Borja Sañudo, PhD1, Luis Carrasco, PhD1, Moisés de Hoyo, PhD1, Ángel Oliva-Pascual-Vaca, PhD2 and Cleofás Rodríguez-Blanco, PhD2
From the Departments of 1Physical Education and Sport and 2Physiotherapy, University of Seville, Seville, Spain
OBJECTIVE: To determine whether an 8-week exercise programme supplemented with whole-body vibration improves body balance and dynamic strength in women with fibromyalgia.
DESIGN: Randomized controlled trial.
Patients: Forty-six participants diagnosed with fibromyalgia.
METHODS: Participants were randomly assigned to: (i) an exercise training group with whole-body vibration (n = 15), which performed twice-weekly exercise sessions (aerobic exercise, strengthening and flexibility) combined with 3 whole-body vibration training sessions a week (bilateral squats: 6–9 sets of 30 s with 45-s recovery between sets; and unilateral squat: 4–7 sets of 30 s, 30 Hz–4 mm); (ii) an exercise group (n = 15) with the same combined exercise therapy; and (iii) a usual-care control group (n = 16).
RESULTS: Statistically significant improvements in the Medio–Lateral Stability Index and Medio–Lateral Mean Deflection with open eyes were found in the whole-body vibration exercise group compared with the control group. Non-significant effects were found for lower-limb physical function.
CONCLUSION: The results show that a traditional exercise programme, supplemented with whole-body vibration training, improved balance in women with fibromyalgia. This may represent a key factor for falls prevention in this patient group.
Key words: physical function; fall prevention; vibration training; strength; neuromuscular performance; fibromyalgia.
J Rehabil Med 2013; 45: 678–684
Correspondence address: Borja Sañudo, Dpto. Educación Física y Deporte, Facultad de Ciencias de la Educación, Universidad de Sevilla, Pirotécnia s/n, ES-41013 Seville, Spain. E-mail: bsancor@us.es
Accepted Feb 7, 2013; Epub ahead of print Jun 24, 2013
Introduction
Fibromyalgia (FM) is characterized by chronic widespread pain, mainly in musculoskeletal structures, and multiple additional clinical features, such as fatigue, disrupted sleep, and poor physical fitness (1). Patients with FM also report significantly lower perceived functional ability and impaired postural control compared with matched controls (2). Patients with FM report significantly more falls than healthy controls (2, 3). A survey of 2,596 people with FM identified balance problems as one of the top 10 most debilitating symptoms, with a reported prevalence of 45% (4).
The motor control problems displayed by patients with FM (5) have been suggested to be associated with specific clinical findings, such as reduced muscle strength, sensory or motor deficits, and suboptimal muscular coordination (2). The peripheral and central communication system impairments in these patients can also give rise to vestibular signalling dysfunctions (6). In fact, impaired balance in FM could be due to an altered perception or interpretation of audio-vestibular signals (7). It has also been suggested that FM affects dynamic balance control, as examined with dynamic posturography, with up to 34% of FM subjects scoring below the fifth percentile for population norms on sensory organization conditions (8). Again, this may be due to altered somatosensory inputs to the central nervous system.
There is now fairly strong evidence that exercise is effective in the treatment of the signs and symptoms associated with FM, and in improving patients’ overall physical condition (9). Regular resistance training is advised as an effective intervention to counter reduced motor ability, as a consequence of a reduction in strength, power, muscle mass, bone mass, and postural stability. However, despite the limitations reported above, balance training is generally not included in FM treatment.
Given that patients with FM have impaired balance and are at a higher risk of falling, it follows that one of the major therapeutic objectives should be to stimulate the neuromuscular system in order to develop their proprioceptive capacity. To this end, researchers have begun to explore the effects of a wide range of exercise techniques that extend beyond more conventional exercise training modes. In recent years whole-body vibration (WBV) training has raised interest for its potential benefits.
WBV is considered an efficient alternative for administering conventional resistance training to older individuals, which would also avoid excessive load on lower limb joints (10). Numerous studies have considered the effect of WBV on balance and functional mobility (11–16), showing that WBV had significant positive effects on balance, minimizing age-related functional decline, and restoring functional independence in elderly people (17). However, there is not yet consensus in the literature on WBV training, and its effectiveness should be accepted with caution (18). The literature reports are mixed, and inconsistent results are found. Some studies found little or no effect on postural control following WBV training (10, 19, 20).
Although the efficacy of WBV training on neuromotor function in older adults remains controversial (21), some authors have suggested that the improvement in these outcomes could be ascribed either to an enhancement of neuromuscular performance, in terms of improved muscle reflex (11, 12, 22) or to neurogenic adaptation, such as better synchronization of motor unit activation. It has been argued that greater synchronization of motor unit activity is in response to the vibrations or increased muscle spindle activation (23), which may be important, as these mechanisms are also responsible for the automatic postural response (24, 25).
Although some trials have demonstrated positive effects of WBV, the converse has also been reported (10, 11, 14, 21, 22, 26). A major reason for the inconsistency in the results of WBV could be the heterogeneity in study designs, a range of different WBV protocols are used in the literature. Furthermore, the patient population used in different studies varies (for example with respect to disability level), which may influence the response to treatment. Despite this, some preliminary research has suggested the potential benefit of WBV in populations with different chronic diseases (21, 27), and although WBV has been used in the treatment of a number of disorders (14, 28), few studies have specifically addressed its potential benefits for the treatment of FM syndrome. A number of researchers have combined WBV with traditional physical exercise programmes, reporting improvements both in FM symptoms (pain and fatigue) and in overall quality of life (29–31), but to our knowledge little research has addressed the efficacy of WBV as a means of improving balance and maintaining stability in patients with FM (32, 33). Gusi et al. (32), with 3 weekly WBV sessions comprising 6 sets of 45–60 s at 12.5 Hz, reported improvements in balance using a short-term WBV programme, Sañudo et al. (33) reported similar results with WBV combined with traditional exercise after a 6-week programme (3 sets of 45 s at 20 Hz–3 mm and 4 sets of unilateral squats at 20 Hz–2mm). The few published studies note the ability of WBV to improve dynamic balance, although the mechanisms of action are not well understood (32). Further studies are therefore needed in order to determine how specific balance interventions can improve motor control and postural balance impairments in FM.
Gusi et al. (32) have emphasized the importance of developing new studies to assess different vibratory devices (i.e. those with tilt or up and down mechanisms). It is also important to note that in both Gusi’s and Sañudo’s studies a rotational platform was used and, to date, no studies have analysed the effect of vertical platforms in this population group. Sañudo et al. (33) also highlighted that the addition of co-interventions makes it difficult to evaluate the contribution of each individual therapy, therefore a more ideal study design may involve each study group performing identical exercises on a WBV unit, with one group receiving vibration with or without additional physical exercise and the other not. The current study addresses this gap in the literature and aims to compare the effectiveness of an 8-week traditional exercise programme supplemented or not with WBV in order to improve body balance and physical function in women with FM.
Methods
Participants
Women (n = 46) who met the American College of Rheumatology criteria for classification of FM (34) were recruited to the study from physician practices and local FM support groups in Seville, Spain. Participants were randomly assigned by using a computer-generated random number sequence to either an exercise training group with WBV (WBVEX; n = 15), exercise group (EX; n = 15), or usual-care control group (CG; n = 16). Randomization was undertaken by a member of the research team not directly involved in the recruitment or assessment of patients (C. R.–B.). In addition, the randomization sequence was not disclosed to the researcher responsible for the day-to-day running of the trial (B.S.) until the patients had completed their baseline assessments. None of the participants had previous experience with vibratory training and were excluded if they had 1 or more possible contraindications for a WBV intervention (acute hernia; thrombosis; diabetes; epilepsy; metabolic or neuromuscular diseases; osteoporosis; osteoarthritis; orthopaedic injuries and prosthesis). Participants with respiratory or cardiovascular diseases that prevent physical exertion, or those taking drugs that could interfere with balance control, were also omitted. Finally, women with FM who were receiving psychological or physical therapy were excluded to avoid possible interactions with the present trial. This research was carried out according to the Declaration of Helsinki of the World Medical Association and was approved by the University of Seville Research Ethics Committee.
Sample-size calculation
The primary outcome measure for this study was change in overall stability index (OSI) at the 8-week point. In a previous pilot study conducted in our laboratory (33) improvements of 1.13 (standard deviation; SD 1.12) in OSI after combined exercise training and WBV in patients with FM were reported, representing a 17% change from baseline. On this basis, sample-size calculations indicated that 16 participants in each group were needed to show an improvement in OSI score of this magnitude, using a power of 0.8 and an alpha level of 0.05.
Outcome measures
Body balance assessment. Body balance assessments were performed using a Biodex F1c Stability System (BSS; Biodex, Inc., Shirley, NY, USA), which consists of a dynamic balance platform that allows simultaneous movements around the anterior-posterior (AP) and medio-lateral (ML) axes. The reliability and validity of the BSS has been demonstrated previously, with research reports demonstrating intra-class correlation coefficients (ICC) ranging from 0.43 to 0.95 for the BSS (34–36), with OSI reported as the most reliable measure of dynamic balance. The BSS measures, in degrees, the tilt about each axis during dynamic conditions and calculates a Medio–Lateral Stability Index (MLSI), an Anterior–Posterior Stability Index (APSI), and an OSI, which is a composite of the MLSI and the APSI. The BSS also calculates the mean position for the patient during all motions throughout the test, which is referred to as the Mean Deflection (MD).The Anterior–Posterior Mean Deflection (APMD) and the Medio–Lateral Mean Deflection (MLMD) were included as dependent variables. A higher score in all these outcomes indicates poorer balance.
The BSS device has 8 levels of stability (1–8); it is more difficult to maintain balance at level 1 than at level 8. All measurements were performed at the fifth level of stability, which has previously been reported to be appropriate in this patient group (33). In order to assess balance, patients were asked to stand on the BSS device for 1 min. During the assessment period, the platform began to move freely and simultaneously calculate the degree of tilt about both axes (AP and ML). All postural balance measurements were repeated 3 times and the mean was used for the analysis. The tests were performed in two different phases; in the first phase, patients kept their eyes open (visual control) and in the second phase, participants kept their eyes closed.
Lower-body dynamic strength. In order to determine the lower-body dynamic strength, participants were asked to perform as many repetitions as possible of a half squat exercise (using a multipower device with guided weight) in 1 min quantified by the system of measurement of dynamic forces T-FORCE system® (Ergotech Consulting, Spain). Prior to assessment of the test, subjects underwent a familiarization session in order to practice proper lifting technique. The movement begins from a standing position, and participants were asked to bend their knees to 120º flexion and then return to the upright position.
Procedures
Participants were randomly assigned to the WBVEX and EX groups performed twice-weekly exercise sessions of 45–60 min duration for 8 weeks. Each session (community-based supervised intervention) included 10 min of warm-up activities (slow walking, and gentle movements of progressive intensity, e.g. arm swinging); 10–15 min of aerobic exercise at 65–70% of maximal heart rate (HRmax), 15–20 min of muscle strengthening exercises (1 set of 8–10 repetitions for 8 different muscle groups, with a load of 1–3 kg), and 10 min of flexibility exercises (1 set of 3 repetitions for 8–9 different exercises, maintaining the stretched position for 30 s). Strengthening and flexibility exercises focused on the main areas of pain in patients with FM (deltoids, biceps, neck, hips, back and chest). In addition WBVEX participants performed 3 individual-based WBV training sessions per week using a vibrating platform (Power Plate, North America Inc., Northbrook, USA). Participants were asked to stand on the platform on 2 legs, with both knees in 120º isometric knee flexion, as measured by a goniometer and with the trunk upright. Participants were then exposed to a vibration frequency of 30 Hz and a peak to peak displacement of 4 mm (71.1 m/s-2 ≈ 7.2 g). To ensure maximum comfort all subjects wore sport shoes for the vibration exercises. The intensity of vibration was chosen based on previous literature, where 30 Hz has been shown to induce maximal muscular electrical activity (37). Each session consisted of 6 sets of 30 s, with 45-s recovery between sets (with participants standing with both feet on the platform), and 4 sets of 30 s of unilateral (i.e. single-leg) static squats. Participants completed 30 s of the exercise with the right leg and then immediately completed 30 s on the left leg, and this was considered one set. The vibration intervention progressed as indicated in Table I. The assessment of all outcomes was performed before and after the 8-week intervention in all groups.
|
Table I. Progression of the whole-body vibration training |
|
|
Weeks 1–2 |
Weeks 3–4 |
|
1. 6 × 30 s/45 s rest (bilateral squat) 2. 4 × 30 s/45 s (unilateral squat) |
1. 7 × 30 s /45 s rest (bilateral squat) 2. 5 × 30 s/45 s (unilateral squat) |
|
Weeks 5–6 |
Weeks 7–8 |
|
1. 8 × 30 s /45 s rest (bilateral squat) 2. 6 × 30 s/45 s (unilateral squat) |
1. 9 × 30 s /45 s rest (bilateral squat) 2. 7 × 30 s/45 s (unilateral squat) |
Statistical analysis
All analyses were performed using PASW 19.0 software (SPSS Inc., Chicago, IL, USA). Mean and standard deviations were calculated for each variable. A normal distribution of quantitative data was assessed by means of the Kolmogorov–Smirnov test (p > 0.05). Baseline features were compared between groups, using analysis of variance (ANOVA) test for continuous data, and χ2 test of independence for categorical data. An intention-to-treat analysis of covariance (ANCOVA) was used to assess differences between groups, with the pre-intervention value as covariant, group as the inter-group variable, and the post-intervention value as dependent variable. The statistical analysis was conducted at a 95% confidence level. In all analyses a p-value lower than 0.05 was considered as statistically significant.
RESULTS
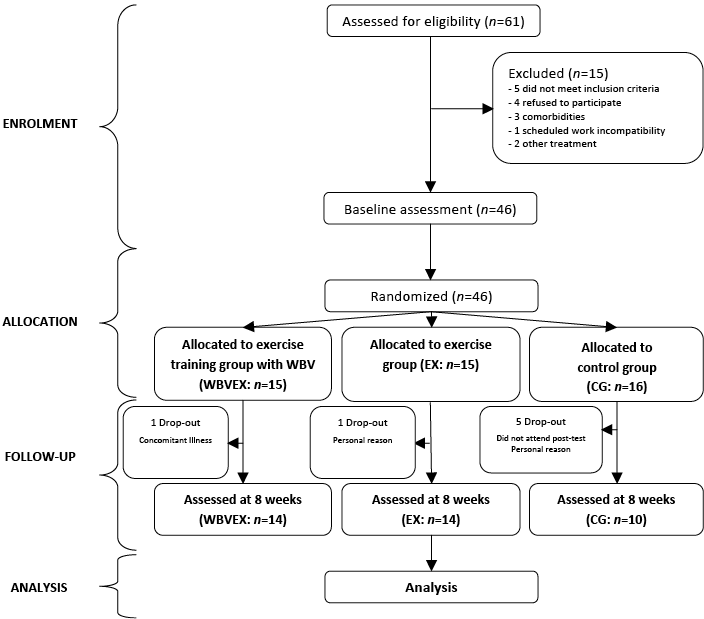
A total of 38 women completed the 8-week intervention and were included in the analysis. One patient in the WBVEX group, one in the EX and 5 in the CG group dropped out of the study. Reasons for drop-out included the following: illness (2), personal reasons (2), and, in the CG, 4 patients were lost to follow-up and did not complete the trial (Fig. 1). Hence, follow-up data were available for 38 women, whose characteristics are presented in Table II. Compliance with the exercise interventions was excellent, with women in the WBVEX group attending a mean of 31 of 40 (77%) sessions and women in the EX group attending 19 of 24 (79%) sessions. Groups were comparable at baseline with respect to age, weight, and height. In addition, at baseline there were no between-group differences in any outcome measures (all p-values > 0.05), except for MLMD with open eyes between both experimental groups (p = 0.02). Table III summarizes pre- and post-intervention data for all groups.
Fig. 1. Flow of participants through the trial. Enrolment, randomization and retention of study sample.
|
Table II. Sociodemographic characteristics of patients with fibromyalgia by treatment group |
|||
|
Characteristics |
WBVEX (n = 15) |
EX (n =15) |
CG (n = 16) |
|
Age, years, mean (SD) |
57.15 (6.80) |
62.28 (9.83) |
55.55 (7.90 |
|
Height, cm, mean (SD) |
156.02 (5.27) |
156.66 (7.89) |
157.81 (4.78) |
|
Weight, kg, mean (SD) |
73.02 (2.26) |
71.97 (8.23) |
71.91 (10.63) |
|
Marital status, n (%) |
|||
|
Single |
– |
1 (6.7) |
1 (6.3) |
|
Married |
9 (60) |
8 (53.3) |
10 (62.5) |
|
Separated |
3 (20) |
2 (13.3) |
3 (18.7) |
|
Widow |
3 (20) |
4 (26.7) |
2 (12.5) |
|
Education level, n (%) |
|||
|
University degree |
1 (6.7) |
– |
– |
|
Diploma |
7 (46.7) |
5 (33.3) |
8 (50.0) |
|
Compulsory school |
6 (40.0) |
8 (53.3) |
7 (43.7) |
|
None |
1 (6.7) |
2 (13.3) |
1 (6.3) |
|
Employment status, n (%) |
|||
|
Retired |
2 (12.3) |
1 (6.7) |
1 (6.3) |
|
Disability pension/sick leave |
3 (20.0) |
2 (13.3) |
3 (17.7) |
|
Employed |
3 (20.0 |
4 (26.7) |
5 (31.3) |
|
Not working |
7 (46.7) |
8 (53.3) |
7 (45.7) |
|
Duration of symptoms, years, mean (SD) |
8.5 (7.4) |
9.2 (8.3) |
8.8 (8.2) |
|
SD: standard deviation; WBVEX: whole-body vibration exercise group; EX: exercise group; CG: control group. |
|||
|
Table III. Effects of 8 weeks of whole-body vibration training on dynamic balance and lower-limb physical function in women with fibromyalgia. Analyses are on an intention-to-treat basis |
||||||
|
Intention-to-treat |
WBVEX |
Experimental group |
Control group |
|||
|
Pre-test Mean (SD) |
Post-test Mean (SD) |
Pre-test Mean (SD) |
Post-test Mean (SD) |
Pre-test Mean (SD) |
Post-test Mean (SD) |
|
|
Overall SI OE |
7.02 (3.66) |
5.75 (2.51) |
5.53 (1.49) |
6.10 (1.40) |
6.17 (1.93) |
6.36 (2.01) |
|
Mean DEF OE |
5.85 (3.18) |
4.67 (2.09) |
4.58 (1.32) |
4.99 (1.16) |
4.94 (1.65) |
5.36 (1.67) |
|
AP SI OE |
5.36 (2.90) |
4.92 (2.18) |
4.46 (1.36) |
5.03 (1.21) |
4.85 (1.75) |
4.58 (1.06) |
|
AP MD OE |
2.47 (2.24) |
2.48 (1.29) |
2.18 (1.67) |
2.40 (1.08) |
1.98 (1.19) |
1.90 (0.93) |
|
ML SI OE |
4.54 (2.56) |
2.94 (1.44) |
3.35 (1.17) |
3.83 (1.37) |
3.93 (1.12) |
4.05 (2.14) |
|
ML MD OE |
2.28 (1.08) |
1.31 (0.21) |
1.23 (1.66) |
0.76 (0.19) |
0.70 (0.18) |
1.04 (0.30) |
|
Overall SI CE |
9.91 (3.64) |
9.10 (2.99) |
9.31 (1.83) |
8.89 (1.95) |
8.46 (2.83) |
9.58 (3.54) |
|
Mean DEF CE |
8.43 (3.55) |
7.76 (2.83) |
7.90 (1.77) |
7.63 (1.80) |
7.19 (2.54) |
8.36 (3.36) |
|
AP SI CE |
7.68 (2.58) |
7.32 (2.47) |
7.31 (1.93) |
7.30 (1.84) |
6.60 (2.19) |
6.68 (2.34) |
|
AP MD CE |
1.90 (2.01) |
3.18 (2.27) |
3.21 (2.66) |
3.87 (2.38) |
2.54 (1.95) |
1.84 (1.09) |
|
ML SI CE |
6.39 (2.86) |
5.48 (2.03) |
5.81 (1.49) |
5.21 (1.21) |
5.41 (2.15) |
6.98 (2.67) |
|
ML MD CE |
1.09 (0.87) |
1.80 (1.02) |
1.62 (1.02) |
0.95 (0.84) |
1.06 (0.95) |
1.49 (1.52) |
|
NUM REPS |
30.85 (8.90) |
31.14 (7.18) |
23.72 (7.98) |
23.50 (6.63) |
24.00 (6.24) |
19.83 (6.12) |
|
SI: stability index; MD: mean deflection; AP: anteroposterior; ML: medial-lateral; OE: open eyes; CE: closed eyed. NUM REPS: number of squats performed in 1 min with a 30% body weight load; WBVEX: whole-body vibration exercise group. |
||||||


Balance assessment has an intrinsic variability, thus the standard error of measurement (SEM) was calculated with pre-intervention data of the whole sample (SD/√ sample size) for all the variables in order to determine if group differences could be provoked by an inherent error of the balance data (low levels of SEM indicate high levels of score accuracy). SEM had significantly lower values than changes obtained after training, which suggests that these changes were induced by the intervention and not related to an inherent error of the equipment. In Table III it can be seen that the 8-week intervention of exercises and WBV resulted in a statistically significant improvement in MLSI, and Bonferroni-adjusted post-hoc comparisons between all 3 groups indicated statistically significant differences for the WBVEX over the EX group (p = 0.014) and over the CG (p = 0.029), when the eyes were open. In addition, significant improvements were noted in MLMD with open eyes. Table IV shows that the effect size of these improvements was large for MLSI (R2 = 0.29) and MLMD (R2 = 0.32). No other statistically significant difference in the balance outcomes was found.
|
Table IV. Inter-group comparison using analysis of covariance analysis |
|||||
|
SEM |
Power |
F |
p-value |
Effect size (η2) |
|
|
Overall SI OE |
0.41 |
0.068 |
2.390 |
0.106 |
0.120 |
|
MD OE |
0.36 |
0.081 |
2.223 |
0.123 |
0.113 |
|
AP SI OE |
0.33 |
0.074 |
0.953 |
0.396 |
0.052 |
|
AP MD OE |
0.28 |
0.063 |
0.420 |
0.660 |
0.023 |
|
ML SI OE |
0.28 |
0.283 |
7.432 |
0.002* |
0.292 |
|
ML MD OE |
0.15 |
0.387 |
7.537 |
0.002* |
0.320 |
|
Overall SI CE |
0.45 |
0.059 |
0.116 |
0.890 |
0.007 |
|
MD CE |
0.43 |
0.063 |
0.127 |
0.881 |
0.007 |
|
AP SI CE |
0.36 |
0.066 |
0.098 |
0.907 |
0.006 |
|
AP MD CE |
0.38 |
0.423 |
2.329 |
0.114 |
0.127 |
|
ML SI CE |
0.36 |
0.201 |
0.299 |
0.743 |
0.017 |
|
ML MD CE |
0.15 |
0.356 |
0.673 |
0.517 |
0.037 |
|
NUM REPS |
0.46 |
0.702 |
2.396 |
0.112 |
0.166 |
|
SI: stability index; MD: mean deflection; AP: anteroposterior; ML: medial-lateral; OE: open eyes; CE: closed eyed. NUM REPS: number of squats performed in 1 min with a 30% body weight load. SEM: standard error of measurement. Effect size (eta squared): > 0.01 small; > 0.06 medium; > 0.14 large. *p < 0.05. |
|||||
Regarding lower-limb strength, non-significant differences were found in the number of repetitions performed in 1 min at baseline. However, after the 8-week intervention, significant inter-group differences were found between the WBVEX and the CG. While the participants in the experimental groups with or without vibration training remained stable, participants in the CG experienced deterioration in this outcome (17.37%), although inter-group differences were not found.
DISCUSSION
The aim of this study was to assess the changes in body balance and functional performance following an 8-week exercise programme supplemented or not with WBV in patients with FM. This study showed that, compared with the CG, the WBVEX group presented improved functionality and balance after the exercise and WBV programme.
To our knowledge, this study was the first to investigate the effectiveness of an 8-week WBV and exercise programme on postural control in women with FM using a synchronous vibration platform. Subjects were trained using a widely adopted commercial vibrating platform, and postural control was assessed by means of BSS. WBV is known to provide significant sensory stimulus, activating the muscle spindles and the sensory receptors of the skin, which are responsible for the muscle contraction. This temporary increase in the muscle activity may also improve proprioception (38). These mechanisms are also the primary sensory inputs used for postural orientation in space and for automatic postural response (24, 25).
We now have evidence of the effects of both synchronous and side-alternating vibration (which may or may not be combined with physical therapy) on body balance and physical function in elderly populations (11, 12, 14–16). These groups underwent vibration 3–5 times/week for 3–6 min (frequencies 12–30 Hz) for 6 weeks to 3 months, and although significant improvements were reported in chair-rising times (16), balance and gait (11–13, 15), there are several inconsistencies regarding the dose–response relationship. It may be the case that greater benefits of WBV training on balance ability might be obtained if these parameters are correctly combined (15).
Previous studies reported that, after 12 weeks, women with FM who performed WBV training (12.5 Hz–3 mm; 3 times per week) demonstrated improvements in dynamic balance that were not seen in control patients who maintained usual daily activities (32). Recently, our group of researchers also investigated the effects of a combined exercise/vibration programme (aerobic, strengthening, and flexibility exercises twice weekly, plus WBV training consisting of bilateral and unilateral static squats performed on a side-alternating vibration platform 3 times weekly) or a traditional exercise programme (33). The group engaged in the 6-week traditional exercise programme with supplementary WBV improved their MLSI, suggesting WBV may impart additional balance benefits when combined with traditional mixed exercise programmes. This is consistent with the results reported in the current study, where MLSI and MLMD improvements were seen when performed with open eyes. The maintenance of balance depends on the interaction of multiple sensory systems. One possible explanation for the lack of effect with closed eyes may be the lack of peripheral-central communication and the disturbances in vestibular signalling suggested in FM (6), which may have limited the effects of WBV. Furthermore, the training programme was conducted with opened eyes and only the assessment was carried out with modified visual input; therefore, no specific adaptations with closed eyes were expected.
These additional benefits achieved in this study may be due to differences in the type of platform utilized. The one used in this study oscillates uniformly up and down, in contrast to the platform used in the previous studies, where the WBV platform oscillates through the medial axis. With rotational vibration, the platform rotates about an anterior-posterior axis; consequently, positioning the feet further apart results in increased amplitude of movement and applies force asynchronously to the left and right foot. With vertical platforms the vibration is spread vertically and symmetrically, causing simultaneous movement of the lower extremities in the same direction.
It is interesting to note that only improvements in medio-lateral stability with open eyes, but not in the anterior–posterior sway, were found in the current study. One possible reason for these findings could be (as reported above), that the type of vibration selected for this study (synchronous vibration) instead of the side-alternating vibration, employed in the aforementioned studies may be different and may selectively influence the electromyographic activity (EMG) of the affected muscles. Side-alternating vibration is capable of producing the highest EMG activities, and moderate vibrations in the X-direction have been demonstrated, while synchronous vibration induced very stable vibration patterns (which moved only in the vertical direction) (39). In fact, previous studies reported non-significant effect using the device manufactured by Powerplate, which generates synchronous WBV (10, 19, 20). It was hypothesized that the added instability from side-alternating vibrations may pose a more challenging training condition for medio-lateral postural control (40); however, the findings of this study demonstrated that improvements in this axis can also be achieved with synchronous WBV. Given the findings in the literature and the current study, the question that arises is why none of the studies have reported benefits in anterior–posterior sway. Again, the possible reason may be that the acceleration in the Z-direction with both vibratory platforms is low. Studies assessing the changes in the position while performing the exercises are warranted, as all studies investigating balance in standing on both legs reported no significant results. Conversely, all studies evaluating single-leg-standing balance favoured WBV (40).
WBV training has also been associated with increased muscle strength in the lower limbs (13, 15). Previous researchers have demonstrated that women with FM exhibit reduced functional performance and lower limb muscle strength (3, 41, 42), which has also been related to reduced postural control and balance confidence (2). Reduced muscle strength influences functional activities and has been identified to modify the risk of falls (43). Góes et al. (3) determined the relationship between muscle strength and falls in women with FM, and reported deficits in lower limb muscle strength, balance and agility in 16 women with FM compared with 16 healthy controls. However, some researchers have found improvements in balance and motor control (one-legged stance) in response to multimodal exercise programmes with a significant strength training load for patients with FM (44); these strengthening effects were also reported after 6-weeks’ exercise/WBV training in this patient group (31, 33). The results of our current study showed that participants in the WBVEX group did not improve their lower-limb physical function after the intervention, which might be due to a remodelling of the central balance control circuits rather than to strength gains.
The current study is limited by the sample size related to the primary outcome, at the end-point of the study only 38 participants were available for evaluation. This large attrition figure (17%) should be taken into consideration when determining sample size at the outset in future studies. When evaluating the benefits of exercise for people with FM, it is important to consider possible adverse effects of exercise, such as an increase in symptoms (e.g. pain, stiffness and fatigue) and musculoskeletal problems. This study, however, demonstrated that WBV training is a safe (no adverse effects), suitable (no drop-outs due to the intervention) and effective (increased lower-limb muscle strength) way to exercise the musculoskeletal system, and potentially a feasible intervention for those patients who cannot participate in conventional strength training. Despite the limitations of this study, the improvements recorded in postural balance are encouraging, and suggest that WBV may be a viable alternative to exercise training to improve body balance among people with FM.
AcknowledgementS
This research was supported by funds from the Andalusian Center of Sport Medicine and the University of Seville (project no. 2009/00001546).
References
