Samuel Carlsson, MD1 and Jean-Luc af Geijerstam, MD, PhD2
From the 1Department of Medicine Västerås Hospital, Västerås and 2Clinical Epidemiology Unit, Karolinska University Hospital, Stockholm, Sweden
OBJECTIVE: A study published in 2000 on the acute clinical management of mild traumatic brain injuries in Sweden showed that these patients were routinely admitted to hospital for observation. This study aims to compare current clinical management of mild traumatic brain injury with clinical practice a decade ago.
DESIGN: Questionnaire to senior residents in all emergency departments in Sweden and data from registers covering all in-hospital care in Sweden.
RESULTS: The response rate to the questionnaire was 100%. In Sweden, 71 emergency departments treat patients with mild traumatic brain injuries. An estimated mean of 58% of patients with mild traumatic brain injuries receive computerized tomography scanning, which represents a 3-fold increase compared with 2000. In 2010, Swedish hospitals admitted 8,821 patients for mild traumatic brain injuries (94 per 100,000 inhabitants). This figure is approximately half that of 1996, when 16,877 patients were treated as inpatients for mild traumatic brain injuries (191 per 100,000 inhabitants). However, admission rates continue to vary widely among departments. The mean hospital stay 2010 was 1.21 days, compared with 1.6 days in 1996.
CONCLUSION: This study provides evidence of a change in clinical practice in the acute management of mild traumatic brain injuries in Sweden. Acute management is increasingly based on computed tomography, and in-hospital observation is used less frequently as a strategy for these patients.
Key words: mild traumatic brain injury; computed tomography; clinical management; in-hospital observation; incidence; admission rate.
J Rehabil Med 2013; 45: 718–720
Correspondence address: Jean-Luc af Geijerstam, Clinical Epidemiology Unit, Karolinska University Hospital, SE-171 76 Stockholm, Sweden. E-mail: jean-luc.af.geijerstam@ki.se
Accepted June 4, 2013
Introduction
Worldwide, between 100 and 300/100,000 adult patients per year are treated in hospital for mild traumatic brain injury (MTBI) (1). There are numerous definitions of MTBI, a commonly used one was proposed by the American Congress of Rehabilitation Medicine (2). Most patients with MTBI will recover completely, but some will develop long-term, non-neurosurgical sequelae (3). A few patients will develop serious intracranial complications requiring neurosurgical intervention in the acute phase (4). The aim of any acute management strategy must be to identify accurately, and at reasonable cost, those at risk for deterioration requiring neurosurgical intervention.
In 2000, we published a study on the clinical management of MTBI in Sweden, which drew a clear conclusion; patients with MTBI were routinely admitted to hospital for observation (5). MTBI was commonly defined as patients sustaining a head trauma with “a history of amnesia or loss of consciousness”. Annually, approximately 200/100,000 patients were treated as inpatients for MTBI. All emergency departments (EDs) had access to a 24-h computed tomography (CT) scanner service. No clinics reported using CT to triage patients for admission. Subsequent systematic reviews of the literature showed that using CT to decide who required admission was both a safe and a cost-effective acute management strategy for MTBI compared with a strategy based on in-hospital observation (6). Between 2000 and 2004, a nationwide pragmatic randomized controlled trial (RCT) was also conducted in Sweden to compare the two management strategies. More than half of all Swedish emergency departments participated in the trial. The results provided solid evidence supporting the CT triage strategy (7, 8).
The aims of the present study were to describe current clinical management of MTBI and compare these results with those from our previous study, in order to determine whether management has changed in light of new evidence.
Methods
In June/July 2009 we surveyed all emergency departments in Sweden’s 80 hospitals, asking questions about clinical routines for MTBI (e.g. indications for in-hospital observation, and estimated use of CT). A self-completion postal questionnaire was posted to the senior resident in all the hospitals’ emergency departments. The questionnaire used in this study was identical to the one used in our previous study, in order to facilitate comparing the results from the two surveys (5).
Epidemiological data on in-hospital care (number of admissions and length-of-stay) were obtained from the Swedish National Board of Health and Welfare (NBHW) (website: http://www.socialstyrelsen.se/english). All healthcare in Sweden is publicly funded, and the NBHW collects data on all in-hospital care in the country. Data in the NBHW register have high validity (9). The present study includes data from 1990 through 2010 on all patients with a discharge diagnosis of commotio cerebri (International Classification of Diseases (ICD)-9 code 850/ICD-10 S06.0). We chose to include data up until 2010, since this was the latest available year for data-capture at the time of analysis and preparation of the manuscript.
Results
Characteristics of hospitals treating patients with mild traumatic brain injuries
A total of 80 emergency departments were sent the questionnaire. Non-responders were contacted by post with an additional questionnaire. The few remaining non-responders were contacted by phone or fax. The final response rate was 94%. The 5 clinics that did not submit questionnaires were contacted by phone. All confirmed that they did not accept patients with MTBI, thus the response rate from clinics relevant to this study was 100%.
Seventy-one emergency departments in Sweden accept patients with MTBI. Four of these are specialized paediatric emergency departments, all at university hospitals.
All 71 emergency departments reported having access to a 24-h computerized tomography scanner service. Only 6 clinics reported any restrictions regarding availability; either that the radiologist on call was at home during the night or that qualified neuroradiological interpretation could not be assured during the night.
Evaluation in the emergency department
The basic structure for evaluating MTBI patients in the emergency department is largely unchanged; general surgeons most commonly evaluate patients with MTBI (86%), and most hospitals report treating children with MTBI (86%).
Changes are obvious in two areas: (i) 60% of the hospitals report having written guidelines for MTBI management compared with 32% in our previous study; and (ii) 40% now give written instructions to patients at discharge, whereas only 4% reported doing so in 1998.
Admission for in-hospital observation
Most routines (i.e. where patients are observed, frequency of assessment during the observation period, what is being observed) regarding the in-hospital observation period are reportedly unchanged since 1998. One obvious change is that, in 1998, most clinics reporting a fixed minimum time for in-hospital observation stated that it was 24 h, whereas today the most common minimum time is 12 h. Although the Reaction Level Scale (RLS) remains the dominant scale to evaluate consciousness, utilization of the Glasgow Coma Scale (GCS) has more than doubled.
Radiological imaging
The predominant indications for ordering a CT scan in patients with MTBI were basically unchanged. CT is used for between 5% and 100% of patients with MTBI, with a mean value of 58%. This represents nearly a 3-fold increase in the use of CT compared with 1998, when CT was used for between 2% and 80% of patients, with a mean value of 22%. Fig. 1 shows the estimates for 2009 compared with 1998.
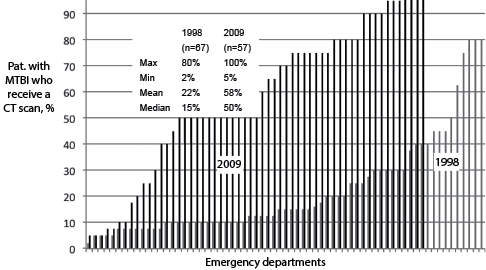
Fig. 1. Estimated use (by the senior resident) of computerized tomography (CT) scanning for patients with mild traumatic brain injury (MTBI) in emergency departments in Sweden, in 1998 (grey) and 2009 (black) (responses were missing from 8 departments in 1998 and 14 in 2009).
As in 1998, no hospitals perform routine skull radiography in the work-up of MTBI patients.
Epidemiological data and resource consumption
In our previous study we could observe a relatively stable yearly incidence of MTBI patients admitted to hospital for the decade leading up to our study (1987–1996). This stability in incidence suggested a consistency in clinical policy in MTBI management in Sweden throughout the period. This has clearly changed. Fig. 2 shows the yearly incidence of MTBI patients admitted to hospital from 1990 to 2010. In 2010, 8,821 patients were admitted to hospital for MTBI (94 per 100,000 inhabitants). This represents approximately a 50% reduction in admissions for MTBI compared with 1996, when 16,877 patients were treated as inpatients (191 per 100,000 inhabitants). No apparent change in the age and sex distribution was noted in this cohort compared with previous years. In 1998 the mean hospital stay for patients with MTBI was 1.6 days, while in 2010 it was 1.2 days. As in 1998, the admission rates continue to vary widely among departments.
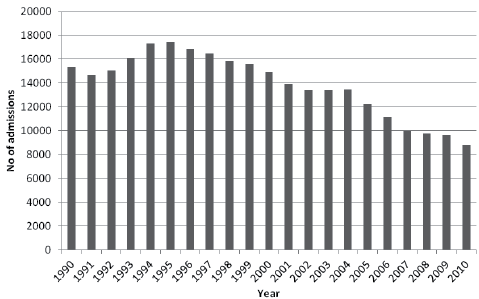
Fig. 2. Number of patients admitted to hospital for mild traumatic brain injury in Sweden, 1990–2010.
Discussion
Our results show several changes in the acute management of MTBI patients in Sweden, compared with our earlier study. Fewer patients are admitted for in-hospital observation, and the mean hospital stay is shorter than previously. The reported fixed minimum time for observation is shorter, a larger proportion of clinics have written guidelines for MTBI care, and patients are more frequently given written instructions at discharge. The estimated use of CT in MTBI shows nearly a 3-fold increase.
All of these changes indicate that CT is being used as a screening tool for admission. Annually, however, many patients are still being admitted after MTBI. It is possible that a number of those patients are both being admitted and receive a CT. Such clinical practice represents unnecessary resource utilization (8). If CT findings are normal, and there are no other reasons for admission, most patients with MTBI can be discharged early without an in-hospital observation period. A large, pragmatic RCT in Sweden, where almost 90% of MTBI patients were discharged early, showed the feasibility of such a practice (7). Similar trends regarding MTBI incidence and CT use have been observed recently in other Nordic countries (10, 11). In general, most current guidelines on MTBI management include CT scanning in the acute phase (12, 13).
Why have we not observed an even more drastic change in the clinical management of MTBI? One simple reason is that clinical practice is often difficult to change, and when such changes occur they tend to take a long time (14). The routine of observation after MTBI has been used in Sweden for many decades, and staff in the emergency departments have all been trained and accustomed to such a practice. Another possible reason could be the lack of incentive to change. If beds for in-hospital observation are not in short supply, then new routines for MTBI might not seem particularly appealing. Another reason might be purely administrative; many emergency departments in Sweden have adopted patient flow processes to reduce patients’ waiting time to see a physician and the overall length of stay in the ED (15). Hence, MTBI patients in some hospitals are “admitted” to a short-stay ward adjacent to the ED while awaiting CT. Such a practice will result in an entry in the in-hospital register for MTBI and, falsely, in our study be interpreted as management by observation strategy when in fact CT triage is being used (16). The number of cases reported in this manner is unclear.
An obvious weakness of our study concerns the questionnaire design, which is an indirect measure of clinical management. However, coupled with the analysis of epidemiological data, we believe that our main conclusions in this paper are valid. Further analyses of MTBI management should focus on aspects such as exploring barriers to change and the reasons for wide variations in admission rates between clinics. Furthermore, acute strategies for selecting patients for CT need to be further developed and validated as regards long-term functional outcomes and costs (13).
This study provides evidence of a change in clinical practice in the acute management of MTBI in Sweden over a 10-year period. Acute management is increasingly becoming CT based, and in-hospital observation is being used less frequently as a strategy for these patients.
Acknowledgements
The study received support from the Swedish Council on Health Technology Assessment. The authors declare that they have no conflicts of interest.
References
