fracture (Fig. 4C). Ten days after the injury, nerve conduction studies performed in both legs did not reveal any abnormality, except for the absence of sensory nerve action potential in the right lateral femoral cutaneous nerve of the thigh, which was compatible with the clinical presentation of meralgia paraesthetica (Table I).
Fig. 4. Computed tomography (A: axial view: B: coronal view) showed a bony fragment (arrowheads) at the inferior part of the anterior superior iliac spine with minimal displacement. (C) A possible haematoma (arrowheads) with increased computed tomography signals was detected 1 cm caudal to the axial plane of the fracture. ASIS: anterior superior iliac spine; I: iliacus muscle; P: psoas major muscle; S: sartorius muscle; T: tensor fascia lata muscle.

|
Table I. Nerve conduction studies evaluated 10 days after the injury |
||||
|
Site stimulated (recorded) |
Distal latency (ms) |
Amplitude (mV) |
Distance (mm) |
Conduction velocity (m/s) |
|
Motor nerve conduction velocity |
||||
|
Right peroneal nerve (EDB) |
||||
|
Ankle |
4.60 |
9.2 |
80 |
|
|
Lateral popliteal fossa |
13.35 |
8.8 |
420 |
48.0 |
|
Left peroneal nerve (EDB) |
||||
|
Ankle |
4.35 |
8.0 |
80 |
|
|
Lateral popliteal fossa |
12.65 |
7.2 |
420 |
50.6 |
|
Right tibial nerve (AHB) |
||||
|
Ankle |
3.75 |
20.0 |
80 |
|
|
Popliteal fossa |
13.30 |
13.4 |
440 |
46.1 |
|
Left tibial nerve (AHB) |
||||
|
Ankle |
4.45 |
18.4 |
80 |
|
|
Popliteal fossa |
14.05 |
12.2 |
440 |
45.8 |
|
Sensory nerve conduction velocity |
||||
|
Right sural nerve (posterior ankle) |
3.1 |
19.2 |
140 |
45.2 |
|
Left sural nerve (posterior ankle) |
3.1 |
16.2 |
140 |
45.2 |
|
Right superficial peroneal nerve (lateral ankle) |
3.5 |
12.2 |
140 |
40.0 |
|
Left superficial peroneal nerve (lateral ankle) |
3.5 |
9.1 |
140 |
40.0 |
|
Right lateral femoral cutaneous nerve of thigh (lateral thigh) |
No response |
|||
|
Left lateral femoral cutaneous nerve of thigh (lateral thigh) |
2.2 |
9.7 |
120 |
54.5 |
|
F wave (recorded), minimal latency (ms) |
||||
|
Right peroneal nerve (EDB) |
52.45 |
|||
|
Left peroneal nerve (EDB) |
51.65 |
|||
|
Right tibial nerve (AHB) |
50.70 |
|||
|
Right tibial nerve (AHB) |
51.65 |
|||
|
H-reflex, latency (ms) |
||||
|
Right tibial nerve |
31.00 |
4.1 |
||
|
Left tibial nerve |
31.40 |
3.2 |
||
|
EDB: extensor digitorum brevis; AHB: abductor hallucis brevis. |
||||
After the fracture was diagnosed, non-surgical 6-week conservative treatment was recommended by the orthopaedist. The patient was advised to undertake partial weight-bearing and range-of-motion exercises in the following weeks. Two months post-injury, the patient could return to normal activities with little discomfort.
DISCUSSION
The clinical presentation of meralgia paraesthetica in this case was a rare presentation of ASIS avulsion fracture. One cadaver study suggested that the lateral femoral cutaneous nerve is most susceptible to mechanical trauma located posterior, anterior, or medial to the ASIS; that is, at the origin of the sartorius and tensor fascia lata muscles (1). Although many cases of meralgia paraesthetica are due to entrapment of the inguinal ligament, other mechanisms, such as traction force resulting from bone grafting (5) or bony fragment (4) and haematoma or oedema irritation (2, 3), have been proposed. In the present case, the lateral femoral cutaneous nerve of the thigh was probably compressed by an inguinal haematoma due to strain on the sartorius muscle, which highlighted that the diagnosis was made using ultrasound.
Avulsion fracture of the ASIS is an uncommon pelvic apophyseal injury, typically occurring in adolescents after a sudden contraction of a muscle attached to the growing aphophyses (6). Depending on the muscle affected, this fracture can be categorized into sprinting (sartorius) type or swinging (tensor fascia lata) type, with the sprinting type accounting for most cases (7). Sports that result in this injury include soccer, athletics, gymnastics, tennis, fencing, basketball, and baseball (6, 7). A delay in treatment of the avulsion fracture of the ASIS can cause painful non-union, limited sports performance, and even long-term disability. Determining the timing of the injury is difficult, and diagnosis of the avulsion fracture may be missed in conventional plain X-ray scan of the pelvis (8). In the present case, if the CT had been carried out immediately after the injury, the fracture would have been diagnosed, which suggests that plain X-ray may not be sufficient for detecting occult apophyseal injuries. Conservative treatment in cases of minimal displacement show favourable outcomes (6, 9), while surgical intervention should be considered in cases of extensive displacement.
In conclusion, the clinical presentation of meralgia paraesthetica in adolescent athletes may be indicative of ASIS avulsion fracture. Sonography may help clinicians to screen for muscular haematoma and occult fractures, which may allow them to diagnose the nature of the muscle injury, thus guiding the most appropriate therapeutic strategy.
REFERENCES
