Anne Norup, PhD1, Lars Siert, MSc1 and Erik Lykke Mortensen, MSc2
From the 1Research Unit on BRain Injury rehabilitation, Copenhagen (RUBRIC), Department of Neurorehabilitation, Traumatic Brain Injury Unit, Copenhagen, University Hospital, Glostrup and 2Institute of Public Health and Center for Healthy Aging, University of Copenhagen, Copenhagen, Denmark
OBJECTIVE: This pilot study investigated the effects of acute neuropsychological intervention for relatives of patients with severe brain injury.
METHODS: Participants were enrolled in an intervention group comprising 39 relatives, and a control group comprising 47 relatives. The intervention consisted of supportive and psycho-educational sessions with a neuropsychologist in the acute care setting. The intervention group completed self-report scales in the acute setting and after the intervention at admission to sub-acute rehabilitation. The control group completed the self-report scales only at admission to sub-acute rehabilitation. Outcome measures included selected scales from the Symptom Checklist Revised 90 (SCL-90-R), the Short Form 36 (SF-36), and a visual analogue quality of life scale.
RESULTS: The intervention group showed a significant decrease in anxiety scores from the acute to the sub-acute setting (t = 2.70, p = 0.010, d = 0.30), but also significantly lower Role Emotional scores (t = 2.12, p = 0.043, d = 0.40). In the sub-acute setting, an analysis of covariance model showed a borderline significant difference between the intervention and the control group on the anxiety scale (p = 0.066, d = 0.59).
CONCLUSION: Any effects of the acute neuropsychological intervention were limited. Further research is needed to explore the effects of different interventions in more homogenous and larger groups of relatives.
Key words: acute neuropsychological intervention; relatives; severe brain injury; anxiety; depression; quality of life.
J Rehabil Med 2013; 45: 827–834
Correspondence address: Anne Norup, Department of Neurorehabilitation, Traumatic Brain Injury Unit, Copenhagen University Hospital, Glostrup, Denmark. E-mail: anne.norup@regionh.dk
Accepted April 23, 2013
INTRODUCTION
Emotional strain and distress in relatives of patients with brain injury have been documented in a number of studies (1–8). The majority of studies have focused on the long-term impact on family members, and there has been a lack of studies investigating the early effects of brain injury and the family’s condition during hospitalization. Only two studies have been identified investigating relatives of patients with severe brain injury in the early phases of hospitalization (9, 10). Pielmaier et al. (10) reported that more than half of relatives of patients with severe traumatic brain injury (TBI) admitted to critical care had clinically significant post-traumatic stress symptoms shortly after the injury, which is in concordance with our findings in a neuro intensive care unit (NICU) reporting high frequencies of anxiety and depression (9). These results are consistent with research with longer follow-up investigating the condition of the relatives (6, 11–14).
A review concerning the emotional condition of relatives of critically ill patients in intensive care units (ICUs) and NICUs found that most relatives needed “to have questions answered honestly” and “to know specific facts regarding what is wrong with the patient and the patient’s progress”. The review concluded that information was the most important need identified in critical care, when the patient’s situation is unstable. The families sought honest and frequent information about progress, status and prognosis (15).
A few intervention studies have been conducted investigating different types of interventions for families of brain injury survivors in outpatient centres years after injury (16–21). Despite knowledge of the distress and needs of families of patients admitted to NICUs (3, 9, 10, 15), no studies have investigated and evaluated intervention for families of brain injury survivors in the early phases of rehabilitation.
Present study
The present pilot study was designed in an attempt to meet the needs of the relatives in the early phases of rehabilitation. When receiving the families at admission to sub-acute rehabilitation most families expressed a need for support and information that they felt had not been met in the acute setting. Therefore, this pilot study tried to meet the needs of the relatives in the acute setting based on our clinical experience.
The purpose of the study was to investigate the effects of neuropsychological intervention for relatives of patients with severe brain injury in the acute care setting. The intervention consisted of supportive sessions with a trained neuropsychologist, and the sessions were a flexible mixture of both psycho-education and emotional support. The sessions were individualized and focused primarily on the family’s immediate situation with a close family member in hospital.
The aims of the pilot study were to investigate whether:
MATERIAL AND METHODS
Participants
Two groups of relatives of patients with a severe brain injury were included: an intervention group receiving acute neuropsychological intervention and a control group receiving no intervention in acute care. The intervention group initially comprised 46 relatives, but because 4 patients died and 3 relatives did not return follow-up questionnaires at admission to rehabilitation, data are reported for only 39 relatives. The control group comprised 47 relatives, who completed the questionnaires only when included at admission to sub-acute rehabilitation.
All patients had severe brain injury and a need for intensive neurorehabilitation. Patients admitted for rehabilitation have to fulfil the admission criteria of the unit, where the highest priority is given to patients who after initial treatment in a neurosurgical or other clinic have a Glasgow Coma Score (GCS) in the range 3–12 one day after cessation of sedation. All such survivors are transferred as soon as they breathe spontaneously, even if the prognosis for recovery may appear extremely bad.
Secondly, the unit admits patients with a GCS of 13–14 one day after cessation of sedation. These patients are admitted only if they have severe focal neurological deficits, such as aphasia, hemiparesis and/or are severely agitated (the admission criteria are more thoroughly described in previous publications (22, 23)).
Exclusion criteria were: relatives who did not speak Danish, those who had a psychiatric diagnosis, or a progressive brain disease.
Procedure
The two groups of relatives were included at two different time-points and allocated to the two groups depending on time of enrolment. Despite the different time of enrolment, all patients had been through the same pathway of care in the acute setting.
The intervention group was included at the neuro-intensive care unit (T1), when the patient’s condition was stabilized, and the control group was included at admission to the sub-acute rehabilitation (T2). Patients were included only if they fulfilled the criteria above, and if the relative did not meet any of the exclusion criteria. Both groups were admitted for intensive neurorehabilitation in the sub-acute phase at the traumatic brain injury unit (Fig. 1).
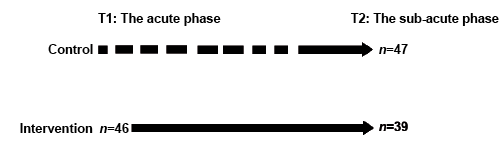
Fig. 1. Inclusion procedure.
Oral consent to participate was obtained by a neuropsychologist, when the relative was included. If more than one relative was present at the time of inclusion, the family decided who should participate in the study.
The study was approved by the Committees on Biomedical Research Ethics of the Capital Region of Denmark (journal number H-KF-311150) as the Danish Data Protection Agency (journal number 2007-41-0583).
Intervention
Method. The intervention group received neuropsychological support during acute care, conducted by neuropsychologists trained in dealing with psychological trauma and having years of experience in the field of brain injury rehabilitation. The sessions did not follow a specific treatment manual, as the emotional condition, and consequently the needs, of relatives differed considerably. In each session the neuropsychologist decided on the most beneficial structure of the session according to the needs of the relatives, balancing between psychological support and psycho-education. This method was chosen after conducting a few pilot sessions facing the very different situations and needs of the families. The intervention was administered during the first 3 weeks after the injury.
Purpose and expected benefits. The purpose of the intervention was two-fold, and consequently it was a flexible mixture of both emotional support and psycho-education. The sessions were targeted on the family’s immediate situation with a close family member severely ill in hospital. The first purpose of the intervention was providing psychological support to the family in terms of dealing with the distressing situation of having a critically ill family member. The primary objective for the neuropsychologist was to listen and to instil hope in the families by identifying progress in the patient’s condition and personal strengths in the relatives. This was expected to help families regain hope in the future, and indirectly cause emotional relief. The second purpose of the session was psycho-educational, providing information about treatment in the acute setting and the consequences of brain injury. Giving needed information was expected to improve understanding of the patient’s condition and reduce anxiety and more general symptoms of distress. The relatives were only given information they requested, and in each session the neuropsychologist carefully evaluated how much information the relatives were capable of receiving without causing further distress (Table I).
|
Table I. Overview of intervention |
|||
|
Purpose |
Objective |
Expected benefits |
Examples of topics |
|
Emotional support |
Identifying progress in the patient’s condition and emotional strength in the relative by listening and instilling hope |
Regain hope in the future and indirectly causing emotional relief |
Handling each day with a family member in hospital Feelings of isolation, guilt and distress |
|
Psycho-education |
Improve understanding of the patient’s condition by providing information |
Reduce anxiety and general symptoms of distress |
Treatment in the acute setting; monitoring of intracranial pressure, decompressive surgery, etc. The first period of unconsciousness, vegetative and minimally conscious state Post-traumatic amnesia, consequences and recovery from brain injury |
Content and topics. The topics of the sessions depended on the relatives’ specific needs. Every session began with the neuropsychologist asking the family how they experienced the accident, if they witnessed it or were involved. In cases in which the relatives had not been present, they were asked to share how they received the message about the accident. The relatives often needed immediate psychological support to help them deal with their own emotional reactions and needs during the first critical phases of the patient’s stay in the acute setting. Topics often addressed in the supportive part of the sessions were how to handle each day with a close family member in hospital, feelings of isolation, guilt and emotional distress. The second part of the sessions was psycho-educational, and the relatives were able to ask any questions regarding treatment in the acute setting, the first period of unconsciousness, post-traumatic amnesia, consequences of brain injury and recovery from brain injury.
In some cases, the relatives had obvious symptoms of anxiety, being tense, physically restless and almost unable to sit still. In such sessions, the focus remained on the immediate situation and how to handle this. In cases, where the families were more calm and able to receive information, the neuropsychologist tried to answer the relatives’ questions about prognosis, treatment in the acute setting, etc. However, it was very important that each session was finished properly, making sure that the relatives had no further questions or queries.
Outcome measures. Effects of the intervention were assessed by having the relatives complete standardized questionnaires regarding anxiety, depression and quality of life (information regarding the specific measures is given below). Anxiety and depression were chosen, as these symptoms have been described in families of brain injury survivors for years (15, 24–27). We expected anxiety to be more sensitive to the intervention, as information is known to be able to reduce anxiety.
A quality of life measure was also included; as research has shown that quality of life can be high in caregivers despite high levels of distress (28).
Amount of intervention. The duration of the sessions was 1–1.5 h, depending on the relatives and their ability to maintain concentration throughout the session. In some cases, the relatives were very restless, as described above, and the sessions were kept brief. However, more often the family enjoyed the respite from the bedside and the possibility to talk about their loved one and their current situation. The majority of the relatives (67.4%) received 1 session. Of the relatives, 17.4% had 2 sessions, 13.0% had 3 sessions, and 1 relative had 4 sessions (2.2%).
An independent samples t-test showed no difference in the relatives’ emotional wellbeing on T2 depending on whether or not the relative received more than 1 session of intervention.
Assessment of relatives
Outcome measures were administered at T1 and T2 in the intervention group and at T2 in the control group, as described below.
Quality of life. Each relative was asked to complete the Short Form 36 (SF-36), a measure of self-reported health-related quality of life. The questionnaire comprises 36 items addressing 8 dimensions of health. Scores in each domain of the SF-36 range from 0 to 100, with higher scores indicating better health. Only 4 scales were used in the present study: Role Emotional (RE), Social Function (SF), Mental Health (MH) and Vitality (VT). The scores of the relatives were evaluated in terms of available Danish norms (29). This normative study showed high Cronbach’s alpha coefficients on all the subscales used in this study ranging from 0.75 to 0.85 (29).
The relatives were also asked to rate their own perception of quality of life on a visual analogue scale (VAS) with a range from 0 to 10; 0 indicating “very dissatisfied” and 10 indicating “very satisfied”.
Anxiety and depression. The relatives’ symptoms of anxiety and depression were evaluated by the relevant scales of Symptom Check List 90 Revised (SCL-90-R); a self-report checklist designed to reflect the symptom pattern and level of distress (30). Each item is scored on a scale of 0 (“not at all”) to 4 (“extremely”), indicating the degree of distress for that particular item. The respondents are asked to answer each item according to their condition during the past 7 days. Raw-scores were converted into T-scores, and evaluated in terms of the gender-specific norms for a Danish sample. This Danish population study revealed high alpha coefficients on all the SCL subscales, and in particular for the depression and anxiety scales used in this study (a = 0.91 and a = 0.86, respectively) (30).
We also registered the relatives’ social support and prior life events, as both factors are known to influence emotional reactions (1, 30–32).
Social support and life events. Questions regarding the relatives’ social support included a question about how often they had contact with different people (parents, children, other family, colleagues after work, neighbours, childhood friends, other friends, professional caregiver), and how satisfied the relative was with this contact. The relatives also reported how many people they were able to share very personal matters with.
Questions about traumatic life events over the past year and over the entire life-span included 5 work-related questions (unemployment, not being promoted, conflicts with colleagues, superiors or subordinates) and 7 questions related to events in the family (children severely ill, severe educational problems for children, severe conflicts with grown-up children, severe problems in marriage, own severe illness, severe illness or death among relatives, severe economical problems). We counted the total amount of traumatic events in the past year and over the entire life.
The questions were modified versions of questions used in the Copenhagen City Heart Study and were administered, when the relatives were enrolled (33).
Assessment of patients
As a standard procedure during admission, relevant data were collected regarding the patient’s condition: severity of injury, level of consciousness and function. Data regarding the condition of the patients were included in the study, as previous research has shown how the condition of the patient and the relative are entangled (3, 9, 24).
Severity of injury. The severity of injury was assessed by two well-known and validated scales: The Glasgow Coma Score (34) and the Injury Severity Score (ISS) (35). GCS is scored from 3 to 15. Patients with scores less than 9 are considered to be in coma, and patients with scores of 15 have spontaneous eye opening, are able to follow commands and are fully oriented. According to criteria for injury severity, GCS scores of 8 or less are classified as severe injuries. The treating physician assessed GCS at admission to the traumatic brain injury unit.
The treating physician also estimated the ISS, which consists of an anatomical scoring system that provides an overall score for patients with multiple traumatic injuries. The ISS ranges from 0 to 75. Each injury is assigned an Abbreviated Injury Scale (AIS) score and is allocated to 1 of 6 body regions (head, face, chest, abdomen, extremities and skin). Only the highest AIS score in each region of the body is used. The scores of the 3 most severely injured regions are added together to produce the ISS. The ISS was only assessed for patients with a traumatic brain injury.
Level of consciousness. Rancho Los Amigos (RLA) score (36, 37) was assessed by a neuropsychologist at admission to sub-acute rehabilitation. This score ranges from level 1, which describes a comatose condition with no observable response, to level 8, which is a condition with purposeful and appropriate responses. This scale was designed for use on patients with a traumatic brain injury.
Functional level. The patient’s functional level at admission was assessed with the Early Functional Abilities (EFA) and the Functional Independence Measure (FIM).
The EFA is an assessment tool for patients with severe cerebral impairments in the early neurological rehabilitation stage, which describes clinically observable changes in a patient’s early functional abilities (38) The EFA Scale contains 20 items and assesses early basic abilities related to 4 functional areas: vegetative, face and oral, sensory-motor, and sensory cognitive functions. Each item is rated on a 5-point scale from “not obviously observable” to “no essential functional limitation”. The total score is the sum of the item scores, ranging from 20 to a maximum of 100. High scores indicate better functional ability.
The FIM (39) is an 18-item rating scale assessing activities of daily living (ADL): self-care, bowel and bladder management, mobility, communication, cognition, and psychosocial adjustment. Each item is rated on a 7-point scale, from “total assistance” to “complete independence”. A total FIM score ranges from 18 to 126 with higher scores indicating greater independence. The FIM Scale has been shown to be valid and reliable for measuring functional outcome after TBI.
Both FIM and EFA scores assessed by physiotherapists and occupational therapists, who were trained users of the scales.
Data analysis
Descriptive statistics were used; results are presented as percentages and means with standard deviation and range. Categorical and ordinal data were analysed using χ2 and Mann-Whitney tests. Changes in the relatives’ emotional condition between T1 and T2 were analysed with paired t-tests and the emotional condition of the intervention and control group were compared using independent samples t-tests. ANCOVA was used to adjust for the relatives’ gender and for the observed group differences on variables with significantly different distributions in the two patient groups. We calculated Cohen’s d to estimate effect size.
All data was analysed using two-tailed testing, and p = 0.05 as a threshold for statistical significance. The statistical software used was SPSS version 19.0.
RESULTS
Description of the intervention and the control group
The intervention group consisted primarily of parents (61%) and spouses (20%), and most relatives were female (80%). The majority of the relatives (59%) were living with the patient at time of injury and most (87%) were working at time of injury. The majority of the patients was male (80%) and had sustained a TBI (80%). A fifth of the intervention group had sustained a non-traumatic brain injury (NTBI) caused by spontaneous intracranial haemorrhage (2.5%), subarachnoid haemorrhage (5%), brain tumour (2.5%) and major cerebral infarction (10%). The mean age of the patients in the intervention group was 31 years (standard deviation (SD) 17; range 4–71 years) (Table II).
The control group consisted primarily of females (69%), and most relatives were spouses (44%) or parents (27%). The majority of the relatives (58%) were living with the patient at time of injury, and the majority (83%) was working at time of injury.
Most patients in the control group were male (68%) and had acquired a TBI (66%). Of the patients in the control group, 16 had acquired a NTBI caused by cardiac arrest (8%), spontaneous intracranial haemorrhage (4.5%), subarachnoid haemorrhage (4.5%), major cerebral infarction (11%), tumour (2%) and meningitis (2%). The mean age of the patients in the control group was approximately 46 years (SD 20; range 1–82) (Table II).
|
Table II. Characteristics of the relatives and the patients retrieved at baseline p-values from Student’s t-test for continuous data, from χ2 tests (or Fisher’s exact test) for categorical characteristics and Mann-Whitney for ordinal data |
|||
|
Characteristics of the relatives |
Intervention group (n = 39) |
Control group (n = 47) |
p-valuea |
|
Female, n (%) |
31 (80) |
32 (69) |
0.211 |
|
Cohabitant at time of injury, n (%) |
23 (59) |
28 (58) |
0.820 |
|
Working at time of injury, age 16–66 years, n (%) |
34 (87) |
40 (83) |
0.683 |
|
Relationship, n (%) |
|||
|
Spouse Parent Sibling Child Boy-/girlfriend Other |
8 (20) |
21 (44) |
0.002 |
|
24 (61) |
13 (27) |
||
|
1 (3) |
2 (4) |
||
|
5 (13) |
8 (17) |
||
|
0 (0) |
3 (6) |
||
|
1 (3) |
1 (2) |
||
|
Social support |
|||
|
Very satisfied, % People to talk with about personal matters, median (range) |
82 |
80 |
0.855 |
|
4 (1–6) |
3 (1–8) |
0.377 |
|
|
Life events, median (range) |
|||
|
Last year Entire life |
0 (0–2) |
1 (0–4) |
0.434 |
|
2 (0–5) |
2 (0–5) |
0.651 |
|
|
Completion of questionnaires, mean (SD) [range] |
|||
|
T1: NICU, days after injury |
16 (6) [5–32] |
– |
– |
|
T2: Sub-acute rehab, days after injury |
24 (8) [11–41] |
35 (18) [9–77] |
0.001 |
|
Characteristics of the patients, n (%) |
|
||
|
Male |
31 (80) |
32 (68) |
0.145 |
|
Traumatic brain injury |
31 (80) |
31 (66) |
0.211 |
|
Clinical status at admission to rehabilitation, mean (SD) [range] |
|||
|
Admission, number of days after injury |
17 (6) [7–34] |
24 (16) [8–68] |
0.013 |
|
Age |
31.35 (17.02) [4–71] |
45.51 (19.62) [1–82] |
< 0.001 |
|
Glasgow Coma Score |
10.44 (2.96) [4–15] |
11.05 (3.25) [5–15] |
0.402 |
|
Early Functional Abilities |
42.47 (17.42) [23–90] |
44.80 (19.81) [22–91] |
0.784 |
|
Functional Independence Measure |
22.11 (12.06) [18–74] |
24.36 (13.82) [18–68] |
0.451 |
|
Rancho Los Amigo |
3.86 (1.68) [2–8] |
4.00 (1.39) [2–7] |
0.805 |
|
Injury severity |
34.90 (10.94) [25–66] |
28.58 (7.09) [10–43] |
0.009 |
|
SD: standard deviation. |
|||
The relatives in the intervention group completed questionnaires regarding emotional wellbeing in the acute phase (T1) on average 16 days (SD 6; range 5–32) after injury, and once again when the patient was transferred to sub-acute rehabilitation (T2) about 24 days (SD 8; range 11–41) after injury. The patients in the intervention group were admitted to rehabilitation 17 days (SD 6; range 7–34) after injury.
The patients in the control group were admitted to sub-acute rehabilitation 24 days (SD 16; range 8–68) after injury on average, and their relatives completed the questionnaires at admission to sub-acute rehabilitation (T2) 35 days (SD 18; range 9–77) days after injury.
Condition of the relatives
The condition of the relatives in the two groups was assessed and compared with the relevant Danish norms (29, 30) using one-sample t-tests. The relatives in both groups had significantly higher scores on the depression and anxiety scales and significantly lower quality of life at T2 compared with Danish norms, and this was also the case for the intervention group at T1. Means, SD and range can be seen in Table III.
Changes in emotional wellbeing from T1 to T2
Quality of life. The intervention group became significantly worse from T1 to T2 (t = 2.12, p = 0.043, d = 0.40) on the RE-scale, but a trend towards improvement on the VT-scale was found (t = –2.02, p = 0.051, d = 0.18). No change from T1 to T2 was observed on the MH-scale and SF-scale.
On the VAS, the relatives in the acute group rated their quality of life slightly better on T2 compared with T1 (Table III).
|
Table III. Emotional condition of the relatives at the acute phase (T1) and the sub-acute phase (T2) |
||||||
|
The intervention group |
The control group |
|||||
|
T1 (n = 39) |
T2 (n = 39) |
T2 (n = 47) |
||||
|
Mean (SD) |
Range |
Mean (SD) |
Range |
Mean (SD) |
Range |
|
|
Quality of life |
||||||
|
SF-36 |
||||||
|
VT |
28.38 (19.62) |
0–75 |
31.84 (17.45) |
10–75 |
33.04 (20.48) |
0–75 |
|
SF |
53.62 (30.05) |
0–100 |
50.96 (30.40) |
0–100 |
56.12 (27.69) |
0–100 |
|
MH |
33.58 (17.61) |
4–76 |
34.39 (14.67) |
13–77 |
32.00 (16.52) |
3–73 |
|
RE |
26.01 (31.38) |
0–100 |
13.54 (20.49) |
0–67* |
25.83 (31.57) |
0–100*** |
|
VAS |
6.40 (3.01) |
1–10 |
6.43 (2.8) |
1–10 |
6.27 (2.77) |
0–10 |
|
Emotional distress |
||||||
|
SCL-90-R |
||||||
|
Anxiety |
64.08 (7.75) |
45–80 |
61.72 (8.31) |
36–73** |
61.91 (9.89) |
36–80 |
|
Depression |
64.00 (6.94) |
47–80 |
61.95 (7.56) |
41–80 |
61.96 (8.29) |
43–75 |
|
*Significant decrease from T1 to T2, p = 0.043, Cohen’s d = 0.40. **Significant decrease from T1 to T2, p = 0.010, Cohen’s d = 0.30. ***Significant difference comparing the groups at T2, p = 0.05, Cohen’s d = 0.39. SD: standard deviation; SF-36: Short Form 36; VT: Vitality; SF: Social Function; MH: Mental Health; RE: Role Emotional; VAS: Visual Analogue Scale; SCL-90-R: Symptom Checklist Revised. |
||||||



Emotional distress. The intervention group experienced significantly less anxiety at T2 compared with T1 (t = 2.70, p = 0.010, d = 0.30), and scored lower on depression at T2 compared with T1, although not significantly lower (t = 1.77, p = 0.085, d = 0.29) (Table III).
Comparisons between the intervention and the control group
Group differences. The control group was admitted to rehabilitation and completed the questionnaires later than the intervention group (see Table II). The groups did not differ significantly with regards to occupational status, cohabitation status or gender distribution.
The relative’s relationship to the patient was re-coded into 3 categories; parents, spouses and others (siblings, children, boy-/girlfriends), and a χ2 test showed that the relatives’ relationship to the patient was distributed significantly different in the 2 groups (see Table II). The groups did not differ significantly with regards to social support or experienced life events.
The patients in the intervention group were significantly younger than the control group, and the intervention group had a significantly higher ISS score than the control group, indicating that patients in the intervention group had more severe injuries (Table II for results regarding group differences).
Quality of life. A significant difference was found on the RE-scale; the control group had significantly better scores on T2 (t = –1.99, p = 0.05, d = 0.39) than the intervention group. No difference was observed between the two groups on the MH-, SF- or VT-scales.
No difference was found when comparing the VAS scores of the intervention group with the VAS scores of the control group scores at T2 (Table III).
Emotional distress. No difference was found with regards to symptoms of anxiety or depression, when comparing the two groups at T2 (Table III).
Adjusted differences between groups
An ANCOVA model was used to adjust for gender and variables showing significantly different distribution in the intervention and the control group. The model adjusted for the relative’s gender, the relatives’ relationship to the patient (spouse vs other), the patient’s age and the number of days after injury that the relatives completed the questionnaire. The model also adjusted for the ISS, and this reduced our sample, as it is only applicable to patients with TBI (see Table IV for raw and adjusted means).
|
Table IV. Raw and adjusted means for emotional distress and quality of life at sub-acute phase |
|||||||
|
Quality of life |
The intervention group |
The control group |
p-values |
||||
|
Raw mean |
Adjusted meanb |
Raw mean |
Adjusted meanb |
Unadjusteda |
Adjustedb |
||
|
VT (n = 59) |
30.86 |
34.34 |
38.00 |
34.64 |
0.776 |
0.925 |
|
|
SF (n = 61) |
47.17 |
53.24 |
62.50 |
58.56 |
0.413 |
0.558 |
|
|
MH (n = 58) |
32.87 |
37.05 |
32.76 |
28.58 |
0.493 |
0.070 |
|
|
RE (n = 47) |
15.94 |
22.45 |
31.94 |
25.70 |
0.061 |
0.710 |
|
|
VAS (n = 59) |
6.46 |
6.81 |
6.38 |
6.04 |
0.788 |
0.354 |
|
|
Emotional distress |
|||||||
|
Anxiety (n = 61) |
61.73 |
59.46 |
62.03 |
64.23 |
0.922 |
0.066 |
|
|
Depression (n = 61) |
62.17 |
61.02 |
61.90 |
63.01 |
0.996 |
0.338 |
|
|
aUnadjusted p-values calculated from independent t-tests. bAdjusted for the relative’s gender and relationship to the patient (spouse vs other), the patient’s age, number of days after injury that questionnaire was completed and the patient’s the injury severity score. VAS: visual analogue scale; VT: Vitality; SF: Social Function; MH: Mental Health; RE: Role Emotional. |
|||||||
No significant differences were found, but we did find a non-significant trend towards higher anxiety (p = 0.066, d = 0.59) and depression scores (p = 0.338, d = 0.31) in the control group at T2. With regards to quality of life, the control group showed lower adjusted VAS scores (p = 0.351, d = 0.30), but non-significant, and this was also the case on the MH-scale (p = 0.070, d = 0.61). Scores on the anxiety and MH-scale were borderline significant. Table IV shows that the control group obtained higher scores on the remaining SF-36 scales, however non-significant.
Supplementary analyses
The age of the patient was significant in the model, and consequently possible interactions between the age of the patient and the effect of the intervention were tested. However, the differences were not significant, and analyses including only patients above the age of 15 years showed results similar to those obtained for the full sample.
However, in the full sample, the age of the patient was important in relation to anxiety (p < 0.001) and depression (p < 0.001), indicating that relatives of older patients experienced less anxiety and depression. The relatives of older patients had higher scores on the VAS (p = 0.001), RE- (p = 0.001), MH- (p < 0.001) and VT-scales (p < 0.001), indicating better quality of life.
We also found that spouses had higher levels of depression (p < 0.001) and anxiety (p = 0.001) and reported lower quality of life at MH- (p = 0.002) and VT-scale (p = 0.007) compared with other relatives.
DISCUSSION
Changes in emotional wellbeing from T1 to T2
We found a significant decrease in symptoms of anxiety from T1 to T2 and a decrease in symptoms of depression; however, this decrease was not significant. We found a borderline significant increase in Vitality scores, but the only significant change on the SF-36 scales was a decrease in RE scores from T1 to T2, indicating lower quality of life at T2.
Anxiety probably reflects acute worries about the patient and the future, and these symptoms may decrease more rapidly than symptoms of depression, as other studies have shown that symptoms of depression can persist for years after injury (2, 5–7, 25, 31). The decrease in symptoms of anxiety and depression and improvement in vitality could be caused by the intervention, but it is very likely that the decrease is a consequence of a more spontaneous improvement in the emotional state of the relatives related to the patient’s more stable and perhaps improved condition (40).
Low scores on the RE-scale reflect problems with work or other daily activities as a result of emotional problems. It is very likely that relatives rate this score lower at T2 because at this point they realize the severity of the injury and the long-term care and rehabilitation needed.
Because of the intervention as well as the stabilization of the patient’s condition, an improvement in the condition of the relatives from T1 to T2 was anticipated, and the control group was included in attempt to obtain a more realistic picture of the effects of the intervention.
Comparisons between the intervention and the control group
The control group was included at admission to rehabilitation in hospital and had not received any kind of intervention in the acute setting. Unfortunately, there were many differences between the two groups: the intervention group completed the questionnaire earlier, the patients were younger and had more severe injuries, and the distribution of parents and spouses was significantly different in the two groups. When adjusting for these differences more anxiety and depression were found in the control group as well as lower VAS and MH-scores. The results regarding anxiety and the scores on the MH-scale were borderline significant, but the others were non-significant. We also found a non-significant tendency towards higher scores on the RE- and SF-scales in the control group.
The results are somewhat mixed when comparing the 2 groups, but it is clear that any effects of the intervention were small. Other factors appeared to be more important since the age of the patient and the relatives’ relationship to the patient overrode any effects of the intervention.
This result was unexpected, and in contrast to what most relatives had expressed, since the majority spontaneously expressed satisfaction with the information and support received during the sessions. However, it is likely that the intervention should have been provided even earlier than it was administered. Many relatives pointed out that their need for psychological support as well as information had been more critical earlier during the patient’s stay in acute care. Moreover, in most cases the intervention was limited to only one session, and this may not be enough to produce detectable effects. This indicates that both the timing of and the amount of intervention are important parameters if effects should be detectable.
To the authors’ knowledge, this study is the only one investigating the effect of an early intervention study and therefore adds to the knowledge available regarding the condition of the relatives in the early phases of rehabilitation. Nevertheless, the intervention conducted only had limited effects on emotional distress. The intervention studies previously conducted regarding psychological support have also had difficulties proving effects on standardized measures of psychological distress (16, 18, 21, 41). Intervention effects seem to be more detectable on more subjective measures (17, 42, 43).
Methodological considerations
The aim of this study was to examine the effects of neuropsychological intervention in the acute setting, but a variety of circumstances influenced our data collection and the two groups differed on a number of key variables.
In many cases, one of several eligible relatives volunteered to participate at the critical time of enrolment, and it was not deemed justifiable to ask specific members of the families to participate. Of course, this choice may have resulted in bias, as we might primarily have included resilient and emotionally strong relatives, which may indirectly have influenced the effects of intervention. In addition, this choice made it impossible to stratify the relatives according to their relationship to the patient.
Our samples were relatively small, and it is likely that statistical power was not sufficient to detect small effects of the intervention.
It is also a limitation that we used general measures of mental symptoms and quality of life, since it is possible that outcome measures specifically aimed at detailed description of the immediate emotional distress and concrete worries and concerns of the relatives may be more sensitive to the effects of interventions.
Implications
This pilot study has emphasized the emotionally straining situation of families of brain injury survivors in the early phases of rehabilitation and the need for early intervention. No other studies have investigated the effects of early psychological intervention despite the call for early supportive intervention demonstrated in previous research (3, 9, 10, 44).
Future research should focus on obtaining larger samples and investigating intervention characteristics, such as timing, number of sessions and follow-up time. Randomized studies should be considered, but if this is considered unethical, efforts should be made to obtain more comparable intervention and control groups than we were able to obtain in the present study. Larger samples should enable better statistical control of background variables, but individual matching is also a possibility. Choice of outcome measures, as well as follow-up time after intervention, should be considered thoroughly, as changes in distress might require a longer follow-up time to be measurable. Moreover, it would be relevant to include families’ ratings of their gains and the beneficial components of the intervention.
Conclusion
In the intervention group, a decrease in symptoms of anxiety and depression from T1 to T2 was observed, and this group also showed less anxiety than the control group. However, most effects were small, and consequently the study did not demonstrate convincing effects of a short neuropsychological intervention administered early in the acute phase. Despite the negative results, psychological intervention of sufficient duration is likely to reduce emotional strain and distress, and this possibility should be explored further in future studies.
ACKNOWLEDGEMENTS
The authors would like to thank all participants in the study, and additionally acknowledge the support of the staff at the NICU, Department of Neuroanaesthesiology, Rigshospitalet, Copenhagen University Hospital, in particular Karen-Lise Welling, PhD, and Jesper Qvist, MD. The authors would also like to thank the staff at the Department of Neurorehabilitation, Traumatic Brain Injury Unit, Copenhagen University Hospital, Glostrup, Denmark.
Conflicts of interest. No commercial party had direct influence on the results of the research supporting this article. The study was supported in part by a grant from Aase and Ejnar Danielsens Foundation.
REFERENCES
