Gabi Mueller, PhD1,3, Maria T. E. Hopman, MD, PhD4 and Claudio Perret, PhD2
From the 1Clinical Trial Unit, 2Institute of Sports Medicine, Swiss Paraplegic Centre, 3Swiss Paraplegic Research, Nottwil, Switzerland and 4Department of Physiology, Radboud University Nijmegen, The Netherlands
OBJECTIVE: To compare the effects of inspiratory resistance training and isocapnic hyperpnoea vs incentive spirometry (placebo) on respiratory function, voice, thorax mobility and quality of life in individuals with tetraplegia.
DESIGN: Randomized controlled trial.
Patients/methods: A total of 24 individuals with traumatic, complete tetraplegia (C5–C8, American Spinal Injury Association (ASIA) Impairment Scale; AIS A) were randomly assigned to 1 of 3 groups. They completed 32 supervised training sessions over a period of 8 weeks. Before and after the training period, the following tests were performed: body plethysmography, inspiratory and expiratory muscle strength, subjective breathing parameters using a visual analogue scale, voice measurements, thorax mobility and quality of life. Cohen’s effect sizes and Kruskal-Wallis tests for differences between pre- and post-training values were calculated.
RESULTS: Compared with placebo training, inspiratory resistance training showed high effect sizes for inspiratory muscle strength (d = 1.13), the subjective ability “to blow one’s nose” (d = 0.97) and the physical component of quality of life (d = 0.82). Isocapnic hyperpnoea compared with placebo showed a high effect size for breathlessness during exercise (d = 0.81). We found a significant effect of inspiratory resistance training vs placebo (p = 0.016) and vs isocapnic hyperpnoea (p = 0.012) for inspiratory muscle strength.
CONCLUSION: In individuals with motor and sensory complete tetraplegia during the first year post-injury, inspiratory resistance training is more advantageous than isocapnic hyperpnoea, performed 4 times a week for 10 min.
Key words: spinal injuries; breathing exercises; respiratory muscles; quality of life.
J Rehabil Med 2013; 45: 00–00
Correspondence address: Gabi Mueller, Clinical Trial Unit, Swiss Paraplegic Centre, Guido A. Zaechstr. 1, CH-6207 Nottwil, Switzerland. E-mail: gabi.mueller@paranet.ch
Accepted Sep 5, 2012; Epub ahead of print Feb 6, 2013

*This paper was presented as an oral presentation at the ISCOS (International Spinal Cord Society) and ASIA (American Spinal Injury Association) Annual Conference, 4–8 June 2011, in Washington DC, USA.
INTRODUCTION
Respiratory complications are the leading cause of death in individuals with spinal cord injury (SCI) (1). Haisma and colleagues (2) reported that the risk of pulmonary infections is 3.5 times higher for individuals with complete, compared with incomplete, lesions. The increased risk of pulmonary infections for individuals with motor complete tetraplegia seems to result from loss of respiratory muscle innervation and consecutive decrease in lung volume (3, 4). Another consequence of this loss of respiratory muscle innervation is an increasing stiffness of the thorax with increasing time post-injury, which further decreases lung function (4). Early initiation of respiratory muscle training after an SCI may delay stiffening of the thorax and therefore have a positive effect on respiratory function (5, 6) and may prevent respiratory complications (7). However, review articles on respiratory muscle training in individuals with SCI have shown that most studies are of low methodological quality and that there are not yet enough data to prove a positive effect of respiratory muscle training on respiratory function, respiratory complications or quality of life (8, 9). Most respiratory muscle training studies (5, 6, 10–12) have used a high training volume of approximately 30 min daily, which may jeopardize the motivation and compliance of patients in everyday situations. Therefore, a reduction in daily training time, but increased training intensity, may be advantageous to produce an effective training stimulus.
There exist different methods for respiratory muscle training in clinical practice, which can be grouped approximately into respiratory resistance (strength) and respiratory muscle endurance training methods. To our knowledge, no study has compared the effects of these two fundamentally different respiratory muscle training methods in individuals with SCI.
Therefore, the aim of this study was to conduct a randomized controlled trial to compare the effects of respiratory resistance and respiratory muscle endurance training with the effects of sham training (placebo) on respiratory function, voice, subjective breathing parameters, thorax mobility and quality of life in individuals with complete tetraplegia.
METHODS
This study was conducted as a randomized controlled trial with consecutive enrolment of subjects to group 1, 2 or 3 by the study coordinator, between February 2004 and October 2010 in a single SCI rehabilitation centre. The study was approved by the local ethics committee and written informed consent was obtained from each patient before the start of the study. Inclusion criteria were: individuals 18–65 years old, with a traumatic, motor and sensory complete tetraplegia between C5 and C8 (AIS A), 6–8 months post-injury. Exclusion criteria were: injuries of the lung or the thorax, or any other respiratory diseases. Details of enrolment, allocation, follow-up and analysis of participants are shown in the CONSORT (Consolidated Standards of Reporting Trials) flow diagram (Fig. 1). Sample size calculation was based on Pimax as main outcome parameter and clinical data on expected differences and standard deviations (SD) (i.e. SD 1.2 times the difference between treatments). For an 80% probability of detecting a treatment difference at a two-sided significance level of 0.05, the number needed to treat was 24.
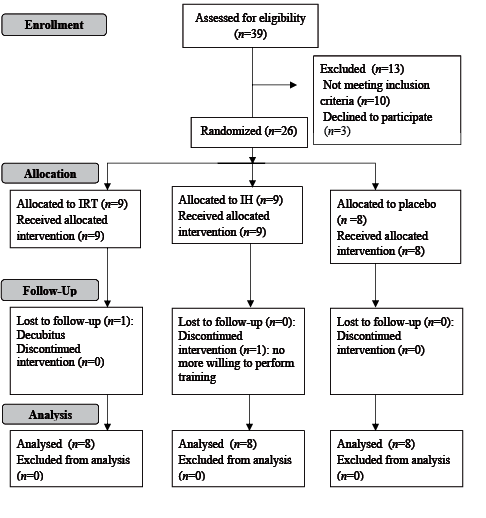
Fig. 1. CONSORT (Consolidated Standards of Reporting Trials) flow diagram of study participants from enrolment to analysis. IH: isocapnic hyperpnoea; IRT: inspiratory resistance training.
Respiratory muscle training
Patients were consecutively randomized to 1 of 3 study groups, as follows:
1. Inspiratory resistance training (IRT).
2. Respiratory muscle endurance training using isocapnic hyperpnoea (IH).
3. Placebo training using incentive spirometry (placebo).
All subjects completed 32 supervised training sessions (4 × ~10 min per week) over 8 weeks. The IRT group used an electronic inspiratory threshold device with visual feedback of achieved resistance, called Respifit S® (Eumedics GmbH, Purkersdorf, Austria). Subjects were instructed to inhale with maximal inspiratory power during each of 90 repetitions. Inhalations with less than 80% of the individual maximal inspiratory power had to be repeated. Maximal inspiratory power was assessed at the start of each training session (mean of the 3 highest values during the first 10 repetitions).
The IH group used a device called Spirotiger® (Idiag AG, Volketswil, Switzerland), which enables intensive hyperventilation through partial re-breathing of ventilated air, supported by visual and acoustic feedback of breathing volume and frequency. Subjects hyperventilated continuously for 10 min at 40–50% of their individual maximal voluntary ventilation (MVV) (13). The intensity of IH was increased over the 8 weeks of training by increasing breathing frequency by 1 breath/min every second or third training session.
The placebo group was instructed to perform “volume training” with an incentive spirometry device called Voldyne 5000® (Tyco Healthcare, Mansfield, UK). Subjects had to inhale 16 times from residual volume (RV) to total lung capacity (TLC) with 30–40 s of rest in between repetitions in order to reach a comparable training duration to the other 2 groups (~10 min). After each training session, subjects in all 3 groups had to indicate subjective training effort on a visual analogue scale (VAS).
Pre- and post-training tests
Before and after the 8 week’ training period, the following tests were performed:
1. Body plethysmography (Master Screen® Body, Viasys Healthcare GmbH, Hoechberg, Germany) in order to measure lung volumes and flows, such as TLC, RV, expiratory reserve volume (ERV), vital capacity (VC), forced expiratory volume during 1 s (FEV1), peak expiratory flow (PEF) and MVV over 12 s. Each manoeuvre was repeated at least 3 times until the 2 repetitions with the highest value were within 5%. The highest value of each parameter was used for analysis. The subject’s sitting position was standardized to the best possible position in the patient’s own wheelchair with abdominal binders (if any) removed.
2. Inspiratory and expiratory muscle strength measurements (Pimax, Pemax) (Micro RPM, Micro Medical, Hoechberg, Germany) were repeated at least 5 times until the 2 repetitions with the highest value were within 5%. The highest value of each parameter was used for analysis.
3. Subjective breathing parameters, such as coughing, secretion clearance, the ability to blow one’s nose and shortness of breath during exercise, were assessed using a VAS. Coughing, secretion clearance and the ability to blow one’s nose were defined as follows: 0 = not possible at all, 10 = possible without any problems. For breathlessness during exercise, 0 was defined as no breathlessness during intensive exercise (e.g. climbing a ramp in a manual wheelchair), whereas 10 was defined as one has to stop exercising because of breathlessness.
4. Voice measurements, such as loudness of voice (Voltcraft 320, Conrad Electronic SE, Hirschau, Germany) and sustained phonation time (stop-watch, TIMEX Ironman, North Little Rock, USA) were assessed 3 times each and the highest value of each parameter was used for analysis. For loudness of voice, we used the mean over 1 s (best second) and for sustained phonation time we controlled for constant loudness between the 3 repetitions.
5. An adapted Short-Form (SF)-12 quality of life questionnaire (14) was used to assess the physical and mental components of subjective quality of life.
6. Thorax mobility was measured in the supine position using computed tomography (Somatom Sensation 40; Siemens, Germany). At maximal inspiration and expiration, two images at the fourth and ninth vertebral body were recorded. Intra-costal areas and anterior–posterior distances from the sternum to the vertebral body were analysed manually. For further details on this method please refer to Mueller et al. (15).
To avoid any bias, especially concerning Pimax, Pemax measurements, data acquisition was carried out by a study nurse, whereas the respiratory training was supervised by a scientist. Moreover, for the post-training measurements the study nurse as well as the patients were blinded to baseline data.
Statistics
Differences between pre- and post-training values were calculated. Cohen’s effect sizes (pre- vs post-training values) for IRT or IH vs placebo as well as for IRT vs IH were calculated and used as a measure of clinically relevant changes. An effect size of < 0.5 represents a small effect, 0.5–0.8 a medium effect, and > 0.8 a great, clinically relevant effect. Furthermore Kruskal–Wallis tests with Mann–Whitney U post-hoc tests were used to compare IRT or IH vs placebo using SPSS 18.0. The significance level was set at p < 0.05.
RESULTS
A total of 24 subjects were included and analysed in this study (Fig. 1). Subjects’ characteristics are presented in Table I. There were no significant differences in any baseline data between the groups (Table II). Mean differences between pre- and post-test values for all measured parameters are presented in Table III. There was a positive influence of IRT on inspiratory muscle strength (Fig. 2). The changes pre- vs post-training resulted in a significant effect of IRT vs placebo (p = 0.016) and IRT vs IH (p = 0.012). Pre- vs post-training changes between the tested training methods did not have a significant effect on the other respiratory function parameters, voice measurements, subjective breathing parameters, thorax mobility or quality of life.
Effect sizes for IRT vs placebo, IH vs placebo and IRT vs IH are presented in Table IV.
|
Table I. Subjects’ characteristics for the 3 study groups |
||||||||
|
Group |
Lesion level (n) |
TPI Months Mean (SD) |
Age Years Mean (SD) |
Height, m Mean (SD) |
Body mass, kg Mean (SD) |
Gender Male/ female n |
Smoking, pack-years Mean (SD) |
Physical activity, h/week Mean (SD) |
|
Placebo |
C5 (3) C6 (3) C7 (2) |
6.6 (1.4) |
41.6 (17.0) |
1.75 (0.07) |
71 (6) |
6/2 |
11 (18) |
9.6 (2.9) |
|
IH |
C5 (4) C6 (3) C7 (1) |
6.6 (0.9) |
33.5 (11.7) |
1.78 (0.06) |
72 (6) |
6/2 |
9 (21) |
10.1 (1.9) |
|
IRT |
C5 (4) C6 (2) C7 (1) C8 (1) |
6.0 (0.0) |
35.2 (12.7) |
1.75 (0.07) |
70 (14) |
6/2 |
7 (10) |
10.1 (1.6) |
|
TPI: time post-injury; IH: isocapnic hyperpnoea; IRT: inspiratory resistance training; physical activity: sports therapy, physiotherapy and respiratory muscle training; SD: standard deviation. |
||||||||
|
Table II. Absolute mean baseline data (standard deviation; SD) of the 3 study groups |
|||
|
Parameter |
Placebo Mean (SD) |
IH Mean (SD) |
IRT Mean (SD) |
|
Lung function TLC, l RV, l ERV, l VC, l FEV1, l PEF, l/s MVV, l/min Respiratory muscle strength Pimax, cmH2O Pemax, cmH2O Voice measurements Sustained phonation time, s Loudness of voice, dB VAS parameters, 0–10 Coughing Secretion clearance Ability to blow one’s nose Breathlessness during exercise Quality of life (SF-12), units Physical part Mental part Thorax mobility T4 anterior–posterior diameter, mm T4 intra-thoracic area, cm2 T9 anterior–posterior diameter, mm T9 intra-thoracic area, cm2 |
5.8 (1.1) 3.0 (1.0) 0.3 (0.2) 2.4 (0.8) 2.2 (0.5) 4.4 (1.1) 80.4 (21.4) 69.4 (20.4) 61.8 (39.6) 11.0 (4.9) 91. (13.2) 4.6 (2.7) 3.6 (3.5) 5.7 (3.8) 9.5 (1.0) 40.4 (7.5) 48.3 (12.4) 13.9 (17.0) 43.3 (45.0) 11.7 (9.2) 46.7 (35.0) |
5.5 (1.1) 3.1 (1.0) 0.3 (0.3) 2.3 (0.7) 2.0 (0.7) 4.5 (1.5) 75.8 (21.3) 69.4 (29.9) 58.8 (20.4) 12.2 (3.4) 92.3 (5.4) 4.5 (2.2) 4.1 (2.8) 3.0 (1.9) 9.3 (1.2) 45.4 (4.0) 55.1 (5.4) 10.2 (7.2) 30.6 (23.7) 9.4 (7.7) 43.2 (43.6) |
5.5 (0.9) 2.6 (0.6) 0.3 (0.3) 2.9 (1.0) 2.4 (0.7) 4.7 (1.5) 84.3 (27.6) 66.1 (30.6) 55.5 (30.4) 12.8 (8.3) 99.6 (6.5) 2.9 (2.4) 2.7 (3.2) 2.6 (1.9) 8.5 (2.6) 42.1 (7.2) 53.4 (4.1) 14.0 (12.2) 49.1 (40.9) 12.6 (10.8) 47.8 (35.0) |
|
IH: isocapnic hyperpnoea; IRT: inspiratory resistance training; TLC: total lung capacity; RV: residual volume; ERV: expiratory reserve volume; VC: vital capacity; FEV1: forced expiratory volume in 1s; PEF: peak expiratory flow; MVV: maximal voluntary ventilation; Pimax: maximal inspiratory pressure; Pemax: maximal expiratory pressure; VAS: visual analogue scale; T4: fourth thoracic vertebra; T9: ninth thoracic vertebra. |
|||
|
Table III. Mean change (standard deviation; SD) (absolute values) from pre- to post-training values for each training group |
|||
|
Parameter |
Placebo Mean (SD) |
IH Mean (SD) |
IRT Mean (SD) |
|
Lung function TLC, l RV, l ERV, l VC, l FEV1, l PEF, l/s MVV, l/min Respiratory muscle strength Pimax, cmH2O Pemax, cmH2O Voice measurements Sustained phonation time, s Loudness of voice, dB VAS parameters, 0–10 Coughing Secretion clearance To blow one’s nose Breathlessness during exercise Quality of life (SF-12), units Physical part Mental part Thorax mobility T4 anterior-posterior diameter, mm T4 intra-thoracic area, cm2 T9 anterior-posterior diameter, mm T9 intra-thoracic area, cm2 |
–0.25 (0.81) –0.48 (0.57) 0.06 (0.22) 0.32 (0.45) 0.21 (0.32) 0.57 (0.94) 6.95 (14.62) 8.88 (15.21) 3.25 (13.27) 0.57 (3.33) 2.92 (2.99) 0.89 (3.41) 1.78 (4.05) –0.53 (2.73) –2.16 (3.06) –2.75 (6.40) 4.10 (5.47) 4.00 (4.42) 1.47 (18.14) 0.25 (7.68) 1.22 (38.95) |
0.18 (0.34) –0.35 (0.31) 0.05 (0.25) 0.34 (0.31) 0.26 (0.26) 0.44 (0.49) 15.96 (15.10) 7.00 (10.03) 8.50 (39.41) 1.69 (5.37) 1.90 (6.47) –0.05 (1.56) 0.13 (1.18) 1.04 (1.85) –0.29 (1.12) 2.23 (7.45) –1.67 (4.58) 4.24 (4.34) 1.54 (18.87) 1.64 (4.80) –1.14 (48.25) |
0.10 (0.76) –0.39 (0.84) 0.13 (0.22) 0.46 (0.44) 0.42 (0.44) 1.18 (1.22) 16.28 (17.45) 35.38 (29.43)* 7.50 (14.73) 2.73 (6.21) –0.79 (6.31) 1.08 (1.47) 0.67 (1.94) 1.71 (1.80) 0.03 (2.65) 1.63 (4.05) –1.45 (4.61) 3.03 (5.48) 0.26 (8.59) 3.70 (3.52) 0.57 (10.97) |
|
*Significant difference compared with placebo and IH (p < 0.05). IH: isocapnic hyperpnoea; IRT: inspiratory resistance training; TLC: total lung capacity; RV: residual volume; ERV: expiratory reserve volume; VC: vital capacity; FEV1: forced expiratory volume in 1s; PEF: peak expiratory flow; MVV: maximal voluntary ventilation; Pimax: maximal inspiratory pressure; Pemax: maximal expiratory pressure; VAS: visual analogue scale; T4: fourth thoracic vertebra; T9: ninth thoracic vertebra. |
|||
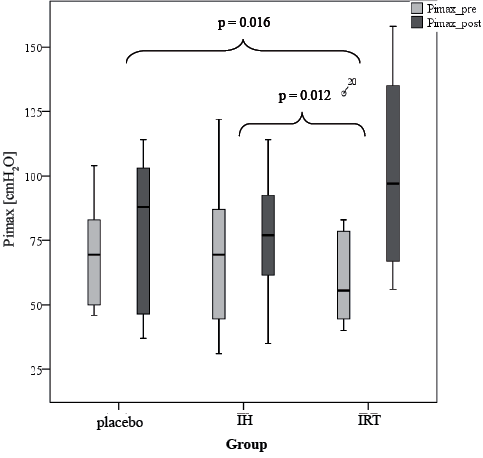
Fig. 2. Box-plots of pre- and post-training inspiratory muscle strength (Pimax) for the 3 study groups. Please note that p-values are calculated based on differences between pre- and post-training values. IH: isocapnic hyperpnoea; IRT: inspiratory resistance training; Pimax_pre: maximal inspiratory muscle strength before the start of the training phase; Pimax_post: maximal inspiratory muscle strength after the training phase.
|
Table IV. Comparison of effect sizes for pre- to post-training changes between the groups |
|||
|
Parameter |
IRT vs placebo |
IH vs placebo |
IRT vs IH |
|
Lung function TLC RV ERV VC FEV1 PEF MVV Respiratory muscle strength Pimax Pemax Voice measurements Sustained phonation time Loudness of voice VAS parameters Coughing Secretion clearance To blow one’s nose Breathlessness during exercise Quality of life (SF-12) Physical part Mental part Thorax mobility T4 anterior-posterior diameter T4 intra-thoracic area T9 anterior-posterior diameter T9 intra-thoracic area |
0.43 0.12 0.35 0.31 0.55 0.55 0.58 1.13 0.30 0.43 –0.75 0.07 –0.35 0.97 0.77 0.82 –1.10 –0.19 –0.85 0.58 –0.22 |
0.68 0.30 –0.04 0.05 0.19 –0.18 0.61 –0.15 0.18 0.25 –0.20 –0.35 –0.55 0.67 0.81 0.72 –1.14 0.06 0.04 0.22 –0.54 |
–0.14 –0.08 0.37 0.31 0.43 0.80 0.02 1.29 –0.03 0.18 –0.42 0.75 0.33 0.37 0.16 –0.10 0.05 –0.25 –0.87 0.49 0.49 |
|
Bold numbers indicate high effect sizes. IRT: inspiratory resistance training; IH: isocapnic hyperpnoea; TLC: total lung capacity; RV: residual volume; ERV: expiratory reserve volume; VC: vital capacity; FEV1: forced expiratory volume in l/s; PEF: peak expiratory flow; MVV: maximal voluntary ventilation; Pimax: maximal inspiratory pressure; Pemax: maximal expiratory pressure; VAS: visual analogue scale; T4: fourth thoracic vertebra; T9: ninth thoracic vertebra. |
|||
DISCUSSION
The high effect sizes for IRT vs placebo regarding Pimax, the subjective parameter of the ability to blow one’s nose and the physical component of subjective quality of life showed that IRT performed 4 times a week for 10 min is effective to improve respiratory function in individuals with AIS A tetraplegia during the first year post-injury.
Furthermore, there was a significant positive effect of IRT on inspiratory muscle strength (Fig. 2), despite a very low training volume compared with other respiratory muscle training studies that showed positive effects on respiratory muscle strength or lung volumes (5, 6, 11, 12). We believe that low training volumes, with, on the other hand, high training intensities, have positive effects on the motivation and consecutively on training compliance, especially if patients are to perform the training on their own initiative. Therefore, we recommend motivating patients to achieve the highest possible training intensity in each training session, since this seems to be important for an effective training stimulus. The high effect sizes of the subjective parameter “to blow one’s nose” and the physical component of SF-12 quality of life may help to enhance patient motivation.
Lung function and respiratory muscle strength
The significant improvement in Pimax after IRT may not be surprising for many readers of this journal. However, this is the first study showing a significant improvement with a very low training volume and the devices used for training and testing of inspiratory muscle strength were not the same (see methods), i.e. the IRT group had no advantage concerning customization to the device, compared with the other two groups. Of course, the learning effect of the inspiratory manoeuvre may have been higher in the IRT group compared with the other groups. However, this is a highly desired part of the training method, which cannot be excluded for testing and is highly desired as a training outcome.
We found a high effect size for IRT compared with IH regarding PEF (Table II). PEF is an important parameter for coughing (16) and thus for secretion clearance. Normal PEF values during coughing range from 6 to 20 l/s, and a minimum flow of 2.7 l/s is necessary to clear secretions (16, 17). Even though our subjects’ mean baseline values were above this minimum flow of 2.7 l/s (Table II), they did not reach the lower limit of normal flow rates. In the IRT group, PEF improved by 1.18 l/s, whereas the placebo and IH groups only showed an improvement of 0.57 and 0.44 l/s, respectively. The improvement in PEF in the IRT group may directly be related to the significant improvement in Pimax after the training period. Kang and colleagues (18) reported that peak cough flow, a parameter similar to PEF, is more closely related to Pimax than Pemax. They further stated that inspiratory capacity may be more important for an effective cough than expiratory muscle strength in individuals with complete tetraplegia (18). Higher inspiratory muscle strength increases diaphragmatic tension during inspiration, which causes higher elastic recoil during expiration and thus helps to enhance PEF.
Voice measurements
We performed voice measurements because the loudness of the voice and the sustained phonation time are measures that are important for the daily life of individuals with AIS A tetraplegia and that influence their quality of life. This may be crucial for motivating patients to perform respiratory muscle training on their own. Interestingly, we found a high negative effect size of IRT vs placebo regarding loudness of voice (Table IV), which means that placebo training showed a higher effect on loudness of voice than on IRT. We hypothesize, that a possible effect of placebo training may be improvements in coordination of the respiratory muscles and/or learned activation of accessory respiratory muscles of the neck (19). In contrast, sustained phonation time improved most in the IRT group (Table III).
Subjective parameters (VAS and quality of life)
There was a high effect size for the subjective ability “to blow one’s nose” after IRT compared with placebo (Table IV). This is in line with the improvement in Pimax and the slightly higher gain in lung volumes in the IRT group compared with the other groups (Table III). These results show that inspiratory muscle strength may also positively influence the ability to blow one’s nose, similarly to PEF. Since this is a subjective measure, it may also have a positive influence on the motivation of patients to perform such training. Furthermore, there was a high effect size for breathlessness during exercise after IH compared with placebo. This finding is not surprising, since IH has been shown to improve endurance exercise performance in wheelchair racing athletes (20).
Looking at the effect sizes for quality of life, there was a high value for the physical component of the SF-12 assessment after IRT compared with placebo (Table IV). Surprisingly, we found high negative effect sizes for the mental part of the SF-12 questionnaire for IRT vs placebo and IH vs placebo of –1.10 and –1.11, respectively (Table IV). This means that placebo training was advantageous to IRT and IH concerning the mental part of quality of life. Of course there are lots of other unknown factors influencing quality of life during inpatient rehabilitation after a SCI and we therefore have to be careful in interpreting these data. Nevertheless, we think that it is important also to assess quality of life, which is important for the patients, especially as there are not yet any data available concerning the effects of respiratory muscle training on quality of life (8).
Thorax mobility
Thorax mobility is an important parameter for follow-up measurements during long-term care of individuals with cervical SCI, because of increasing rib cage stiffness with longer time post-injury (4). We therefore wanted to evaluate whether mobility of the thoracic cage can be increased, or at least if stiffening can be delayed, by any of the respiratory muscle training methods we tested. Even though we found no significant improvements, we can at least conclude that rib cage mobility of all our 3 groups did not decrease during the 2 months of respiratory muscle training (Table III). Interestingly we found high negative effect sizes for the intra-thoracic area at the fourth thoracic vertebra after IRT vs placebo and vs IH. This suggests that the two training methods that request high breathing volumes (IH and placebo) may have positive effects on the accessory respiratory muscles of the neck, which help to elevate the upper ribs and therefore increase the intra-thoracic area at the T4 level. The accessory neck muscles become important inspiratory muscles, especially in individuals with tetraplegia, and the coordinated action of these muscles can be learned after a SCI (19).
Study limitations
None of the investigated respiratory muscle training methods showed any significant between-groups effect on lung volumes, flows, voice measurements and thorax mobility. This may have resulted from a concomitant spontaneous increase in all 3 study groups, since the study was conducted during the first year post-injury, where lung volumes and flows are known to increase over time (21). To prove spontaneous increases without any training, we would have to include a control group who did not perform any respiratory training or therapy. However, since we used subjective parameters, such as the VAS and the SF-12 quality of life questionnaire, in the present study, knowledge of doing no training would have had a negative influence on these important outcome parameters and may therefore not be a very good option in the context of this study.
Furthermore, with the present study we cannot conclude whether a higher training volume of approximately 30 min daily, as used in other studies with SCI individuals (5, 6, 10–12), would have had different or better effects than only 10 min of training 4 times a week. However, based on our long-lasting clinical experience in this field, we consider that even if a higher training volume had better effects, most tetraplegic individuals would not do this training on their own for a long time, due to lack of motivation. Therefore, we conclude that there is no need to evaluate a training method that would not be used in daily practice.
Conclusion
Pimax can be improved by high-intensity IRT in individuals with motor complete tetraplegia, despite a relatively low training volume. During the first year post-injury, 10 min of IRT performed 4 times a week is advantageous compared with the same volume of IH, for individuals with motor and sensory complete tetraplegia.
Acknowledgement
We thank Joerg Krebs for critically reading the manuscript.
REFERENCES
