Jerry Larsson, MSc1, Ann Björkdahl, PhD1,2, Eva Esbjörnsson, PhD1 and Katharina S. Sunnerhagen, MD, PhD1,3
From the 1Rehabilitation Medicine, Institute of Neuroscience and Physiology, University of Gothenburg, 2Ersta Sköndal University College, Gothenburg, Sweden and 3Sunaas Rehabilitation Hospital, The Medical Faculty, Oslo University, Oslo, Norway
OBJECTIVE: The aim of this work was to explore the extent to which social, cognitive, emotional and physical aspects influence participation after a traumatic brain injury (TBI).
Design/subjects: An explorative study of the patient perspective of participation 4 years after TBI. The cohort consisted of all patients (age range 18–65 years), presenting in 1999–2000, admitted to the hospital (n = 129). Sixty-three patients responded; 46 males and 17 females, mean age 41 (range 19–60) years.
METHODS: Four years after the injury, the European Brain Injury Questionnaire (EBIQ), EuroQol-5D, Swedish Stroke Register Questionnaire and Impact on Participation and Autonomy (IPA) questionnaire were sent to the sample. Data were analysed with logistic regression.
RESULTS: On the EBIQ, 40% of the sample reported problems in most questions. According to IPA, between 20% and 40% did not perceive that they had a good participation. The analyses gave 5 predictors reflecting emotional and social aspects, which could explain up to 70% of the variation in participation.
CONCLUSION: It is not easy to find single predictors, as there seems to be a close interaction between several aspects. Motor deficits appear to have smaller significance for participation in this late state, while emotional and social factors play a major role.
Key words: social participation; brain injury; depression; self-centring; cognitive.
J Rehabil Med 2013; 45: 802–807
Correspondence address: Jerry Larsson, Rehabilitation Medicine, Institute of Neuroscience and Physiology, University of Gothenburg, Gothenburg, Sweden. E-mail: jerry.larsson@vgregion.se
Accepted April 29, 2013
INTRODUCTION
Traumatic brain injury (TBI) is a significant problem worldwide, which has an impact not only on the person, but on society as well. The incidence of TBI is approximately 400/100,000 inhabitants, and the number of disability cases as a result of TBI was estimated in 1996 at approximately 5.3 million in the USA and 6.2 million in Europe (1, 2).
Participation is a core in all models of disability according to the World Health Organization (WHO) and International Classification of Functioning, Disability and Health (ICF) (3). There is also a general consensus that the goal of rehabilitation after TBI is to achieve good participation in society. According to Cicerone, measuring participation as an outcome of rehabilitation is the most meaningful way to measure outcome, but it is probably also the most challenging method, since there are many things that contribute to a person’s level of participation (4). “Participation” is defined in the ICF as “involvement in a life situation”. The opposite of participation, “restrictions to participation”, is defined as “problems an individual may experience in involvement in life situations” (3).
Persons with TBI often experience limitations in their participation. In a study of 160 persons, Wiese et al. showed that 81% with moderate and severe TBI had not returned to pre-injury levels of leisure participation 1 year after the injury (5). Their activity had changed from being engaged in partying, drug and alcohol use and sports to watching television. It appears that a large number of individuals with TBI will experience changed and reduced leisure participation over extended periods (6, 7). In a longitudinal study from Taiwan, it was reported that patients still had difficulties with social interactions and family relationships 6 years after TBI, even though they could live and work independently (8).
It is important to consider factors other than the direct consequences of the trauma that can also influence participation. For example, in another study in this group, it was noted that it is necessary to consider pre-morbid factors in the rehabilitation (9). Of those who were on sick leave on the day of occurrence of the trauma, 80% were still on sick leave 4 years after the trauma, compared with 40% of those who were not on sick leave on the day of the trauma.
Depression is common after all forms and severities of TBI (10). The prevalence of depression in the TBI group is thought to be more than 50% and, specifically, the patient with a pre-morbid poorer psychosocial functioning and greater psychiatric distress is more prone to secondary depression after TBI (11).
Much is still unknown about the factors involved in the ability to participate in society after TBI, and it is important to gain better knowledge about the influence of different factors, such as somatic, emotional, cognitive and environmental factors.
The aim of this work was to explore the extent to which the social, cognitive, emotional and physical aspects influence participation after a TBI, according to the individual’s subjective experience.
MATERIAL AND METHODS
Participants
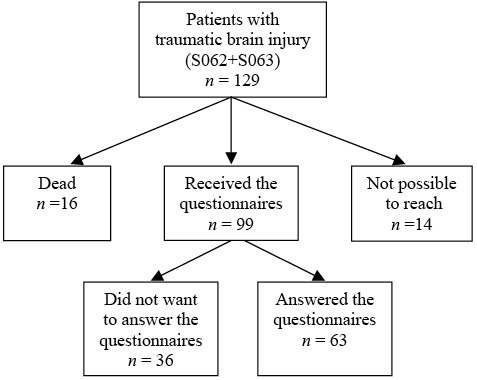
The study was carried out at Sahlgrenska University Hospital, Gothenburg, Sweden, which has a catchment area of approximately 900,000 inhabitants. The cohort was made up of all patients with a TBI classified as S06.2 and S06.3 according to International Classification of Diseases – 10th revision (ICD-10) (n = 129) (excluding the mild injuries that are often diagnosed as commotio S06.0). The persons included in the study were between 18 and 65 years of age and admitted to the emergency room at the hospital during a two-year period (1999–2000). A survey was sent to the participants that could be reached (n = 99). A flow-chart for the study inclusion is shown in Fig. 1.
Fig. 1. Study recruitment.
The ethics committee of the University of Gothenburg approved the study.
Procedure and instruments
Four years after the injury a letter was sent to each patient at home, asking them to complete 4 questionnaires: EuroQol-5D (EQ-5D), a self-report of health-related quality of life, consisting of 5 domains (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) (12), to which is added a visual analogue scale (VAS) for evaluation of perceived health-related quality of life, where 0 = worst imaginable health status and 100 = best imaginable health status; the European Brain Injury Questionnaire (EBIQ), a self-report measure for persons who are brain injured, that measures the subjective experience of cognitive, emotional and social difficulties (13); the Impact on Participation and Autonomy Questionnaire (IPA) (14), a questionnaire with 39 items measuring participation in accordance with the definition set out in the ICF; and a questionnaire from the Swedish Stroke Register (http://www.riks-stroke.org/index.php?content=form) concerning living conditions, activities of daily living and support (modified so that the questions started with “since your brain injury…”). Demographic data and severity of the trauma, according to the Reaction Level Scale (RLS) (15), were gathered from medical charts. The RLS score was converted to the Glasgow Coma Scale (GCS), which is presented here (16).
Data analysis
As most data were ordinal, non-parametric statistics were used and the logistic regression was chosen as suitable for this kind of data. The level of significance was set to p = 0.05. Statistical analysis was carried out with the SPSS, Version 20 (SPSS Inc., Chicago, IL, USA).
Descriptive data are presented for gender, age, cause and severity of the trauma and GCS. The EQ-5D’s 5 domains and the EBIQ were used to describe the sample and the experience of difficulties after the injury. The percentage of the sample indicating problems according to single items in EBIQ is presented.
The IPA was used to describe the experience of participation in society. The analysis included 4 domains from IPA (autonomy indoors, family role, autonomy outdoors and social life/relationship). The response options were 0 = very good, 1 = good, 2 = fair, 3 = poor and 4 = very poor. In the analyses, the data were dichotomized into good (0–1) and not so good participation (2–4). The activities and participation factors of the IPA are fundamental and important for life, and therefore the answer “fair” was also interpreted as not so good participation.
To identify what factors influence participation in society, items that were considered relevant for participation in the different IPA domains were chosen and logistic regressions were carried out between these items and each of the IPA domains. Items reflected social, cognitive and emotional aspects (EBIQ) as well as aspects of mobility (EQ-5D) and dependence in “Daily hygiene”. Due to the correlations between the different EBIQ domains (risk for multicollinearity) being too high it was impossible to use the EBIQ domains for the regression analysis, and therefore single questions without a high inter-correlation were selected instead. This was examined by correlation analysis (Spearman’s), where questions with correlations below 0.40 were selected. After this selection 15 items remained. However, there was no item representing communication, which was considered important, and therefore 3 items on communication were added, resulting in 18 items. Because of the sample size in the study a maximum of 5 factors in each logistic regression was considered feasible. To reduce the number of items for each regression with the different IPA domains, 5 relevant factors were selected according to clinical experience and relevance for the domain. For the selection of relevant factors to the regression model, we decided to rely on clinical experience and theoretical knowledge, rather than using mathematics. For the domain of social life we valued contact with others, dependence and initiative as important aspects and thereby chose these items for the model. For the domain “family role” we valued dependence, communication and cognitive aspects as important. Autonomy outdoors was expected to be related to dependence, social and cognitive aspects. For the domain “Autonomy indoors” we valued dependence and close relations with family and caregivers to influence the possibility of participation.
Finally, the items included in the different regressions were; “difficulty communicating what you want to say”, “leaving others to take the initiative in conversations”, “losing contact with your friends” (social aspects), “trouble concentrating”, “feeling unable to get things done”, “failing to notice other people’s mood” (cognitive aspects), “others do not understand your problems”, lack of interest in your surroundings”, “thinking only of yourself” (emotional aspects), “mobility” (EQ-5D), “daily hygiene” (Swedish Stroke register). To explore whether gender, age and severity of injury would improve the models, these variables were added in the regression, but, as they did not have a positive effect, the original model was chosen to decrease the number of variables in the model. For the degree of variance explained in the logistic regression the Cox & Snell (17) and Nagelkerke (18) were used, and reported as an interval.
RESULTS
Sixty-three out of the 99 subjects who received the survey responded (Fig. 1) (46 males and 17 females). At the time of the injury the mean age was 41 years (standard deviation (SD) 12, age range 19–60 years), and 21% were under 30 years, 33% between 31 and 40 years, 18% between 41 and 50 years, and 28% over the age of 50 years. According to the GCS, 16% were classified as mild, 54% as moderate, and 30% as severe brain injury. The drop-out from the original sample of 129 persons consisted of 16 subjects who were not longer alive, 14 who could not be reached, and 36 who did not respond or who declined to participate in the study. There were no significant differences between the group of responders and the drop-outs.
At the follow-up 4 years after trauma 52% of the sample was employed full- or part-time. Ninety-seven percent lived in their own homes, 3% lived in group homes, and 30% lived in one-person households. A large proportion of the sample reported that they had functional disabilities. On the EQ-5D, 25% of the group stated that they had problems (some or severe problems) with mobility. Fifteen percent had problems with self-care, 33% with usual activities, 58% with pain, and 58% with anxiety/depression. On the EQ-5D VAS scale, the group stated their health as a mean of 68 of a best possible 100, which, compared with a Swedish control group (mean = 82) this is under the 25th percentile.
The results of the EBIQ on single questions showed that 40% of the sample stated having problems in as much as 43 of the 62 questions, and 60% reported problems on 8 single questions of the EBIQ (Fig. 2).
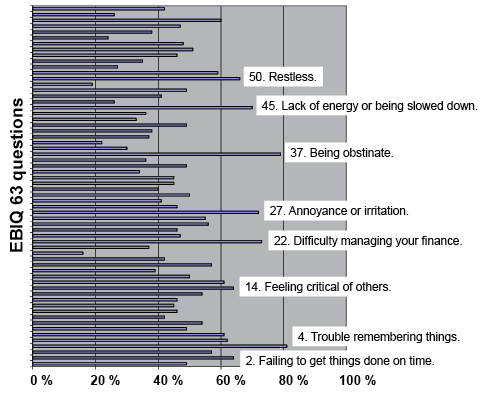
Fig. 2. Percentage of the sample that rated problems on each of the 63 European Brain Injury Questionnaire (EBIQ) items. Those items for which more than 60% of the sample indicated problems are highlighted.
The IPA questionnaire, impact for participation and autonomy, showed that 40% of subjects did not experience any good participation in the domain of “autonomy outdoors”, and this was also the opinion of 36% in the domain of “social life and relationship”. Dissatisfaction was also expressed in the other domains, such as 34% regarding “family role” and 21% in “autonomy indoors”. The domain “work and education” was not relevant for the majority (81% did not work or study), and this domain was thus excluded from the analysis.
Logistic regression analysis between selected items reflecting social, cognitive and emotional aspects, mobility and dependence and the different domains of the IPA was used to examine factors that had an influence on participation in society. The models for the different domains were retrieved by separate processes, as explained in the methods section, and the contents were found to differ between the domains (Tables I–IV). The goodness-of-fit for the models were good according to the Hosmer and Lemeshow Test (19). Poor fit in this test is indicated by a significance value less than 0.05 and the significance values in our models were 0.574 for social life, 0.533 for family role, 0.938 for outdoor, and 0.634 for indoors participation. From the logistic regressions 5 significant predictors were retrieved that reflected emotional and social aspects (Tables I–IV). In none of the regression analyses, were mobility or dependency in daily hygiene significantly predictive of the experience of participation.
|
Table I. Logistic regression model for participation in the domain of “social life”(IPA), with single items of European Brain Injury Questionnaire (EBIQ) from the domains motivation and communication, the ability to perform daily hygiene (Swedish Stroke Register Questionnaire) and mobility (EuroQol (EQ-5D)) |
|||
|
p-value |
Odds ratio |
95% CI for odds ratio |
|
|
Feeling unable to get things done EBIQ 26 |
0.079 |
4.276 |
0.847–21.600 |
|
Lack of interest in your surroundings EBIQ 38 |
0.042* |
10.431 |
1.090–99.839 |
|
Losing contact with your friends EBIQ 60 |
0.004** |
16.215 |
2.449–107.360 |
|
Daily hygiene (Swedish Stroke Register Questionnaire) |
0.256 |
7.833 |
0.224–273.360 |
|
Mobility (EQ-5D) |
0.561 |
0.555 |
0.076–4.051 |
|
*p ≤ 0.05; **p ≤ 0.01. CI: confidence interval. |
|||
|
Table II. Logistic regression model for participation in the domain of “family role”(IPA), with single items of European Brain Injury Questionnaire (EBIQ) from the domains isolation, cognition and communication and mobility (EuroQol (EQ-5D)) |
|||
|
p-value |
Odds ratio |
95% CI for odds ratio |
|
|
Others do not understand my problems EBIQ 6 |
0.010** |
23.591 |
2.130–261.327 |
|
Trouble with concentration EBIQ 22 |
0.065 |
31.257 |
0.804–1215.909 |
|
Mobility (EQ-5D) |
0.571 |
1.860 |
0.218–15.908 |
|
Difficulty in communication EBIQ 35 |
0.247 |
2.740 |
0.451–16.662 |
|
Thinking only of myself EBIQ 39 |
0.048* |
18.969 |
1.030–349.514 |
|
*p ≤ 0.05; **p ≤ 0.01. IPA: Impact on Participation and Autonomy; CI: confidence interval. |
|||
|
Table III. Logistic regression model for participation in the domain of “autonomy outdoors” (IPA), with single items of European Brain Injury Questionnaire (EBIQ) from the domains communication, isolation and cognition, the ability to perform daily hygiene (Swedish Stroke Register Questionnaire) and mobility (EuroQol (EQ-5D)) |
|||
|
p-value |
Odds ratio |
95% CI for odds ratio |
|
|
Mobility (EQ-5D) |
0.592 |
1.804 |
0.209–15.607 |
|
Daily hygiene (Swedish Stroke Register Questionnaire) |
0.156 |
20.614 |
0.315–1350.633 |
|
Losing contact with your friends EBIQ 60 |
0.022* |
9.442 |
1.377–64.749 |
|
Others do not understand my problems EBIQ 6 |
0.024* |
11.491 |
1.382–95.522 |
|
Failing to notice other people’s mood EBIQ 23 |
0.030* |
7.502 |
1.218–46.225 |
|
*p ≤ 0.05. IPA: Impact on Participation and Autonomy; CI: confidence interval. |
|||
|
Table IV. Logistic regression model for participation in the domain of “autonomy indoors” (IPA), with single items of European Brain Injury Questionnaire (EBIQ) from the domains isolation and communication, the ability to perform daily hygiene (Swedish Stroke Register Questionnaire) and mobility (EuroQol (EQ-5D)) |
|||
|
p-value |
Odds ratio |
95% CI for odds ratio |
|
|
Others do not understand my problems EBIQ 6 |
0.039* |
37.003 |
1.207–1134.493 |
|
Thinking only of myself EBIQ 39 |
0.023* |
16.956 |
1.484–193.736 |
|
Leaving it to others to start conversations EBIQ 55 |
0.108 |
9.424 |
0.612–145.136 |
|
Mobility (EQ-5D) |
0.665 |
2.219 |
0.067–73.118 |
|
Daily hygiene (Swedish Stroke Register Questionnaire) |
0.072 |
11.591 |
0.802–167.559 |
|
*p ≤ 0.05. CI: confidence interval. |
|||
DISCUSSION
The aim of this study was to explore what factors most affect the level of participation after a TBI in the individual’s subjective experience.
The study sample showed a trauma background from mild to severe brain injury in accordance with a TBI population diagnosed S06.2 and S06.3. Many subjects reported a large number of problems 4 years after the TBI, as expected. In the EBIQ, 40% reported problems in 43 of 62 questions, and 20% stated problems in as many as 58 out of the 62 questions. The same tendency was seen in the EQ-5D, where 15–58% of the sample reported problems in different domains. It is worth noting that 25% of subject reported problems in mobility, 15% in self-care, and 33% in daily activities, and that the highest extent of problems, 58%, was related to anxiety/depression and, also as a high percentage (58%), pain 4 years after their TBI. The high percentage of problems with pain was, to some extent, unexpected, and therefore was not included in the regression models. However, in recent years, there has been a consensus in the research as to the importance of emotional problems, post-traumatic stress disorder and chronic pain for the impact on outcome after TBI (10, 20–24), and future studies should perhaps consider the impact of pain.
The experienced level of participation reported in the IPA ranged from very good to very poor, and it is impossible to say what an acceptable level is. Is a “fair” participation good enough after a successful rehabilitation? What can be expected after a brain injury? In this study, between 20% and 40% of the sample did not perceive good participation according to the answers on the IPA items. On the other hand, that means that 60%–80% experienced that they had good participation, even though the answer “fair” participation was not included in this group. The participation was not dependent on gender or severity of the brain injury. However, the areas of participation that were rated in the IPA are fundamental in life, and the goal of rehabilitation is to try to help brain-injured persons to achieve a participation good enough to make them feel satisfied, rather than a level of participation that is “fair”, or which only occurs in some aspects.
The results of the IPA showed that the largest proportion experienced good participation in the domain of “autonomy indoors”, which can be explained by the fact that only 25% had problems with mobility. In the other domains as much as 35–40% of the sample did not experience good participation. The objective was to try to find explanations for which factors have a relation to the level of participation. One conclusion was that it is difficult to find single predictors because of the many interacting variables that form a very complex context and reality. In the present study, pain, anxiety and depression were found to be major problems in the sample (58%). Somatic, emotional and cognitive problems after TBI are often associated with post-traumatic stress disorder and chronic pain, a constellation of findings that has been called the polytrauma clinical triad (20). That several factors interact in this way probably explains why it is so difficult to find single robust predictors. Better knowledge of these interactions may be a way to improve rehabilitation in order to reach good participation in society.
A range of components has been associated with participation after stroke and TBI. However, the impact of contextual factors (personal and environmental) is not yet well understood or documented (25). The findings of this study could therefore contribute to this area of knowledge, highlighting the importance of a well-functioning interaction between the injured brain and the environment, as well as of the emotional aspects and subjective experience in terms of having an influence on participation.
In our search for predictors of participation, we used the EBIQ questionnaire. The EBIQ domains were closely correlated, thus it was not meaningful to make an analysis at the domain level, which was a limitation of the study. Instead, the regression models had to be based on single items from the EBIQ that did not correlate with each other. This meant that, as not all questions could be included, a selection was necessary, which may have implied a loss of information. On the other hand, the significant results seem to be relevant to clinical experience and in line with other research (26–28). Another limitation could be the rather large drop-out, but in the analysis of drop-out there were no significant difference between the groups in age, gender or severity of injury, and therefore we think the result is possible to generalize.
Taking the results of the 4 models together, there were 5 different items that were significant as predictors based on the EBIQ answers that reflected different kinds of problems experienced. There may be a variety of reasons why these problems originate from different areas. The 5 items were “lack of interest in your surroundings”, “losing contact with your friends”, “others do not understand my problems”, “thinking only of myself” and “failing to notice other people’s mood”. Depression is common after a brain injury (21) and can be an explanation for all of the above items. That the focus of the injured persons is on themselves and their situation is also common and understandable, as the injured person often has quite enough to do in taking care of his own problems and is not able to pay great attention to others. Cognitive problems often accompany a brain injury, and problems with attention and working memory also come with a mild injury and may result in difficulties in observing and following what is going on around, and may appear to be a lack of interest. Taking note of signs and other people’s feelings may also be a problem. Difficulties in getting things done, and losing friends, can both be consequences of executive inability, i.e. initiating and finalizing tasks. The last of the predictors, the experience that others do not understand their problems, can be explained as the difficulty for a person who has not experienced cognitive problems to really understand what cognitive problems mean. In addition, the injured person may have difficulty explaining the problems, or may have exaggerated demands. In this study, it seems that emotional and social factors have a great influence on the level of participation. In line with these results is the conclusion of Wise’s study (5) that, after TBI, activities change from partying and sports to watching television.
In the domains of “autonomy outdoors” and “autonomy indoors” it was expected that mobility would be an important factor for participation, but this was not verified in this study. This should not be interpreted such that mobility is unimportant for outdoor or indoor autonomy, but could indicate that rehabilitation has good means to compensate for this kind of problem. It might have been expected that mobility and personal care would also have influenced the participation of the domains of “family role” and “social life”, as this kind of dependency is often a pressure on the relation to family and friends. Perhaps like the above, the Swedish social healthcare system provides satisfying assistance and good assistive devices, which means that other factors have a greater impact
It was interesting to note that those who reported good participation in the IPA stated their health in the VAS scale of the EQ-5D to be at the same level as the Swedish norm group, while those who stated “not good participation” reported a low current health status in the EQ-5D. This could be understood such that a person with good participation also perceives having a good health status, in spite of the presence of deficits.
In conclusion, the study found that the sample of TBI reported a number of activity limitations, and approximately 40% also experienced restrictions in participation in the domains of social life, family role and autonomy outdoors. The analyses gave 5 predictors reflecting emotional and social aspects, which could explain up to 70% of the variation in participation. The study also tells us that a great deal of the explanation should also be seen as being connected to an interaction between several aspects. The findings will contribute to the body of knowledge, but further studies are needed to be able to improve participation for persons with disability after a TBI.
REFERENCES
