Anne-Christine Åhlander, MD, PhD1, Marika Persson, OT1 and Ingrid Emanuelson, MD, PhD2
From the 1Queen Silvia Children’s Hospital and 2Institution for Clinical Sciences, Department of Paediatrics, University of Gothenburg, Gothenburg, Sweden
OBJECTIVE: To describe the impaired fine-motor skills in patients with traumatic brain injury acquired in childhood.
DESIGN: A total of 165 patients with traumatic brain injury, aged 0–17 years, injured during the period 1987–1991, were identified. Fifteen years post-injury a questionnaire was sent to the patients. Twenty-six of the subjects had upper limb problems, 15 of whom agreed to participate and 12 attended an evaluation.
METHODS: The Sollerman test was administered. This test consists of 20 activities, of which 7 hand-grips were used (pulp-pinch, lateral pinch, tripod pinch, 5-finger pinch, diagonal, transverse and spherical volar grip). Each sub-test was scored from 0 to 4 points. Each task must be performed within 20 s. The maximum score was 80. Bimanual fine motor skills were classified by Bimanual Fine Motor Function (BFMF). BFMF consists of 5 levels of function of each hand. Level I is normal function, level II–V means subnormal function in an increasing grade. Co-ordination, spasticity, 2PD and stereognosis were also measured.
RESULTS: All patients had subnormal results on the Sollerman test. Fifty-eight percent had abnormal scores on the BFMF test.
CONCLUSION: The Sollerman test seemed to be reliable at picking up hand motor problems, as all subjects who reported such problems scored subnormally. This is in contrast to the BFMF test findings, where only 60% of our group scored subnormally.
Key words: long-term follow-up; upper limb function; traumatic brain injury.
J Rehabil Med 2013; 45: 815–819
Correspondence address: Ingrid Emanuelson, Habilitering och Hälsa, Näverlursgatan 38, SE-421 44 Västra Frölunda, Sweden. E-mail: ingrid.emanuelson@vgregion.se
Accepted June 4, 2013
Introduction
Children and adolescents who experience severe traumatic brain injury (TBI) comprise a group that requires not only medical resources in the acute phase, but also long-term rehabilitation because of remaining cognitive and motor deficits. There are some studies that have examined the long-term outcome in children with severe TBI, but they are few in number, have a short-term follow-up and do not always specify upper limb dysfunction. The Westmead Pediatric Multidisciplinary Outcome Study (1) is a prospective cohort study from a tertiary paediatric trauma centre in Australia, which followed 81 consecutive admissions (26 severe TBI, 41 mild TBI, 30 non-TBI controls) aged 0–14 years, 2 years after injury. Thirty-six percent of the severe subjects continued to have upper limb motor difficulties (muscle tone and arm/hand difficulties, poor handwriting, abnormal hand grasp, subnormal bilateral activity) (1). Mild TBI and control subjects had no or very few difficulties. Overall, half of the subjects in the severe TBI group had persistent fine motor difficulties at 2 years post-injury (1). In 2003, Kuhtz-Buschbeck (2) reported that hand motor skills had improved less than gait within 5 months of the injury. Functional motor function and control were affected 1–2 years after a TBI (2, 3) with reaction time and movement duration being prolonged. Co-ordination deficits were also frequent (2). In 2004 Gölge and co-workers (3) investigated recovery of precision grip in children after TBI. In this study 13 children, 5–14 years of age, with moderate to severe TBI were examined. The first date of examination was defined by Barthel index (part B > 20 points). Re-examinations followed after 1 and 5 months. Four different grips were measured. The children had deficits in force regulation, but weakness of the hand muscles did not seem to be a problem. This persisting physical disability in the severe TBI group is consistent with the findings of other researcher (4–7). The late outcome for children with severe TBI is thought to be dependent on the age at which the child was injured, so that those who experience TBI at an early age have more severe sequelae, compared with children who are older at the time of injury (3, 8). This study was initiated as the literature lacks descriptions of the long-term results with respect to fine-motor function.
This study was undertaken to clarify the complex pattern of impaired fine-motor skills in the long-term perspective in children with TBI. In the present study, patients have been followed for 15 years to determine their upper limb function after a moderate or severe TBI.
Material and Methods
Patients
A total of 165 survivors of moderate and severe TBI, aged between 0 and 17 years, injured during the period 1987–1991, were identified in the former south-west Sweden healthcare region, which has a population of 1.7 million. Inclusion criteria were the above-mentioned and documented moderate or severe brain injury: ≥1 h of unconsciousness and/or neurophysiological, neuroradiological or neurological signs of a brain contusion or haemorrhage. The exclusion criterion was a diagnosis of concussion. This population has previously been presented in an epidemiological study and a study of health-related quality of life (9, 10). The traceable individuals (149) were invited to take part in a follow-up investigation 10 years after injury. Twenty individuals did not reply, 16 did not want to participate, 2 had died and 2 had moved abroad. A total of 109 individuals answered a questionnaire on symptoms and health-related quality of life (10).
Of these 109, 29 had problems with upper limb function. A new questionnaire with questions about upper limb function was sent 15 years after the injury and 26 subjects agreed that they still had these problems and were invited to participate in a clinical investigation. All 26 belonged to the group of 29 who had replied at the 10-year follow-up, that they had upper limb problems. Fifteen agreed to attend an assessment and were called for an interview and a clinical examination. Twelve subjects (age range 16–32 years) (8 males, 4 females) finally attended the evaluation, and the examination of upper limb function was performed a mean of 15.11 years (standard deviation (SD) 1.44, range 14.19–16.03 years) after the injury. The 12 individuals who finally attended the evaluation did not differ significantly in terms of severity of injury from the 29 who originally stated that they had problems with upper limb function (Tables I and II).
|
Table I. Severity parameters at injury 15 years before follow-up for the 29 patients with upper limb dysfunction and the 12 who attended the investigation |
|||
|
Severity parameter |
Group n = 29 Mean (SD) |
Group n = 12 Mean (SD) |
p-value Mean (SD) |
|
GCS |
4.63 (2.69) |
5.88 (3.61) |
n.s. |
|
LOC, h |
230 (218.01) |
181 (148.25) |
n.s. |
|
Acute care, days |
29.65 (40.49) |
26.36 (23.16) |
n.s. |
|
Rehabilitation duration, days |
8.31 (144.85) |
59.08 (148.75) |
n.s. |
|
GOS |
4.41 (0.68) |
4.58 (0.67) |
n.s. |
|
SD: standard deviation; GCS: Glasgow Coma Scale: GOS: Glasgow Outcome Scale; LOC: Loss Of Consciousness; n.s.: not significant. |
|||
|
Table II. Demographic data for the examined group of 12 patients |
||||
|
Patient number |
Age at injury, years |
External cause |
Traffic category |
Sequelae at discharge from acute care |
|
1 |
10.9 |
Fall |
None |
|
|
2 |
15.2 |
Traffic |
Moped |
Motor + medical + behaviour |
|
3 |
15.7 |
Traffic |
Motor vehicle |
Motor + speech |
|
4 |
8.4 |
Traffic |
Pedestrian |
Motor |
|
5 |
8.5 |
Traffic |
Motor vehicle |
Motor + behaviour |
|
6 |
13.0 |
Traffic |
Motor vehicle |
None |
|
7 |
11.2 |
Traffic |
Pedestrian |
Motor + behaviour |
|
8 |
2.5 |
Traffic |
Motor vehicle |
Medical + motor + behaviour + cognive + speech |
|
9 |
0.3 |
Violence |
Motor + behaviour |
|
|
10 |
4.4 |
Traffic |
Cyclist |
Motor |
|
11 |
13.9 |
Traffic |
Cyclist |
Motor + cognitive |
|
12 |
17.0 |
Traffic |
Cyclist |
Motor + vision |
Identification of children
The children were identified primarily by the International Classification of Diseases (ICD)-9 diagnosis classification system and hospital death records, including the records from the forensic department. The study was approved by the ethics committee of the University of Gothenburg.
Measurements
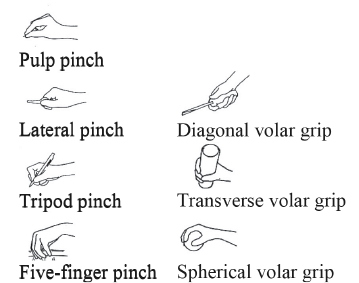
Hand function was evaluated using the standardized Sollerman hand function test (11). The test was developed for measuring hand function in healthy adult populations and has been used for tetraplegic individuals, for individuals with rheumatic illnesses and for those with chronic stroke (12). This test consists of 20 different activities of daily living (ADL), of which 7 main hand-grips are used to the same extent (pulp-pinch, lateral pinch, tripod pinch, 5-finger pinch, diagonal, transverse and spherical volar grip) (Fig. 1).
Fig. 1. The 7 grips in the Sollerman test.
Each subtest is scored by the examiner (according to the guidelines for scoring subtests) (11) on a 0–4-point scale. The ratings are based on the time and quality of performance of the hand-grip. Each of the tasks must be performed within 20 s to be given a score, giving a maximum score of 80, and the estimated time for performing the test was 20 min (according to the instructions given by the author). The subjects’ bimanual fine-motor skills were classified using the Bimanual Fine Motor Function (BFMF) classification system (13). BFMF consists of 5 levels describing the grade of function of the hands separately, and was developed for children with cerebral palsy (Table III). This is the first study describing the use of their classification in a TBI population. Levels II–V mean restrictions of functions in daily life.
|
Table III. Bimanual Fine Motor Function classification (BFMF) |
|
|
Level I |
One hand: manipulates without restrictions. The other hand: manipulates without restrictions or limitations in more advanced fine motor skills. |
|
Level II |
a) One hand: manipulates without restrictions. The other hand: only ability to grasp or hold. b) Both hands: limitations in more advanced fine motor skills. |
|
Level III |
a) One hand: manipulates without restrictions. The other hand: no functional ability. b) One hand: limitations in more advanced fine motor skills. The other hand: only ability to grasp or worse. |
|
Level IV |
a) Both hands: only ability to grasp. b) One hand: only ability to grasp. The other hand: only ability to hold or worse. |
|
Level V |
Both hands: only ability to hold or worse. |
Grip strength was measured with the Grippit instrument (AB Detektor, Göteborg, Sweden). The instrument estimates peak grip strength over a 10-s period, and sustained grip strength averaged across the 10 s. The instrument has been found to have good reliability in healthy adults (14, 15).
Tactile sensibility was measured by tactile gnosis and 2-point discrimination (2PD). Tactile gnosis was measured by the Shape-Texture Identification test (STI), where 6 standardized objects of different shape, texture and size should be identified with each hand in a bag without seeing the objects (16, 17). Two-point discrimination was tested for all fingers at a distance of 3–4 mm between the points, using the method developed by Moberg (18).
The clinical examination also included estimation of spasticity and co-ordination. Spasticity was measured using the modified Ashworth scale (19).
Procedure
The follow-up examination included an interview with the patients about problems in fine-motor skills in daily life, a clinical assessment using the Sollerman test, co-ordination (diadochokinesis, finger-nose and tremor) spasticity and tactile gnosis. The procedure was videotaped. A thorough review of the video film was carried out later and the raters also noticed problems during the test procedure. Both the dominant and the non-dominant hand were tested in all the tests.
The assessment was performed by an experienced paediatric neurologist and an occupational therapist. The whole procedure was performed in a quiet environment, in a hospital setting and took 3–4 h.
Statistical analysis
Data calculations were performed using Excel software and descriptive statistics only were used. For comparisons of injury groups, non-parametric statistical methods were used.
Results
The mean age of the patients at injury was 10 years, and they were evaluated between 14.19 and 16.03 years after the injury.
At the 10-year follow-up 27% (29/109) had hand motor problems and 5 years later, 24% (26/109) still had these problems. With regard to gross motor function all the patients were ambulatory without any technical aids.
All the patients had subnormal test results on the Sollerman test (maximum score 80 per hand). Eleven hands scored 71–79 (subnormal), and the remaining 13 hands scored below 71 (Table IV).
|
Table IV. Test results for fine-motor function in the upper limb in 12 patients with traumatic brain injury |
|||||||||
|
Patient number |
Sollerman total score |
Stereognosis |
2PD |
Grip strength |
BFMF level |
||||
|
R |
L |
R |
L |
R |
L |
R |
L |
||
|
1 |
75 |
74 |
n |
n |
n |
n |
n |
n |
1 |
|
2 |
55 |
71 |
n |
n |
n |
n |
A |
n |
2b |
|
3 |
40 |
48 |
n |
n |
A dig1–5 |
n |
A |
n |
3b |
|
4 |
74 |
69 |
n |
n |
A dig4,5 |
n |
n |
n |
2b |
|
5 |
70 |
66 |
n |
n |
n |
n |
n |
n |
2b |
|
6 |
79 |
72 |
n |
n |
n |
n |
n |
n |
1 |
|
7 |
69 |
10 |
n |
A |
n |
A dig1–5 |
n |
A |
3b |
|
8 |
59 |
74 |
n |
n |
n |
n |
A |
n |
2a |
|
9 |
73 |
33 |
n |
A |
A dig1–5 |
A dig3,5 |
A |
A |
3a |
|
10 |
70 |
70 |
n |
n |
n |
n |
n |
n |
1 |
|
11 |
78 |
71 |
n |
n |
A dig5 |
A dig3,5 |
n |
n |
1 |
|
12 |
76 |
70 |
n |
n |
A dig5 |
n |
n |
n |
1 |
|
BFMF: Bimanual Fine Motor Function (see Table III); dig: digits; A: abnormal; n: normal; R: right; L: left. |
|||||||||
Of the total of 240 rated items, 97 had a score of 3 out of 4. In as many as 38 items (39%) the subnormal score was due to more than 20 s being needed to perform the task (see methods). For a score of 3, either more than 20 s but less than 40 s were needed for performance, or the test was performed with some difficulty in the hand grip. The examiners (n = 2) noticed the need for repeated instructions, guidance during the test, impaired task performance and the need for pauses during the test.
On the BFMF test 7/12 patients (58%) had abnormal scores. Of these 7 patients, 5 had subnormal grip strength in 1 or both hands. Only 3 patients with IIIa or IIIb score for BFMF had increased muscle tone (Table IV); of these, 1 patient had undergone hand surgery. Patients scoring between 70 and 79 on the Sollerman test were classified as level I in the BFMF test.
During the clinical examination and when viewing the video of the Sollerman test we also noted that the patients had problems with co-ordination (8 patients), hand manipulation (8 patients), needed more than 20 min for performance (10 patients), needed repeated instructions (9 patients) and had impaired performance of task (9 patients) (Table V). All patients were able to complete the tests.
|
Table V. Results of the clinical assessment of co-ordination (dysmetria, ataxia and tremor), spasticity, in-hand manipulation, need for repeated instructions and performance of task |
||||||||
|
Pat.no |
Coordination |
Spasticity |
Manipulation |
Repeated performance |
Instruction about task |
|||
|
R |
L |
R |
L |
R |
L |
|||
|
1 |
A |
n |
n |
n |
n |
n |
A |
n |
|
2 |
n |
n |
n |
n |
n |
A |
n |
n |
|
3 |
A |
A |
A |
n |
A |
A |
A |
A |
|
4 |
n |
A |
n |
n |
A |
A |
A |
n |
|
5 |
A |
A |
n |
n |
A |
A |
A |
A |
|
6 |
n |
n |
n |
n |
n |
n |
A |
A |
|
7 |
n |
n |
n |
A |
n |
n |
A |
A |
|
8 |
A |
A |
n |
n |
A |
A |
A |
A |
|
9 |
n |
A |
n |
A |
n |
A |
A |
|
|
10 |
n |
A |
n |
n |
A |
n |
A |
A |
|
11 |
n |
n |
n |
n |
n |
A |
A |
A |
|
12 |
n |
A |
n |
n |
n |
n |
A |
A |
|
Pat.: patient; no; number: A: abnormal; n: normal; R: right; L: left. |
||||||||
The current life situation of the patients was distributed so that 7 patients were employed and, of the other 5, 3 attended school (2 in special school, 1 in mainstream school) and 2 had a disability pension. Five were married (4 had children), 4 lived alone (1 needed support in ADL activities) and the 3 who attended school lived with their parents.
Discussion
After a brain injury the outcome varies depending on the location and severity of injury and is unpredictable; thus it is difficult to develop specific tests for TBI, and there is no generally accepted standard test for the evaluation of upper limb function after a TBI. The tests used are the same as those used for other neurological dysfunctions. When reviewing the literature there is, to our knowledge, no earlier study using the Sollerman test and the BFMF test for evaluating the late effects on upper limb function after TBI.
The overall experience to be seems that the Sollerman test is relatively reliable at picking up hand motor problems relevant to activities of daily living in the studied group, as all those who subjectively reported such problems scored subnormally. This is in contrast to the findings in the BFMF test, in which 60% scored subnormally. In the clinical tests of co-ordination 8/12 had such problems, in contrast to the assessment of 2PD and tactile gnosis.
The Sollerman test is sensitive enough to capture the hand function problems related to speed and performance of grasp, but does not describe the reason for the problem. Upper limb tempo was a problem for 10/12 patients. This is in concordance with the findings presented by Chaplin and co-workers (20), who evaluated 14 patients 16 months or later after injury with the Bruininks-Oseretsky Test of Motor Proficiency (BOTMP), and described that upper limb tempo and dexterity were significantly lower than the other fine-motor subtests in the BOTMP.
The BFMF test is designed for the classification of upper limb dysfunction in patients with cerebral palsy (13). The advantage of using this test is that it describes the hands separately, is easy to perform and takes only a short time to administer; however, this test does not identify all those with scores between 70 and 79 on the Sollerman test.
Despite a duration of 15 years post-injury, the limitations of upper limb function remained in 24% of the patients, according to the questionnaires, and we have no reason to believe that the group not examined had recovered with regard to hand function during the follow-up time.
Our study also highlights that patients with TBI have persistent upper limb functional limitations, implying a need for tests which could be used to assess all patients. As these limitations interfere with activities of daily living there is a constant need for support. In the literature descriptions of upper limb dysfunction after TBI are sparse, and those that exist have short follow-up times. In this respect our study emphasizes the role of an individualized, non-structured evaluation. This study highlights the need for both qualitative and quantitative tests to be able to administer adequate support and rehabilitation for these patients.
The limitation of this study is the small number of clinically evaluated patients. This is a part of a larger population-based long-term follow-up study, in which the drop-out rate was 50% for those with anamnestic upper limb problems in the 15-year follow-up group (n = 26). The drop-outs (n = 14) did not differ from the evaluated group (n = 12) in terms of severity of injury (Tables I and II). The group has been followed by a team that has had the same principal investigator for 15 years (IE).
Of the 26 patients in the group, we examined only 12, partly because of memory problems among the patients approached (i.e. they forgot the time of appointments). There were originally 29/109 (27%) with upper limb problems at the 10-year follow-up of children with TBI (8), and in this 15-year follow-up there were 26/109 (24%) according to questionnaire ratings by the patients. In this study the exact nature of the upper limb problems were assessed only on a single occasion, which did not reveal the natural history of these complaints. Furthermore, it is sometimes impossible to discriminate what is the limitation of performance of hand function and what is due to cognitive and perceptual difficulties.
References
