Wendy Boerboom, MSc1,2, Majanka H. Heijenbrok-Kal, PhD1,2, Ladbon Khajeh, MD3, Fop van Kooten, MD, PhD3 and Gerard M. Ribbers, MD, PhD1,2
From the 1Rijndam Rehabilitation Center, 2Department of Rehabilitation Medicine and 3Department of Neurology, Erasmus MC, University Medical Center Rotterdam, Rotterdam, The Netherlands
OBJECTIVES: To compare cognitive and emotional outcomes between patients with aneurysmal and perimesencephalic subarachnoid haemorrhage and norm scores.
DESIGN: First measurement in prospective cohort study.
Patients: Sixty-seven patients with subarachnoid haemorrhage, were divided into perimesencephalic (n = 8) and aneurysmal (n = 59) subarachnoid haemorrhage groups.
METHODS: Patients completed several questionnaires within the first year after haemorrhage. Depression was measured with the Center for Epidemiologic Studies Depression scale, fatigue with the Fatigue Severity Scale, and objective cognitive functioning with the Trail Making Test. Glasgow Coma Scale scores were collected at hospital admission.
RESULTS: Perimesencephalic patients had lower depression (p = 0.006) and lower fatigue scores (p = 0.029) and were faster on the Trail Making Test A (p = 0.002) than aneurysmal patients. No differences between the groups were found on Trail Making Test B (p = 0.112) and presence of fatigue (p = 0.105). Compared with norm scores, aneurysmal patients scored significantly worse on all outcomes, whereas perimesencephalic patients scored worse on Trail Making Test B (p < 0.008), fatigue (p = 0.073) and presence of fatigue (p = 0.058).
CONCLUSION: Perimesencephalic patients may experience problems in complex cognitive functioning and fatigue. In this respect, they have similar sequelae as aneurysmal patients, which may interfere with daily activities and social participation. These findings are of clinical relevance, as perimesencephalic patients often are discharged from hospital without long-term follow-up.
Key words: perimesencephalic subarachnoid haemorrhage; aneurysmal subarachnoid haemorrhage; cognition; fatigue.
J Rehabil Med 2013; 45: 00–00
Correspondence address: Wendy Boerboom, RoNeRes – Rotterdam Neurorehabilitation Research, Rijndam Rehabilitation Center and Erasmus MC, University Medical Center Rotterdam, PO Box 23181, NL-3001 KD Rotterdam, The Netherlands. E-mail: wboerboom@rijndam.nl
Accepted Jul 3, 2013; Epub ahead of print Oct 24, 2013

*This study has been presented as a poster presentation at the Ninth World Congress on Brain Injury of the International Brain Injury Association in Edinburgh, UK, 21–25 March 2012.
INTRODUCTION
Subarachnoid haemorrhage (SAH) is a subtype of stroke that occurs at a relatively young age. The mean age of onset of SAH is 55 years (1), compared with 70 years in men and 75 years in women for stroke in general (2). The overall case fatality rate is 50% in population-based studies. Only 5% of all strokes are SAH, with an incidence in the Netherlands of 5.8 per 100,000 persons per year for men and 9.9 for women (3, 4). In approximately 15% of all SAHs, no structural cause for the haemorrhage can be identified on radiographic imaging, termed angiogram-negative SAH, previously described as SAH of unknown origin or non-aneurysmal SAH (5–8). This group can be subdivided into perimesencephalic and non-perimesencephalic angiogram-negative SAH (9–13). This study focuses on 2 subtypes of SAH based on the cause of the haemorrhage: aneurysmal subarachnoid haemorrhage (A-SAH) and perimesencephalic subarachnoid haemorrhage (PM-SAH) (3). PM-SAH is defined as a haemorrhage restricted to the cisterns surrounding the brainstem and the suprasellar cistern combined with a negative angiogram (3, 7, 14). The cause of PM-SAH is unknown and no surgical treatment is required (3).
A-SAH covers 85% of all SAH and is characterized by the rupture of an intracranial aneurysm and the subsequent accumulation of blood in the subarachnoid space (3, 15). Neuroradiological intervention or neurosurgical clipping are the 2 options for treatment of the ruptured aneurysm (3, 15). PM-SAH accounts for 10% of all SAH cases and the remaining 5% has various other causes (3, 7). In 1985 van Gijn et al. (16) first described PM-SAH as a benign form of SAH.
Several studies have suggested that patients with A-SAH have a significantly less favourable prognosis than patients with PM-SAH, based on the need for surgical or endovascular treatment, risk of re-bleeding, shorter life expectancy and reduced quality of life (1, 5, 15, 17–22). Of the patients who survive, approximately one-third remain dependent (Rankin grade 3–5) (23). Even those who are independent may have cognitive impairments after recovery from A-SAH, in particular in the domains memory, executive functioning and language. Furthermore, half of the A-SAH patients experience mood disturbances and one-third experience fatigue (15, 21, 22, 24). Therefore, the majority of patients with A-SAH are referred to inpatient or outpatient rehabilitation services or nursing homes for follow-up treatment (25, 26).
Patients with PM-SAH have a shorter length of stay in hospital, and are considered to experience good recovery not requiring follow-up treatment or meeting the criteria for rehabilitation services (27). Most studies showing these results are focused on survival and clinical outcomes (10, 12, 13, 28, 29). However, the premise of good functional outcome and cognitive functioning of PM-SAH is unclear. Only 2 studies were found confined to cognition and psychosocial outcome in the subgroup of PM-SAH patients (18, 30). In these studies several problems are reported, such as cognitive deficits, depression, reduced activity levels, headaches, irritability and psychosocial problems, such as returning to a (current) job (18, 30, 31). However, in a long-term follow-up study in angiogram-negative SAH patients, problems in selective attention during the first year of follow-up were found, which normalized within 3 years (9). Two studies comparing the diverse group of SAH patients of unknown origin with selected A-SAH patients, reported impairments in diffuse cognitive functions, such as attention in the first group vs focal cognitive functions, such as short- and long-term memory, in the latter group (6, 8). Outcome studies comparing isolated PM-SAH and A-SAH are not available, to our knowledge.
The aim of this study was to investigate the differences in cognitive and emotional outcomes of the subgroup PM-SAH and A-SAH patients in the first year after SAH. Based on the literature, we expect that patients with PM-SAH will have better outcomes than those with A-SAH, but we also expect to find cognitive problems and mood disturbances in patients with PM-SAH that might require medical attention or follow-up treatment in rehabilitation services.
METHODS
Participants and procedures
All patients diagnosed with SAH, who were hospitalized between 2006 and 2009 at the neurology or neurosurgery department of the Erasmus University Medical Centre Rotterdam, were screened for participation in this study. Inclusion criteria were: at least 18 years of age and survival of SAH at least until hospital discharge. Exclusion criteria were: serious co-morbidity resulting in a short life expectancy less than 1 year and insufficient mastering of the Dutch language. Patients who agreed to participate were asked to sign an informed consent form. The study was approved by the medical ethics committee of Erasmus MC.
Data collection
The presence of SAH was determined by computed tomography (CT) or lumbar puncture. The cause of SAH was determined using CT angiography or digital subtraction angiography. PM-SAH was defined by accumulation of blood around the mesencephalon on CT and a normal 4-vessel angiogram (3, 14).
During hospitalization baseline socio-demographic data and clinical characteristics, such as type, location and severity of SAH, and type of rehabilitation (none, outpatient, or inpatient rehabilitation) were collected by the staff of the neurology or neurosurgery department. Within the first year after SAH a research psychologist visited the patients at home to collect different measurements, which included validated questionnaires for depression and fatigue, and an objective test for cognitive functioning. Data were collected by 3 trained research psychologists.
Normative data from healthy subjects were obtained from the literature for each of the questionnaires and for the cognitive functioning test (32–34).
Measurement instruments
The Barthel Index (BI) is used to evaluate the patient’s state of independence. The total score ranges from 0 to 20, where 0 is completely dependent and 20 is completely independent (35).
Glasgow Coma Scale scores (GCS) were collected as a measure of the severity of the SAH. The GCS is a scale to measure 3 different aspects of impaired consciousness and coma: motor response, verbal response and eye opening. The total score ranges from 3 to 15, of which the higher scores represent a higher level of consciousness (36). In this study the first GCS score during hospital admission was used. These scores were assessed by physicians of the hospital department.
The Center for Epidemiological Studies Depression scale (CES-D) was used to measure emotional outcome. CES-D is a 20-item scale used to measure depressive symptoms over the previous week in a general population. This scale is validated in stroke patients (37). Scores range from 0 to 60 and the higher the score, the more depressive symptoms are present. Scores of 16 or higher are an indication of presence of depression (32, 37, 38).
The Fatigue Severity Scale (FSS) was used to measure the severity of fatigue. The questionnaire has 9 statements on fatigue in daily life. The patient can score these statements on a 7-point Likert scale, ranging from 1 to 7, where 1 is “strongly disagree” and 7 is “strongly agree”. Based on the literature, patients with fatigue are distinguished from healthy controls if the mean score of the 9 items is 4 or higher (33).
The Trail Making Test (TMT), parts A and B, were used as a measure of cognitive functioning. The TMT is widely used and has been researched extensively. The TMT score is a neuropsychological measure that is sensitive to a wide range of neurocognitive deficits (39). The TMT is a pen and paper task to measure cognitive flexibility. In part A, which measures motor speed and processing speed, patients are asked to connect 25 numbered dots in ascending order as quickly as possible. In part B, which measures processing speed and divided attention, the 25 dots contain numbers and letters and the patient must connect the dots alternating between a number and a letter. The measured time (with a maximum of 180 s), including extra time for correcting potential errors, is recorded to calculate a time score (40).
Statistical analysis
Statistical analyses were performed using SPSS version 19 (SPSS Inc, Chicago, IL, USA). Descriptive statistics were used to describe the general population characteristics. Means and standard deviations (SDs) were calculated for interval variables and numbers and percentages for categorical variables. Mann-Whitney U tests were used to analyse the differences between patients with PM-SAH and those with A-SAH for the variables: GCS, CES-D and FSS and independent-samples t-test for the TMT A and B scores. Fisher’s exact tests were used to test the differences between the SAH types of the categorical variables: gender, education (≥ high school), hypertension, smoking presence of depression (CES-D > 16) and presence of fatigue (FSS > 4). Type of rehabilitation (inpatient/outpatient/none) was tested with the χ2 test.
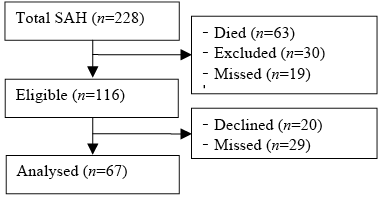
To test for potential selection bias, differences between the groups of missed patients and included patients (see Fig. 1) were evaluated. For all analyses a significance level of p < 0.05 was used.
Fig. 1. Patient inclusion. SAH: subarachnoid haemorrhage.
Comparisons of the PM-SAH and A-SAH group with norm values of healthy subjects were performed with independent-samples t-test and Fisher’s exact tests, using a statistical internet tool (GraphPad Software Inc, La Jolla, CA, USA).
RESULTS
Study population
From a total of 228 patients with SAH, who were hospitalized in the neurology or neurosurgery department of the Erasmus MC between April 2006 and August 2009, 67 were eligible for inclusion in the study. The flow of patients is shown in Fig. 1. Eight of the included patients had a PM-SAH (11.9%) and 59 had an A-SAH (88.1%). None of the patients in this sample was diagnosed with non-perimesencephalic angiogram-negative SAH. The mean age of the study population was 53.1 years (SD 11.6) and 37.3% were male. The mean length of hospital stay was 15.3 days (SD 9.9). Patient characteristics are presented in Table I.
|
Table I. Patient characteristics |
|||
|
|
Analysed group (n = 67) |
Missed group (n = 29) |
p-values |
|
Age, years, mean (SD) |
53.1 (11.6) |
56.4 (12.0) |
0.207a |
|
Length of hospital stay, days, mean (SD) |
15.3 (9.9) |
16.3 (9.0) |
0.645a |
|
GCS, mean (SD) |
13.2 (3.4) |
12.2 (4.0) |
0.425b |
|
Time after SAH, months, mean (SD) |
5.6 (8.6) |
NA |
NA |
|
Type of bleeding, perimesencephalic, n (%) |
8 (11.9) |
3 (10.3) |
1.000c |
|
Gender, men, n (%) |
25 (37.3) |
11 (37.9) |
1.000c |
|
Education, ≥ high school, n (%) |
32 (47.8) |
NA |
NA |
|
Hypertension, n (%) |
29 (43.9) |
NA |
NA |
|
Smoking, n (%) |
27 (40.9) |
NA |
NA |
|
at-test; bMann-Whitney U test; cFisher’s exact test. SAH: subarachnoid haemorrhage; GCS: Glasgow Coma Scale score; SD: standard deviation; NA: not available. |
|||
No significant differences were found between the groups of missed patients and included patients for any of the variables available: type of bleeding, gender, age, length of stay and Glasgow Coma Scale scores (Table I). Data were complete for 92.5% of the TMT-A, 89.6% of the TMT-B, 83.6% of the FSS and 77.6% of the CES-D. The main reason for the missing data was the length of the test battery: time restrictions or fatigue were reasons for not finishing the test battery. Sum scores could sometimes not be calculated because of missing item scores.
Comparison between PM-SAH and A-SAH patients
Compared with the A-SAH group, the PM-SAH group contained significantly more men and had a shorter length of stay (Table II). BI score, age and other patient characteristics did not differ significantly between the 2 groups. Rehabilitation type was also not significant. One PM-SAH patient received outpatient rehabilitation for cognitive complaints only. From the A-SAH patients 27.1% received inpatient rehabilitation including multidisciplinary functional and cognitive therapy. Table III presents the results of the questionnaires and cognitive testing. The PM-SAH patients had lower depression scores and fatigue scores compared with A-SAH patients. None of the PM-SAH patients had a significant depression (CES-D ≥ 16) vs 20 (44.4%) in the A-SAH group. However, the proportion of PM-SAH patients with fatigue (FSS score ≥ 4) was not significantly different from the A-SAH patients. For the tasks of cognitive functioning significant differences were found at the TMT-A. Patients with PM-SAH were faster on this task than those with A-SAH. No significant differences were found between the 2 groups on the more complex TMT-B task.
|
Table II. Comparison of patient characteristics between perimesencephalic subarachnoid haemorrhage (PM-SAH) and aneurysmal subarachnoid haemorrhage (A-SAH) patients |
|||
|
|
PM-SAH (n = 8) |
A-SAH (n = 59) |
PM-SAH vs A-SAH p-values |
|
Age, years, mean (SD) |
48.9 (10.4) |
53.6 (11.7) |
0.278a |
|
Time after SAH, months, mean (SD) |
3.2 (2.5) |
6.0 (9.1) |
0.390a |
|
Length of hospital stay, days, mean (SD) |
7.1 (6.6) |
16.4 (9.8) |
0.012a |
|
GCS, mean (SD) |
14.8 (0.5) |
13.0 (3.5) |
0.121b |
|
BI, mean (SD) |
19.9 (0.4) |
18.6 (2.9) |
0.051b |
|
Gender, men, n (%) |
6 (75.0) |
19 (32.2) |
0.045c |
|
Type of rehabilitation, n (%) Inpatient Outpatient None |
0 (0.0) 1 (12.5) 7 (87.5) |
16 (27.1) 7 (11.9) 36 (61.0) |
0.230d |
|
Education, ≥ high school, n (%) |
5 (62.5) |
27 (45.8) |
0.464c |
|
Hypertensiond, n (%) |
3 (37.5) |
26 (44.8) |
1.000c |
|
Smokingd, n (%) |
2 (25.0) |
25 (43.1) |
0.455c |
|
at-test; bMann-Whitney U test; cFisher’s exact test; dχ2 test. SAH: subarachnoid haemorrhage; GCS: Glasgow Coma Scale score; BI: Barthel Index score. |
|||
Comparison of PM-SAH vs norm values
Comparing the results with the scores of a normal healthy population we found that patients with A-SAH scored significantly worse on all outcome measures. Patients with PM-SAH scored significantly worse than the norm population on the more complex TMT-B task (Table III). In addition, the mean fatigue scores of the patients with PM-SAH and the proportion of these patients with a FSS score ≥ 4 were borderline significant compared with the healthy subjects. No significant differences were found for the depression scores and the TMT-A task.
|
Table III. Comparisons of outcomes between perimesencephalic subarachnoid haemorrhage (PM-SAH), aneurysmal subarachnoid haemorrhage (A-SAH) patients, and norm values |
|||||||||
|
Measurement |
PM-SAH |
n |
A-SAH |
n |
Norm values |
n |
PM-SAH vs A-SAH p-values |
PM-SAH vs norm p-values |
A-SAH vs norm p-values |
|
CES-D, mean (SD) |
5.0 (4.9) |
7 |
13.9 (8.7) |
45 |
8.2 (7.2) |
255 |
0.006b |
0.244a |
0.000a |
|
CES-D ≥ 16, n (%) |
0 (0.0) |
7 |
20 (44.4) |
45 |
32 (12.7) |
255 |
0.035c |
0.601c |
0.000c |
|
FSS, mean (SD) |
3.1 (1.6) |
8 |
4.5 (1.4) |
48 |
2.3 (0.7) |
20 |
0.029b |
0.073a |
0.000a |
|
FSS ≥ 4, n (%) |
3 (37.5) |
8 |
34 (70.8) |
48 |
1 (5.0) |
20 |
0.105c |
0.058c |
0.000c |
|
TMT-A, mean (SD) |
33.0 (8.3) |
7 |
47.9 (20.1) |
56 |
31.8 (9.9) |
41 |
0.002a |
0.764a |
0.000a |
|
TMT-B, mean (SD) |
87.0 (42.4) |
7 |
118.8 (49.1) |
56 |
63.8 (14) |
41 |
0.112a |
0.008a |
0.000a |
|
at-test; bMann-Whitney U test; cFisher’s exact test. CES-D: Center for Epidemiologic Studies-Depression Scale score; FSS: Fatigue Severity Scale score; TMT-A and TMT-B: Trail Making Test A and B scores; SD: standard deviation. |
|||||||||
DISCUSSION
Our results show disturbed cognitive and emotional outcomes in patients with PM-SAH, also found in other studies (18, 30, 31). The cognitive task, TMT-A, indicates that patients with PM-SAH have no problems in processing and motor speed, in contrast with patients with A-SAH, which is in agreement with our hypothesis. However, the results on the more complex TMT-B task indicate that both groups of SAH patients perform worse than a normative sample. This implies that divided attention is affected in both the PM-SAH and A-SAH patients. This confirms the findings of Madureira et al. (18), in which 72% of the patients with PM-SAH showed neuropsychological deficits, and Hütter et al. (6), who found similar cognitive deficits in non-A-SAH patients in comparison with A-SAH patients.
Another notable finding in our study is that the proportion of patients with PM-SAH with fatigue did not differ significantly from that of patients with A-SAH, and it almost significantly differed from the normative scores. To our knowledge, fatigue was not investigated in other studies with validated questionnaires in patients with PM-SAH. This finding suggests that patients with PM-SAH, like those with A-SAH, do experience fatigue, which is described as a common complaint after SAH (24).
Contrary to our expectations, none of the patients with PM-SAH in our study reached the CES-D cut-off score of 16, which indicates clinical depression. This finding differs from earlier literature in which, besides the cognitive deficits symptoms of depression in PM-SAH patients are also reported (9, 18, 30). A possible explanation is that, in our study, the majority of patients with PM-SAH was male. Gender is a known predictor for symptoms of depression, and could therefore have influenced the outcome of the CES-D (32). In the study of Madureira et al. (18), for example, 66% of the patients with PM-SAH with depression were female. Of the patients with A-SAH in our study, 44.4% had clinical depression (1, 15). The difference between A-SAH and PM-SAH might be explained by the different prospects of both groups. Patients with PM-SAH do not require surgical or radiological treatment and get an excellent clinical prognosis without the risk of a re-bleed and without follow-up treatment, whereas A-SAH patients are faced with complex treatment, high complication rates, a survival chance of only 50%, a high risk of recurrence and many of them face months of rehabilitation (1, 15).
Although the results of this study of impaired complex cognitive functioning and fatigue in patients with PM-SAH confirm previous research findings, not much has changed in terms of follow-up treatment for patients with PM-SAH in the Netherlands. Patients with PM-SAH often are discharged from hospital without long-term follow-up because of their good prognosis. Based on our results, this policy should be questioned.
This study has some limitations. The first is that there were only 8 PM-SAH and 59 A-SAH patients enrolled in the study. Even with this small number of PM-SAH patients we did find significant cognitive deficits compared with a normal population. In terms of percentage, this number fits the incidence of 10% of all SAH patients. In further research a larger sample is required to confirm that PM-SAH patients experience fatigue. Another limitation might be that the measurement time, within the first year after the haemorrhage, was not the same for all patients, and no follow-up measurements were done. In recent research it was found that cognitive complaints may diminish within 3 years of follow-up (9). Finally, cognitive testing was limited to the TMT test, which is a good test to measure processing speed and mental flexibility. In future studies other domains of cognitive functioning, such as long-term memory and sustained attention, should be measured in a larger sample over a longer follow-up.
In conclusion, contrary to the assumed favourable outcome, patients with PM-SAH may experience impaired complex cognitive functioning and fatigue. In this respect patients with PM-SAH have similar sequelae to those with A-SAH, which may interfere with daily activities and social participation. These findings are of clinical relevance, as patients with PM-SAH often are discharged from hospital without long-term follow-up. Based on our results this policy should be questioned.
AcknowledgEments
Financial support for this study was provided by: Johanna Kinderfonds (grant no 03.10.13-2003/0200) and Stichting BIO, The Netherlands.
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit on the authors or on any organization with which the authors are associated.
REFERENCES
