Niko Wasenius, MSc1, Teppo Karapalo, MSc2, Tuulikki Sjögren, PhD3, Mika Pekkonen, MD, PhD2 and Esko Mälkiä, PhD3
From the 1Department of General Practice and Primary Health Care, Institute of Clinical Medicine, Faculty of Medicine, University of Helsinki, Helsinki, 2Peurunka Medical Rehabilitation Center, Laukaa and 3Department of Health Sciences, Faculty of Sport and Health Sciences, University of Jyväskylä, Jyväskylä, Finland
OBJECTIVE: To determine the intensity and volume of therapeutic exercises during a standard 13-day inpatient neck rehabilitation course in relation to overall physical activity in rehabilitation and everyday life.
DESIGN: Cross-sectional study.
METHODS: Subjects (n = 19; 16 women and 3 men; mean age 48.6 years, standard deviation (SD) 6.6) with chronic non-specific neck pain were recruited from two inpatient neck rehabilitation courses. Intensity and volume of therapeutic exercises and physical activity were measured in metabolic equivalents (METs) with an objective measurement device and all-time recall questionnaire. Maximum oxygen uptake was determined in METs (METc) by direct maximal cycle ergometer.
RESULTS: Subjects’ mean METc was 7.2 METs (SD 1.4) or 25.3 ml/kg/min (SD 4.8). Intensity of all therapeutic exercises was 1.9 METs or 27 %METc (SD 5.1) and volume 7.7 MET-hours/week. Intensity of specific neck and shoulder exercises was 2.0 METs or 28 %METc (SD 5.4) and volume 2.5 MET-hours/week. In addition, subjects were more active in everyday life than in inpatient rehabilitation.
CONCLUSION: The therapeutic exercise dose failed to reach previously reported target values for pain relief. The dose of therapeutic exercises and confounding physical activity should be carefully controlled in pain rehabilitation programmes.
Key words: physical activity; exercise therapy; metabolic equivalent; physical fitness.
J Rehabil Med 2013; 45: 300–307
Correspondence address: Niko Wasenius, Louhenkatu 4-6 A 5 FI-08100, Lohja, Finland. E-mail: niko.wasenius@helsinki.fi
Accepted Oct 24, 2012; Epub ahead of print Feb 13, 2013
INTRODUCTION
Therapeutic exercise is a subcategory of physical activity, including all bodily movements produced by skeletal muscle contraction resulting in energy expenditure (1–3). The dose of physical activity and its subcategories, including occupational, commuting, leisure-time, therapeutic exercises, miscellaneous home and gardening and sleep, is determined according to the mode/type, intensity, frequency, and duration of the activity (3). These dose characteristics can also be expressed with the concepts of type/mode, intensity and volume (3), because the volume is a product of the intensity, frequency, and duration (3). The dose of therapeutic exercises should be analysed in respect of other physical activity subcategories, as they may include activities that affect or confound the outcome of a specific exercise intervention (3–6).
A few studies have produced detailed dose-response analyses and suggested that active therapeutic exercises are effective in alleviating chronic neck pain and cervicogenic headache (7–10). In these studies the physical dose of intervention was expressed in metabolic equivalents (1 METs = oxygen consumption of 3.5 ml/kg/min = 1 kcal/kg/h) in proportion to overall physical activity, in order to control for the impact of the non-intentional training-like daily activities (7–9). These findings indicated that neck muscles require specific physiological training, which exceeds the effective metabolic-rate threshold and contains biomechanically-effective movements, to cope with neck problems and pain (7, 11). Whether these thresholds are reached in the clinical setting remains unknown.
Therefore, the main aims of this pilot study were: firstly, to measure the dose of therapeutic exercises during inpatient neck rehabilitation in relation to subjects’ maximal physical capacity; second, to determine whether the therapeutic exercises during rehabilitation reach the previously suggested thresholds for pain relief (7, 8), and, finally, to compare physical activity profiles during rehabilitation and everyday life.
METHODS
Subjects
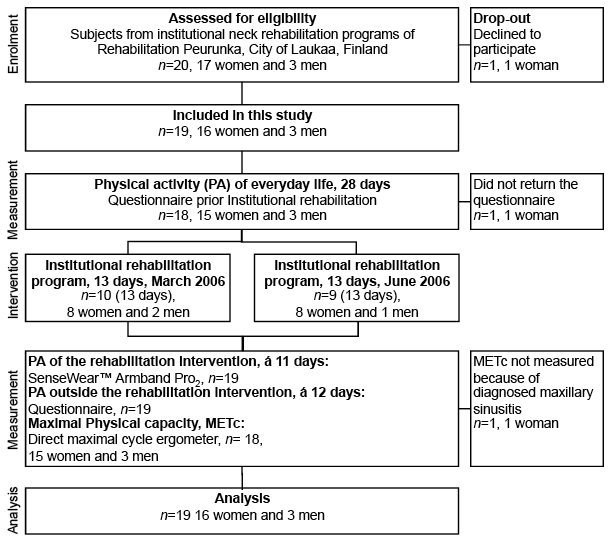
This cross-sectional pilot study utilized data from a normal, real-life, multidisciplinary institutional rehabilitation programme for individuals with chronic neck pain at Peurunka Medical Rehabilitation Center (Peurunka, Laukaa, Finland). Altogether, 19 out of 20 eligible subjects, 16 women and 3 men (age range 36–57 years), were recruited from two institutional rehabilitation programmes conducted between March 2006 (n = 10) and June 2006 (n = 10) (Fig. 1). One eligible female subject declined to participate in the study. The sample size was reasoned to be sufficient for a thoroughly physiological analysis of the rehabilitation programme. A power calculation was not performed, because the purpose of the study was not to investigate the effectiveness of the programme.
The inclusion criteria for the neck rehabilitation programme were set by the Social Insurance Institution of Finland (KELA) (12): neck and shoulder pain > 3 months or symptoms that repeatedly weakened their working or functioning ability, physical overload or ergonomic problems induced by work, psychological stress related to the symptoms, or radiating symptoms in the upper extremities. The KELA authorities decided whether a subject was eligible for the neck rehabilitation programme, based on the subject’s application, including a statement from the medical doctor. Eligibility was considered individually in relation to the guidance criteria given above. The subjects’ characteristics are shown in Table I. The ethics committee of the University of Jyväskylä approved the study and all subjects gave their written informed consent.
Fig. 1. Flow-chart of design, subjects, and main outcome measurements.
|
Table I. Demographic and clinical characteristics of the subjects |
||||
|
All (n = 19) |
Women (n = 16) |
Men (n = 3) |
pa |
|
|
Age, years, mean (SD) |
48.6 (6.6) |
48.6 (7.1) |
48.3 (4.0) |
0.736 |
|
VO2max, ml/kg/minb, mean (SD) |
25.3 (4.8) |
25.4 (5.3) |
24.6 (2.1) |
0.813 |
|
METcb, METs, mean (SD) |
7.2 (1.4) |
7.2 (1.5) |
7.0 (0.6) |
0.858 |
|
BMI, kg/m2, mean (SD) |
26 6 (3.7) |
25.9 (3.9) |
27.4 (2.9) |
0.371 |
|
Fat percentb, mean (SD) |
29.3 (5.0) |
30.0 (5.1) |
25.4 (0.4) |
0.139 |
|
VAS pain scale, 0–10 cmc, mean (SD) |
4.5 (2.6) |
4.9 (2.4) |
2.3 (3.2) |
0.114 |
|
Depression Scale, 0–30c, mean (SD) |
5.8 (5.4) |
5.8 (5.4) |
4.3 (2.5) |
0.974 |
|
Work Ability Index, 7–49d, mean (SD) |
26.4 (5.8) |
26.4 (5.8) |
33.0 (4.0) |
0.051 |
|
Oswestry Index, 0–100%c, mean (SD) |
11.3 (7.0) |
11.3 (7.0) |
14.7 (5.0) |
0.247 |
|
Physical resources, 0–10c, mean (SD) |
6.9 (1.7) |
6.9 (1.7) |
6.3 (2.9) |
0.963 |
|
Mental resources, 0–10c, mean (SD) |
7.5 (1.9) |
7.5 (1.9) |
8.0 (1.0) |
0.965 |
|
Subjective work ability, 0–10c, mean (SD) |
6.8 (1.8) |
6.8 (1.8) |
7.7 (1.5) |
0.390 |
|
Neck pain related disability, 0–10c, mean (SD) |
6.1 (1.9) |
6.1 (1.9) |
5.0 (4.4) |
0.423 |
|
Cervicobrachial syndrome, n |
8 |
7 |
1 |
|
|
Cervicalgia, n |
5 |
4 |
1 |
|
|
Migraine, n |
4 |
4 |
||
|
Cervical spondyloarthrosis, n |
3 |
3 |
||
|
Cervical disc prolapse, n |
2 |
2 |
||
|
Thoracic outlet syndrome (suspected), n |
2 |
2 |
||
|
Bruxism, n |
1 |
1 |
||
|
Cervical disc degeneration, n |
1 |
1 |
||
|
Diffuse idiopathic skeletal hyperostosis, n |
1 |
1 |
||
|
Dystonia, n |
1 |
1 |
||
|
Fibromyalgia (suspected), n |
1 |
1 |
||
|
Fractured clavicula, n |
1 |
1 |
||
|
Hypomobile thoracic spine, n |
1 |
1 |
||
|
Osteoporosis (suspected), n |
1 |
1 |
||
|
Scoliosis (cervical-thoracic spine), n |
1 |
1 |
||
|
Supraspinatus syndrome/acromioplastia, n |
1 |
1 |
||
|
Tension neck, n |
1 |
1 |
||
|
Acromio-clavicular joint arthralgia, n |
1 |
1 |
||
|
Cervical spondylosis, n |
1 |
1 |
||
|
aMen vs women (Mann-Whitney U test, p < 0.05 = statistically significant). bn = 18, 15 women and 3 men. cBest possible score (lower limit) – worst possible score (upper limit). dBest possible score (upper limit) – worst possible score (lower limit). BMI: body mass index; VAS: visual analogue scale; VO2max: maximal oxygen uptake; METc: VO2max in METs; METs: metabolic equivalent (1 MET: 3.5 ml/kg/min). |
||||
Intervention
The main goals of the intervention were: to alleviate pain and increase the subjects’ pain-coping skills; to improve and sustain working and functioning ability; to provide self-directed rehabilitation approaches; and to promote a healthy lifestyle. The intervention was based on the best information available on neck rehabilitation, according to the framework set out by the standard of institutional rehabilitation in Finland (12). The content of the rehabilitation programmes included baseline examinations by the medical doctor and physiotherapist and physical capacity tests (e.g. muscle strength and UKK-2-km walk test). The baseline measurements did not affect the content of the rehabilitation programme. In addition, subjects had group discussions with a psychologist (1 × 60 min) and physiotherapist (3 × 60 min), lectures (e.g. coping with pain), individual treatments (1 × 45 min + 1 × 30 min of therapeutic exercise), massage (3 × 45 min), relaxation (3 × 45 min). The intervention, also included ergonomics lectures and training (3 × 60 min), functional exercises (1 × 120 min), and group exercise sessions (aerobic exercise (2 × 90 min), swimming (1 × 60 min), therapeutic exercises (1 × 75 min), therapeutic exercises and stretching (5 × 90 min)). Furthermore, the programme was carried out according to standard clinical practice and no modification was made by the researchers. Thus, the programme was considered to reflect real clinical practice.
Measurements
At the beginning of the intervention, neck pain and related disability, physical and mental resources, and subjective estimate of working ability were measured with visual analogue scales (VAS) (0 cm = best possible score and 10 cm = worst possible score).
In addition, Work Ability Index (WAI, 7 = worst possible score and 49 = best possible score) (13) and Oswestry index (0% = best possible score and 100% = worst possible score) were calculated and subjects were screened for depression (Depression Scale; 0 = best possible score and 30 = worst possible score) (14).
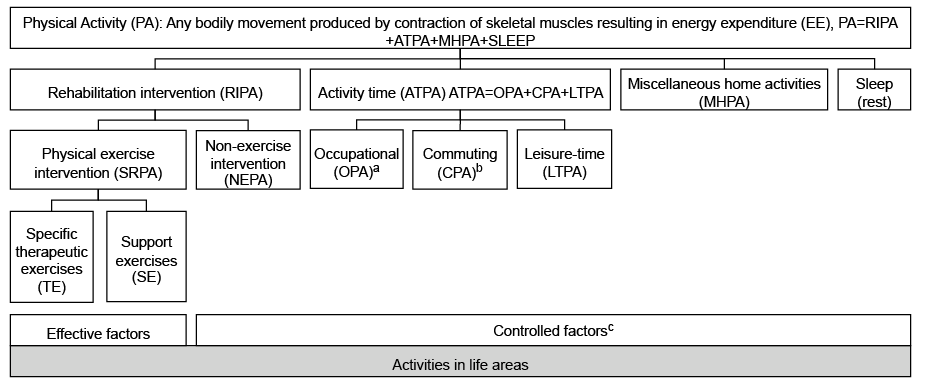
Four weeks prior to rehabilitation Occupational Physical Activity (OPA), Commuting Physical Activity (CPA), Leisure-Time Physical Activity (LTPA), Miscellaneous Home Physical Activities (MHPA; e.g. housework and gardening), and sleep were measured with an all-time questionnaire (Fig. 2). For each subject, a uniform instruction to complete the questionnaires was given. The questionnaire was completed accurately in diary manner during week 1, whilst during weeks 2–4 only changes in activities were recorded. This approach was chosen to make the questionnaire less demanding to complete. The questionnaire asked about activity type, duration, frequency, intensity and terrain geometry (e.g. while walking or cycling). Intensity was determined by external load or breathlessness and/or sweating (15). The questionnaire was analysed with MetPro®-physical activity (PA) analysis programme. The reliability of the questionnaire using the MetPro®-PA analysis programme has been shown to be acceptable (kappa = 0.48–0.78; and intraclass correlation coefficient (ICC) = 0.91–0.94 for all activities and ICC = 0.62–0.76 for LTPA) (8, 15).
Fig. 2. Subcategories of physical activity (PA). aIn rehabilitation Occupational PA (OPA) included rehabilitation intervention activities. bIn rehabilitation Commuting PA (CPA) included transitions from accommodation to rehabilitation intervention activities. cConfounding factors if not accurately controlled.
During rehabilitation the all-time questionnaire was used daily to measure PA outside Rehabilitation Intervention (RIPA). The questionnaire was modified so that the commuting physical activities meant transitions from on-site accommodation to RIPA activities. RIPA comprised all the physical and psychosocial activities in the official rehabilitation programme and their energy expenditure (PA) and duration was measured with a SenseWear® Armband Pro2 (SWP2) (BodyMedia Inc., Pittsburgh, PA 15222, USA). Correlations between the energy expenditure estimated with the SWP2 and indirect calorimetry have been good (ICC = 0.51–0.89) (16, 17).
The SWP2 was worn on the back of the upper right arm to measure energy expenditure (kcal) through algorithms based on subjects’ characteristics and measurements of skin temperature, near body temperature, galvanic skin response, heat flux, and accelerations. Each subject was randomly assigned either one or two measurement days at the beginning of the RIPA. Type of RIPA activity was collected by diary entries made by two researchers. RIPA activities were classified into 3 categories: specific Therapeutic Exercises (TE); support movements (e.g. Nordic walking and aquatics); and other non-exercise intervention activities (all psychosocial rehabilitation activities). The specific therapeutic exercises comprised exercises that were targeted at specific muscle groups and further subdivided into neck and shoulder girdle exercises and other specific exercises (all trunk and leg exercises). All different exercises were guided by physical therapists. Because the SWP2 cannot be used in water the intensity of aquatic training during the RIPA was estimated according to METs measured by direct oxygen consumption analysis in the recent literature (18). Altogether, 147 different activities, of which 104 were physical exercises (including aquatic training), were measured during the rehabilitation intervention with SWP2. A mean of 15.1 (SD 10.8) activities were measured from each subject. The content of the physical exercises executed during the rehabilitation intervention is presented in Table II.
|
Table II. Content of the physical exercise intervention during the rehabilitation intervention |
||||||||
|
Type |
Exercises |
Equipments |
Number of exercises |
Load, kg |
Repetitions/set |
Sets |
Duration, min, |
METs |
|
Specific neck and shoulder girdle exercises |
Neck and shoulder girdle |
Elastic rubber band |
13 isometric |
20 |
1–2 |
3.0 (3.0) |
1.0–1.8 (1.2) |
|
|
Dumb-bells |
12 dynamic |
2–10 |
15–20 |
1–2 |
4.4 (2.6) |
1.1–4.6 (2.7) |
||
|
Resistance equipments |
15 dynamic |
2–26 |
10–20 |
1–2 |
3.9 (1.6) |
1.1–3.4 (2.2) |
||
|
Stretching |
Body weight |
5 |
3.0 (1.2) |
1.0–1.4 (1.2) |
||||
|
Other specific exercises |
Trunk and leg |
Body weight |
15 dynamic |
12–40 |
1–2 |
3.7 (1.6) |
0.8–4.5 (1.8) |
|
|
Elastic rubber band |
1 isometric |
2 |
4.0 (1.0) |
(2.5)b |
||||
|
Free weights |
2 dynamic |
1.5 |
10 |
1 |
1.5 (0.7) |
1.3–1.4 (1.4) |
||
|
Resistance equipments |
12 dynamic |
15–85 |
4–20 |
1–2 |
4.5 (4.9) |
1.0–3.6 (2.1) |
||
|
Resistance equipments |
2 isometric |
2.0 |
1 |
4.0 (1.4) |
2.6–2.6 (2.6) |
|||
|
Stretching trunk and leg |
Body weight |
3 |
1–2 |
4.0 (4.0) |
0.9–1.7 (1.2) |
|||
|
Stretching sessions |
Body weight |
7 |
1–2 |
19.0 (19.0) |
1.6–3.9 (2.4) |
|||
|
Support movements |
Nordic walking, walking, rowing, aerobics, warm-ups, aquatic training |
Body weight (mainly) |
17 |
37.8 (26.4) |
2.2–5.5 (3.5) |
|||
|
Total |
|
|
104 |
|
|
|
12.1 (18.1) |
0.8–5.5 (2.2) |
|
aExercise duration includes both the exercise and recovery between sets. dRange cannot be calculated (data from 1 measured exercise). SD: standard deviation; METs: metabolic equivalents (1 MET: 3.5 ml/kg/min). |
||||||||
The basic time window for PA measurements was 1 min for both questionnaires and SWP2 measurements. In the questionnaires, the 1-minute time-window was achieved by advising the subjects to report the minutes used for a particular activity, rather than using a specific cut-off point to indicate when to report an activity, such as > 10-min. In rehabilitation, and some other activities, shorter activity periods can include anaerobic phases that produce Excess Post-exercise Oxygen Consumption (EPOC). We reasoned that this is not a problem with non-sporting people in the calculation of mean metabolic rate of even less than 1 min. Resistance exercise bouts with an equal work volume have been shown to produce similar exercise oxygen consumption to that of high-intensity exercise (85% 8-repetition maximum (RM)) and low-intensity exercise (45% 8-RM). Higher intensity will produce a greater EPOC in magnitude and volume, but this levels over time (19, 20). In addition, the measured oxygen consumption has been used to calculate METs for 1-minute activities (21, 22).
The energy expended (kcal) on different activities measured with the SWP2 was converted into METs by dividing the energy expenditure (kcal) of the activity with subject’s theoretical resting metabolic rate (kcal) (0.0035 l/min × 4.9 (caloric equivalent) × body weight (kg)). The data collected with questionnaires and measures were transformed into METs with the MetPro®-PA analysis program. Transformations were performed using an extensive database, approximately 2,000 different activities, in which previously published MET-values are integrated and harmonized (19, 23–25), and using the data obtained from the SWP2 measurements executed during RIPA.
The MetPro® program was also used to calculate the Time-Weighted Average Intensity (TWA-MET = 1–T n∑i=1 Miti , where Mi is the MET value for activity i, ti is the duration of activity i in minutes, and T the duration of the measured activity cycle, i.e. the sum of the partial durations ti), maximum intensity or peak intensity in any activity cycle (Max-MET), and volume (MET-hours (METh) = n∑i=1, where Mi is the MET value for activity i, ti is the duration of activity i in hours) of the different activity cycles. Calculation of TWA-MET is similar to PAL (Physical Activity Level), which describes the mean energy expenditure in a day (24 h) and are most often used in nutrition studies. TWA-MET, however, is not limited to 24-h time-period as is PAL.
Maximum oxygen uptake (VO2max) was measured in METs, i.e. maximum physical capacity (METc), by direct maximal cycle ergometry (Ergoline 900, Ergo-line GmbH + Co KG, Ergometriesysteme, Bitz, Germany) at the beginning of the intervention (26). The physical strain of PA was expressed as the percentage of TWA-MET and Max-MET of maximum physical capacity (%METc) or maximum physical capacity reserve (%METcR). The formula was used to calculate physical strain as %METcR [3]:
|
(TWA–MET or Max–MET–1MET) |
× 100 |
|
(METc–1MET) |
All the volume results were proportioned to a week (7 days) as follows:
|
METh of measurement days |
× 7 days |
|
measurement days |
Statistical analysis
The results are expressed as means and standard deviations (SD), or with a 95% confidence intervals (95% CI). Variables were considered normally distributed if the absolute value of skewness or kurtosis fell inside the limits of twice the standard error. Statistical comparison between related samples was made with the Wilcoxon signed-rank test and between the unrelated samples with Mann-Whitney U test. A p-value < 0.05 was considered statistically significant. Statistical analyses were carried out with SPSS (version 15.0) (SPSS Inc., Chicago IL, USA).
RESULTS
The METc of the subjects was 7.2 METs (SD 1.4) or 25.3 ml/kg/min (SD 4.8). Maximal oxygen uptake (VO2max) was lower than the mean reference values for 68% (9/15 women and 3/3 men) of the subjects (27).
TWA-MET during activity time was 2.5 METs (SD 0.6) in everyday life, resulting in a physical strain of 36 %METc, whereas in rehabilitation it was 2.4 METs (SD 0.2) or 34 %METc. Max-MET during activity time was 6.4 METs (SD 1.8) or 89.6 %METc in everyday life and 7.2 METs (SD 1.9) or 97 %METc in rehabilitation. No significant differences were found between everyday life and rehabilitation in TWA-MET and Max-MET during activity time. Activity time included OPA or rehabilitation intervention PA, CPA or transitions PA, and leisure-time PA (Fig. 2). For 53% (9/17) of the subjects the physical strain at work exceeded the proposed upper tolerance limit for physical overload (≥ 30 %METc) (28).
The total volume of PA was significantly (p < 0.01) higher in everyday life (290.2 MET-hours/week, SD 33.8) than in rehabilitation (265.8 MET-hours/week, SD 18.8). No significant difference (p > 0.05) was detected in the total volume of individual activities that exceeded the ≥ 50 %METc physical strain level in everyday life (62.6 MET-hours/week, SD 43.8) and rehabilitation (62.3 MET-hours/week, SD 21.1). In everyday life, however, the total volume accumulated more steadily throughout categories of life areas compared with rehabilitation (Table III).
|
Table III. Time-weighted average intensity (TWA-MET) and volume of physical activities (PA) that exceeded the individual physical strain level of ≥ 50% METc in different life areas in everyday life and in institutional neck rehabilitation |
|||||||
|
Categories of PA |
Everyday life (n = 17) |
Rehabilitation (n = 18) |
pa |
||||
|
TWA-MET (METs) Mean (SD) |
Volume (MET-hours/week) Mean (SD) |
% |
TWA-MET (METs) Mean (SD) |
Volume (MET-hours/week) Mean (SD) |
% |
||
|
OPA or RIPAb |
3.6 (1.4) |
18.5 (25.9) |
30 |
4.7 (0.4) |
20.2 (4.9) |
32 |
|
|
CPAc |
2.4 (2.3) |
3.1 (7.8) |
5 |
3.5 (1.4) |
2.6 (3.8) |
4 |
|
|
LTPA |
5.0 (2.4) |
20.5 (16.3) |
33 |
5.7 (1.1) |
36.8 (16.1) |
59 |
|
|
MHPA |
4.3 (1.6) |
20.6 (29.9) |
33 |
2.9 (1.7) |
2.7 (4.8) |
4 |
|
|
Total |
|
62.6 (43.8) |
100 |
|
62.3 (21.1) |
100 |
0.435 |
|
aTotal volume in everyday life compared with rehabilitation (Wilcoxon’s signed-rank test, p < 0.05 = statistically significant). bOccupational PA in everyday life and RIPA in rehabilitation. cIn rehabilitation commuting included transitions from accommodation to intervention activities. METs: metabolic equivalent (1 MET = 3.5 ml/kg/min); MET-hours/week: sum of MET × time (h/week); SD: standard deviation; OPA: occupational PA; RIPA: rehabilitation intervention PA, CPA: commuting PA; LTPA: leisure-time PA; MHPA: miscellaneous home PA. |
|||||||
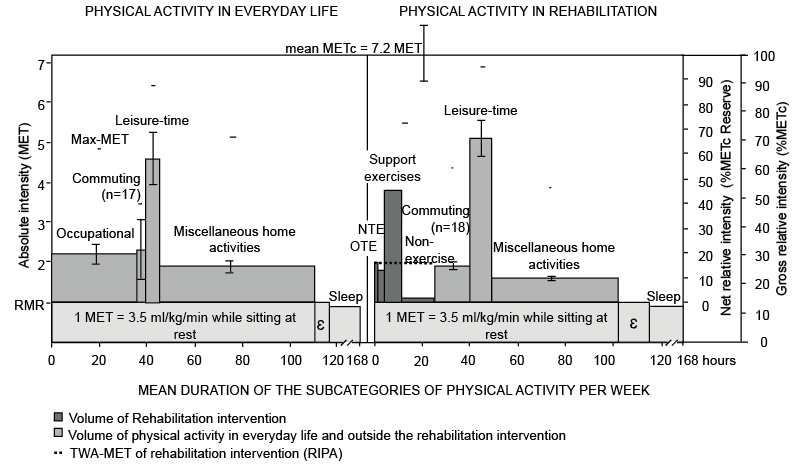
TWA-MET in rehabilitation intervention activities (RIPA) was 2.0 METs or 29 %METc (SD 5.5). TWA-MET of physical exercise executed during the RIPA (SRPA) was 3.1 METs or 45 %METc (SD 8.3). During TE, and in specific neck and shoulder girdle training, TWA-MET was almost the same, 1.9 METs or 27 %METc (SD 5.1) and 2.0 METs or 28 %METc (SD 5.4), respectively. The volume of the TE was 7.7 MET-hours/week, from which the specific neck and shoulder girdle training (2.5 MET-hours/week) accounted for 33% of that of the therapeutic exercises. Fig. 3 shows the intensity and volume relationships between intervention physical exercises and PA in different life areas in everyday life and in rehabilitation.
DISCUSSION
The present study investigated the possible physiological explanation for pain relief during a 13-day rehabilitation intervention following standard clinical practice (without any involvement of researchers in the actual rehabilitation process). The proportion of specific neck and shoulder girdle exercises of the total therapeutic exercise volume was found to be relatively minor (33%). In addition, the dose of specific therapeutic exercises executed during rehabilitation intervention did not reach the previously suggested target values for neck pain relief (7).
It has been suggested previously that the threshold value for decrease in moderate/severe neck pain (57 mm on VAS, 1–100 mm) (29) with specific exercises is 8.75 MET-hours/week with an intensity of 3.3 METs (7). It also has been reported that 15 weeks of light resistance training of 1.15 MET-hours/week with an intensity of 2.8 METs (30% VO2max) is sufficient, with guidance, to alleviate the intensity of mild/weak (30) headache and neck symptoms (1.1–1.6 on rating on the perceived pain scale (CR10, scale 0–10)) (8). In our study, the subjects had moderate neck pain (VAS 45 mm) (29), and the volume of specific exercises (7.7 MET-hours/week) was close to the effective threshold value, but the intensity was substantially lower (1.9 METs).
The lower absolute intensity in our study may indicate the difference in the intervention length. Longer interventions will result in higher average intensity, if training is progressive. At the beginning of the training, neck pain can also hinder the implementation of therapeutic exercises followed by a subsequent decrease in intensity. Therefore, to reach the target intensity levels, it seems to be necessary to perform specific exercises progressively even after the 13-day intervention. In addition, it can be argued, that the dose-response relationships may vary depending on the severity of the pain. Furthermore, pathophysiological differences in neck pain, as suggested by the vide variety of diagnoses and inter-individual variations in baseline functioning (Table I), may also modify the subjects’ responsiveness to the exercise. Thus, in clinical practice, but also in research, more emphasis should be placed on the individual, when treating/investigating complex disorders with multifaceted interventions.
It was also found that physical strain for 53% of the subjects exceeded the proposed upper tolerance limit for an 8-h working day (> 30 %METc) (28). To decrease occupational overload, it is necessary to achieve either decrease in the intensity of occupational activities or increase in the maximum physical capacity (METc). Based on the present findings, LTPA dose during the rehabilitation was sufficient to permit increase in METc, especially if continued after the 13-day institutional rehabilitation (26). To support the need for increase in METc, it was found that, for 68% of the subjects, the METc was lower than mean reference values (27). Increase in METc may, however, contribute only minimally to neck pain (31). Interestingly, one study (32) has also suggested that high occupational physical strain (> 30–35 %METc) is not an independent risk factor for neck and shoulder disorders (31). Recently Pedersen et al. (33) have, however, reported that the total weekly vigorous-intensity activity is positively correlated with right shoulder elevation strength and negatively correlated with days of having neck pain within the last 3 months. Although, these correlations were weak they do suggest that general physical activity of higher intensity can be protective against neck pain and physical weakening (33). Moreover, it has been proposed that dynamic exercise that activates multiple muscles increases movement variability, which may function as a mediator of exercise-induced benefits in chronic pain (34). Thus, increase in METc may contribute to neck pain, by enabling subjects to engage in a physically more active lifestyle, which can subsequently result in an increase in movement variability.
Institutional rehabilitation can provide time for LTPA and recovery. During the rehabilitation period subjects are accommodated at full board, which reduces the need for domestic or household tasks, and provides time for LTPA and recovery. This conclusion is supported by the present findings. It was found that in everyday life, 63% of the total volume (≥ 50 %METc) was executed during OPA and MHPA, whereas in rehabilitation 59% of the volume was executed during LTPA. In addition, the volume of overall physical activity in everyday life, basically as a result of high OPA and MHPA volumes, was higher than in rehabilitation. Moreover, previous research has suggested that gender imbalance (women > men) in domestic work is a vital factor in explaining gender differences in musculoskeletal disorders (35). Thus, rehabilitation may allow time for LTPA and recovery, because it provides surroundings with a lower MHPA dose, and OPA in everyday life is not totally compensated for by the daily programmed rehabilitation activities (RIPA) (7–9, 26).
This study has some limitations that should be considered when interpreting the results. It has been suggested that at least a 2-week measurement of physical activity is needed to even out the day-to-day variability (36). Notwithstanding the previous suggestion, we considered 1 week to be sufficient, because only minor changes were detected during the control period. In addition, the physical activity questionnaires are predisposed to subjectivity. The questionnaires utilized here were modified from the previous ones, which have been shown to be acceptably reliable (8, 15). Thus, within-subject comparisons were considered to be justified. Moreover, the usage of both questionnaires and objective method, may have introduced bias to the results. In exercise physiological studies, however, the data is often combined from multiple sources when investigating the change in physical activity (37, 38). One female subject was dropped from the physical strain analyses, because she was unable to take VO2max due to the maxillary sinusitis, possibly resulting in the overestimation of intensity of physical activities. In addition, the physical strain of some specific therapeutic exercises may have been underestimated, because the strain was expressed relative to METc of the body rather than METc of the individual muscle group (39, 40). Furthermore, the missing time was imputed (1 MET) for analysis of total physical activity volume (Fig. 3). The impact of imputation was estimated to be minor because: the percentage of the missing time was minor, both in everyday life (4%) and rehabilitation (8%); it is likely that the non-reported hours were low-intensity physical activities (more difficult to recall); and imputation of missing time is needed to allow a physiologically sound comparison. The RIPA dose was not measured separately for each individual, possibly resulting in underestimation or overestimation of interventions physical activity on the individual level. The RIPA, however, was mostly group rehabilitation with individually undefined external loads. Thus, the influence of the aforementioned generalization was estimated to be minor at the group level. Furthermore, the sample was relatively small and heterogeneous for results to be generalized and the sample consisted of an uneven number of men (n = 3) and women (n = 16), thus the effect of sex cannot be determined. Finally, it must be emphasized that the intervention may include rehabilitation activities other than therapeutic exercises, such as massage and psychological support, which may have an alleviating effect on neck pain.
Fig. 3. Comparison of intensity and volume of physical activity in relation to subjects’ (n = 19) maximal physical capacity in everyday life and in inpatient neck rehabilitation. METc: maximal physical capacity of subjects; MET: metabolic equivalent (1 MET = 3.5 ml·kg–1·min–1); Max-MET: maximum intensity in the physical activity subcategory; NTE: specific neck and shoulder girdle therapeutic exercises; OTE: other specific therapeutic exercises; RMR: resting metabolic rate; ε: physical activity not measured. Commuting in rehabilitation included transitions from accommodation to rehabilitation intervention activities. Shaded areas represent the volume of PA (MET-hours or MET-minutes = Σ (MET × time)) and height of the quadrangles indicate Time–Weighted Average intensity (TWA-MET).
In conclusion, the dose of specific exercise was lower than the previously suggested target values for neck pain reduction. In addition, pain rehabilitation programmes that included structured exercises should be more carefully customized to account for large inter-individual variability in the dose of everyday-life physical activity, functioning, and pathophysiology of neck pain. Individualization could enable more specific dosage of therapeutic exercises, identification of physical activity elements that are either constructive or harmful to health or well-being, and, thus more effective neck rehabilitation. Furthermore, this study demonstrates the difficulty of reaching the evidence-based exercise guidelines in practice. However, before evidence-based analyses, the rehabilitative dose, that is the intensity and volume physical activity, must be measured carefully and estimated with links to rehabilitation manoeuvres and symptoms.
Acknowledgements
Authors would like to thank Rauno Sauro, MSc, for maximal aerobic capacity tests and body composition assessments, Michael Freeman for checking the language of the manuscript, and the staff of Peurunka Medical Rehabilitation Center. This study was supported by collaboration project between University of Jyväskylä and Peurunka Medical Rehabilitation Center (JYPE-project). As a possible conflict of interest authors would like to state that Mr Mälkiä holds a decision-making position in SciReha Ltd.
REFERENCES
