OBJECTIVE: To determine whether regular interval training on a seated double-poling ergometer can increase physical capacity and safely improve performance towards maximal level in individuals with spinal cord injury.
METHODS: A total of 13 subjects with spinal cord injury (injury levels T5–L1) performed 30 sessions of seated double-poling ergometer training over a period of 10 weeks. Sub-maximal and maximal double-poling ergometer tests were performed before (test-retest) and after this training period. Oxygen uptake was measured using the Douglas Bag system. Three-dimensional kinematics were recorded using an optoelectronic system and piezoelectric force sensors were used to register force in both poles.
RESULTS: The mean intra-class correlation coefficient for test–retest values was 0.83 (standard deviation 0.11). After training significant improvements were observed in people with spinal cord injury in oxygen uptake (22.7%), ventilation (20.7%) and blood lactate level (22.0%) during maximal exertion exercises. Mean power per stroke and peak pole force increased by 15.4% and 23.7%, respectively. At sub-maximal level, significantly lower values were observed in ventilation (–12.8%) and blood lactate level (–25.0%).
CONCLUSION: Regular interval training on the seated double-poling ergometer was effective for individuals with spinal cord injury below T5 level in terms of improving aerobic capacity and upper-body power output. The training was safe and did not cause any overload symptoms.
Key words: exercise; oxygen consumption; paraplegia; ventilation.
J Rehabil Med 2012; 00: 00–00
Correspondence address: A. Bjerkefors, Biomechanics and Motor Control Laboratory, The Swedish School of Sport and Health Sciences (GIH), Box 5626, SE-114 86 Stockholm, Sweden. E-mail: anna.bjerkefors@gih.se
Submitted December 20, 2011; accepted May 29, 2012
Introduction
It is well-known that physical activity is crucial to avoid risks related to a sedentary lifestyle. In wheelchair-dependent individuals with paraplegia, over 80% would benefit from health-intervention programmes due to increased risks for cardiovascular diseases (1). Individuals can reduce the likelihood of secondary complications and/or enhance their physical capacity by including structured exercise activities in their daily schedule throughout their lives (2).
Exercise recommendations to increase physical capacity for people with chronic spinal cord injury (SCI) should be performed at a load of 60–65% oxygen uptake (VO2peak), 2–3 times per week for at least 20 min, with a heart rate corresponding to 60–80% of maximum during, for example, arm cranking or wheelchair ergometer training (3, 4).
A number of training devices have been specifically developed for people who are restricted to a sitting position. The most commonly used ergometer is probably the arm ergometer (5, 6), which requires little space and can be used with the person sitting in a wheelchair. A disadvantage is that arm ergometer training movement is in front of the body, which may increase the asymmetry between strong anterior musculature and weak posterior musculature. This may increase an asymmetry that is often already present as a result of many activities of daily living predominantly occurring in front of the body (7). A specifically designed ergometer should therefore ideally aim at engaging the posterior upper body muscles.
A seated double-poling ergometer (SDPE) has been developed and recently evaluated with a group of people with SCI (8). The results indicate that the SDPE appeared to be a suitable training tool; shoulder movement was within a range of motion not conducive to musculoskeletal injury and it provided a large range of controllable intensities enabling both endurance and strength training (8).
The aim of this study was to investigate whether 10 weeks of regular interval training on a SDPE can increase physical capacity, for example aerobic capacity and upper-body power output, in a group of individuals with SCI, and hence safely improve performance towards maximal level. Furthermore, the study aimed to assess the correlation between calculated power output and power output measured via the commercially available software on the ergometer, and to assess the correlation between oxygen uptake and power output.
Methods
Subjects
Individuals with SCI were recruited from a consumer organization. The inclusion criteria were: age range 18–70 years without diagnosed cardiovascular or lung disease or other diseases that could interfere with an intensive training programme. Thirteen healthy wheelchair users (8 males, 5 females; mean age 47 years (standard deviation (SD) 12), mean height 1.75 m (SD 0.08), mean weight 67.9 kg (SD 10.2) with SCI levels ranging from T5 to L1, volunteered for the study. Years post-injury varied from 3 to 35 (median 23). Nine persons had a complete injury (AIS A) according to the American Spinal Injury Association Impairment Scale and 4 an incomplete injury (AIS B and C). A detailed description of the participating individuals is presented in Table I. All participants received oral and written information about the study and provided written consent to voluntarily participate. The study was approved by the Stockholm Regional Ethical Committee.
|
Table I. Characteristics of the subjects with spinal cord injury
|
|
Subject
|
Age
|
Gender
|
Lesion level
|
ASIA Impairment Scalea
|
Years post-injury
|
Height
(m)
|
Body mass (kg)b
|
|
Before
|
After
|
|
I
|
49
|
M
|
T5
|
A
|
29
|
1.85
|
73.9
|
73.6
|
|
II
|
67
|
M
|
T5
|
A
|
14
|
1.73
|
67.7
|
67.8
|
|
III
|
45
|
M
|
T6
|
B
|
25
|
1.87
|
86.8
|
88.8
|
|
IV
|
45
|
F
|
T6
|
C
|
35
|
1.62
|
58.8
|
56.8
|
|
V
|
55
|
F
|
T5–8
|
C
|
15
|
1.74
|
59.8
|
58.4
|
|
VI
|
38
|
F
|
T9
|
A
|
25
|
1.72
|
64.1
|
65.1
|
|
VII
|
57
|
F
|
T9
|
C
|
33
|
1.70
|
70.9
|
71.2
|
|
VIII
|
43
|
M
|
T11
|
A
|
23
|
1.65
|
77.8
|
76.9
|
|
IX
|
45
|
M
|
T12
|
A
|
25
|
1.79
|
62.9
|
62.8
|
|
X
|
58
|
M
|
T12
|
A
|
14
|
1.79
|
76.8
|
75.3
|
|
XI
|
30
|
F
|
T12
|
A
|
13
|
1.67
|
46.2
|
45.8
|
|
XII
|
22
|
M
|
T12
|
A
|
3
|
1.79
|
69.3
|
69.3
|
|
XIII
|
55
|
M
|
L1
|
A
|
7
|
1.86
|
67.5
|
68.0
|
|
aASIA Impairment Scale, “A” represents complete impairment, i.e. no sensory or motor function in the S2-S4 segment, “B”, incomplete impairment with sensory but no motor function below the neurological level, and “C”, incomplete impairment, i.e. motor function with a muscle grade less than 3 below the neurological level (according to the International Standards for Neurological and Functional Classification of Spinal Cord Injury, American Spinal Injury Association, ASIA) (9).
bNo significant differences in body mass between before and after training values were found, from a mean of 67.9 kg (standard devation (SD) 10.2) to 67.7 kg (SD 10.6), respectively.
|
Training equipment
Four custom-built SDPE modified for persons with motor impairments in the lower extremities were used in the study (Fig. 1). A seat with adjustable backrest and foot brace was mounted on the ergometer to secure the sitting position. The flywheel and the display originally came from a commercially available kayak ergometer (Dansprint ApS, Hvidovre, Denmark) and resistance on the ergometer could be adjusted by regulating the air-intake on the flywheel from 1 (lightest) to 10 (heaviest). The resistance was set at 4 throughout this study, which was a suitable level for both male and female subjects to perform maximum exercise (8). The ergometer display presented the subjects’ power output (W), stroke rate (strokes/min), distance (m) and speed (m/s).
Fig. 1. Custom-built seated double-poling ergometer. To simplify the transition from wheelchair to ergometer and vice versa, an electric motor was mounted under the front part of the seat. Before transferring from the wheelchair to the ergometer, the seat was set in the same height as the wheelchair seat. When the subject was seated in the ergometer, the front part of the seat was elevated to a position that was suitable for the participant to perform an appropriate double-poling movement.
Intervention
The intervention consisted of 3 training sessions on the SDPE per week during a 10-week period for each subject. All training sessions were carried out in small groups coached by an instructor. A training session lasted approximately 50 min and included a warm-up, 4 interval sessions of 6–7 min and a cool-down. The intervals varied between 15 s and 3 min with rests of 15 s to 1 min. The training intensity of the intervals was determined to correspond to 70–100% peak heart rate, which had been obtained during the initial maximum oxygen uptake test. If a higher maximum heart rate was achieved during training, the intensity level was adjusted. Heart rate was measured with a Polar watch (Polar RS 400, Electro OY, Kempele, Finland). During the first two weeks, subjects were taught double-poling technique and were introduced to interval training. After this familiarization period the training intensity was progressively increased during the training period and a new training program was introduced every second week. After each training session, the meanpower output (W), distance (m) and time (min) were documented for all subjects.
Test procedure
Before and after the training period, aerobic and mechanical power was measured during sub-maximal and maximal double-poling exercises on the ergometer. The seat (backrest, foot brace and seat angle) was adjusted for each subject. The adjustments were noted, and used in all pre- and post-tests. To establish a stable pre-training level in the experimental group, test-retests were performed on two occasions (at the same time of day), one week apart in all subjects. The post-training test was conducted within one week after each subject had completed all 30 training sessions. All tests were carried out at room temperatures between 21ºC and 23ºC. The subjects were asked to keep to their normal diet and to refrain from strenuous or protracted exercise for the 24 h preceding the tests.
Prior to the test, subjects were introduced to the test procedure and the use of the Borg Rating of Perceived Exertion (RPE) 6–20 Scale (10). They were also familiarized with the SDPE and performed a 5-minute warm-up on the ergometer at 5 W. This was followed by approximately 6 min double-poling exercise at 10 W, which has been shown in a previous study to be applicable relevant work load for the SCI group (8). A 7-min break was given before the maximal test.
During the maximal test, subjects were instructed and strongly encouraged to achieve their maximum effort during the last minute of the 5-min test. The intensity was increased every min until exhaustion, starting at 10 W during the first min, followed by increased work load every minute; from 13 (somewhat hard), 15 (hard/heavy), 17 (very hard) to 20 (maximal effort), corresponding to the Borg RPE 6-20 Scale (10). If the subject felt he/she could increase even more, the test continued for another 60–120 s.
Test equipment
Oxygen consumption was obtained by using the Douglas Bag system, with 75-l bags (C. Fritze Consulting, Svedala, Sweden). This was smaller than generally used due to the low level of ventilation observed from pilot testing at sub-maximal level in the SCI group. Before the pre- and post-test sessions the Douglas Bag equipment was controlled and calibrated to fulfil accuracy criteria (11). During the tests all subjects used a mouthpiece and a nose clip. The sampling period with the Douglas Bag for the expired air was the last 120–150 s during the sub-maximal (steady state) and maximal test (11). All bags were analysed within 90 min of the completed test session.
A vasodilating cream (Linnex, Temax AB, Järfälla, Sweden) was applied on the ear tip prior to the test and blood samples (20 μl) for lactate analysis were taken immediately after the sub-maximal test and 1 min after the maximal test. The samples were immediately transferred to a tube containing haemolysing solution and were analysed with Biosen C-Line (BIOSEN 5140 analyser, EKF-Diagnostik, Magdeburg, Germany) within 12 h of test completion. Heart rate was continuously recorded during the tests with a Polar watch (Polar RS 400, Electro OY, Kempele, Finland).
Piezoelectric force sensors (Type 9311B, Kistler Instruments AG, Winterthur, Switzerland), were used to continuously register the force in the poles at a sampling frequency of 1200 Hz. The transducers were connected to an amplifier (Type 5073, Kistler Instruments AG, Winterthur, Switzerland) and signals were analog to digital converted.
Three-dimensional kinematic data were recorded using an optoelectronic system (ProReflex, Qualisys Medical AB, Gothenburg, Sweden) at a sampling frequency of 120 Hz. The camera set-up included 9 cameras that were placed in a circle with a radius of approximately 3 m around the ergometer and 4 reflective markers were attached on each pole, respectively. The SDPE display was connected to a computer and data were recorded and analysed using the Dansprint software. All signals were synchronized.
Data analysis
All oxygen uptake data were recorded in Microsoft Office Excel 2003 and used for calculating oxygen uptake (VO2 l/min and ml/kg/min), respiratory quotient (VO2/CO2) and ventilation l/min during the last min of the sub-maximal and maximal test. For heart rate, the mean value during the last min of the sub-maximal trial was used and in the maximum test the highest value recorded during 5 s was referred to as the peak heart rate. Kinematic data were digitally filtered using a 6 Hz low-pass Butterworth filter. The data were used to calculate three-dimensional angular displacement of each pole in Visual3D (C-motion Inc., Germantown, MD, USA). The power output was calculated by using the horizontal components of measured pole forces and velocities of the left pole-tip marker, and mean power per stroke and peak pole force were calculated during the last 60 s for the sub-maximal and maximal tests.
Statistics
All statistical calculations were performed in Statistica 10.0. Shapiro-Wilk’s W test was applied to control for normal data distribution. All values are presented as mean (SD). Intra-class correlation coefficients (ICC2,1) between the two pre-training test results (T1 vs T2) were calculated as indicators of the test-retest reliability. Differences in metabolic parameters and power output between pre- and post-training (T2 vs T3) were determined using a two-way analysis of variance (ANOVA) with the factors training (pre- and post-) and intensity (sub-maximal and maximum). Significant interactions were analysed with pre-determined comparisons. Pearson’s correlation coefficient was calculated between calculated power output and power output presented on the Dansprint display (data from all tests were included) and between calculated power output and oxygen uptake (data from all tests were included). The significance level for all statistical analyses was set at p ≤ 0.05.
Results
Intervention
All participants performed a total of 30 training sessions on the SDPE and all but two conducted all training sessions over the 10-week period, i.e. 3 sessions per week. Two participants had short breaks from training, due to illness, which meant that their training periods were 3–4 weeks longer.
Test–retest
Mean (SD 0.11) of the ICCs between test and re-test (T1 vs T2) was 0.81 (SD 0.11) at sub-maximal load and 0.84 at maximum load (Table II).
|
Table II. Intra-class correlation coefficient of test-retest values before training for the various tests applied
|
|
|
Sub-maximal
|
Maximal
|
|
VO2, l/min
|
0.719
|
0.944
|
|
VO2, ml/kg/min
|
0.868
|
0.928
|
|
Ventilation, l/min
|
0.893
|
0.839
|
|
RQ, VO2/CO2
|
0.639
|
0.715
|
|
Heart rate, beats/min
|
0.897
|
0.892
|
|
Lactate, mmol/l
|
0.919
|
0.664
|
|
Effect, W
|
0.744
|
0.861
|
|
RQ: respiratory quotient; VO2: oxygen uptake.
|
Training effects
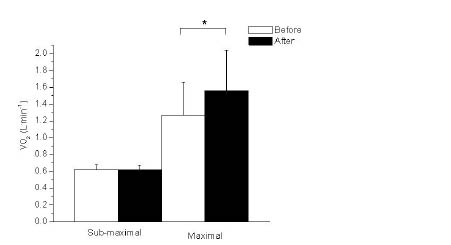
Maximal double-poling exercise. Peak oxygen uptake increased significantly from 1.27 (SD 0.39) before to 1.56 (SD 0.48) l/min after training (Fig. 1). The corresponding values for ml/kg/min were significantly increased from 18.52 (SD 4.79) before to 22.96 (SD 6.27) after the training period (Table III). There was a significant improvement in ventilation from 65.47 (SD 20.32) to 79.00 (SD 26.67) l/min (Table III). Blood lactate increased significantly from 6.71 (SD 1.81) to 8.19 (SD 2.41) mmol/l (Table III). The highest heart rates noted during the maximal test were similar before and after training, mean values being 164 (range 133–183) and 167 beats/min (136–191), respectively, and this difference was not significant (Table III). Mean power per stroke and peak pole force (mean of L and R) increased significantly from 85.62 (SD 27.88) before to 98.79 (SD 32.54) W after and from 98.44 (SD 20.74) to 121.74 (SD 29.20) N, respectively.
Sub-maximal double-poling exercise
At sub-maximal load significantly lower mean values were observed in ventilation after the training period compared with before (20.85 (SD 3.85) and 23.85 (SD 5.79) l/min, respectively) (Table III). Similarly, blood lactate levels decreased significantly from 1.41 (SD 0.84) to 1.06 (SD 0.49) mmol/l (Table III). There were no differences between pre- and post-training values in oxygen uptake (Fig. 2), power output or in peak pole force at sub-maximal load.
|
Table III. Results of sub-maximal and maximal tests before and after 10 weeks of double poling training for the 13 patients with spinal cord injury
|
|
|
Sub-maximal
|
Maximal
|
|
Before
Mean (SD)
|
After
Mean (SD)
|
Before
Mean (SD)
|
After
Mean (SD)
|
|
VO2, ml/kg/min
|
9.26 1.26)
|
9.31 (1.21)
|
18.52 (4.79)
|
22.96 (6.27)
|
|
Ventilation, l/min
|
23.85 (5.79)
|
20.80 (3.85)
|
65.47 (20.32)
|
79.00 (26.67)
|
|
RQ, VO2/CO2
|
0.95 (0.08)
|
0.88 (0.08)
|
1.27 (0.14)
|
1.30 (0.11)
|
|
Heart rate, beats/min
|
100.85 (18.31)
|
100.77 (16.45)
|
164.31 (15.20)
|
166.69 (17.34)
|
|
Lactate, mmol/l
|
1.41 (0.84)
|
1.06 (0.49)
|
6.71 (1.81)
|
8.19 (2.41)
|
|
Effect, W
|
29.34 (1.99)
|
28.94 (2.19)
|
85.62 (27.88)
|
98.79 (32.54)
|
|
Bold figures denote a significant improvement from values before to values after training.
RQ: respiratory quotient; VO2: oxygen uptake;SD: standard deviation.
|
Fig. 2. Mean values (and standard deviation) for peak oxygen uptake (VO2 l/min) during sub-maximal and maximal double-poling ergometer tests before (white bar) and after (black bar) a training period of 10 weeks. *A significant increase (p ≤ 0.05) from before to after training.
Correlations
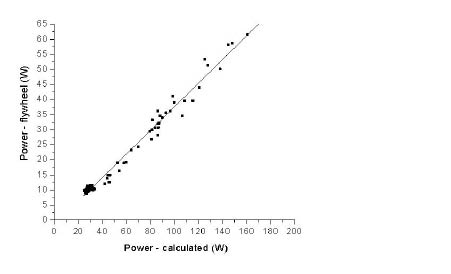
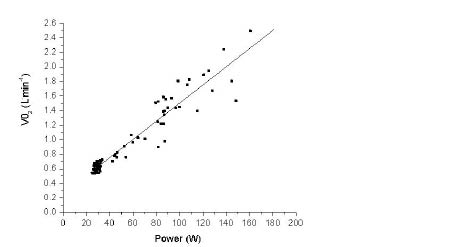
There was a positive correlation between calculated power output and power output presented on the Dansprint display (r2 = 0.982) (Fig. 3). A positive correlation was also seen between calculated power output and oxygen uptake in l/min (r2 = 0.911) (Fig. 4).
Fig. 3. Correlation between calculated power output (W) (x-axis) and power output presented on the Dansprint display (W) (y-axis). Data from all tests (before and after training) were included.
Fig. 4. Correlation between calculated power output (W) (x-axis) and peak oxygen uptake (VO2 l/min) (y-axis). Data from all tests (before and after training) were included.
Discussion
This study indicated that training on the SPDE was effective for wheelchair-dependent individuals with SCI. Maximum oxygen uptake increased by a mean of 23% following the relatively short training period of 10 weeks, and the training did not result in any upper body or shoulder overload symptoms despite the high intensity of training (12).
The training design with a warm-up, intervals and a cool-down has been used in a number of studies for individuals with SCI (13, 14, 15). Previous studies have regulated training intensity relative to load (16, 17), oxygen uptake (17), peak heart rate (6, 13, 18) or heart rate reserve (14, 19). In the present study peak heart rate was chosen. The intensity in this study was somewhat higher than previously recommended (60–80% maximum heart rate [3, 4]). 70–100% peak heart rate was used not only to optimize oxygen uptake training, but also to influence upper-body strength by implementing a protocol in which participants were required to perform short, vigorous double-poling thrusts for 15 s, which corresponded to 8–15 poling cycles. These short intervals were alternated with longer intervals of 1–3 min with the purpose of increasing aerobic capacity. Aerobic interval training with high intensity (85–95% of heart rate maximum) has been shown to be more effective in increasing peak oxygen uptake than moderate exercise of 70–80% heart rate maximum in able-bodied athletes (20) and in cardiac patients (20). Recently, a group of 6 men with SCI performed high-intensity interval training (85–95% of peak W) during combined arm cranking exercise and functional electrical stimulation leg cycling over an 8-week period and results showed that training at this intensity significantly increased peak oxygen uptake and was feasible for this group (22).
The improvements in oxygen uptake during maximal exercise by a mean of 23% were slightly higher than reported in previous studies investigating interval training on wheelchair ergometers (15–19%) (13, 15, 16). The mean increase in ventilation (21%) was similar to the improvement in oxygen uptake. Miles et al. (14) presented the only previous study reporting an increase in ventilation (32%). The participants in Miles et al. (14) were elite wheelchair basketball players and had a broad spectrum of impairments, which may have contributed to the large improvement. Other training studies including paraplegics with injury levels corresponding to the present study, reported no significant differences in ventilation (6, 13, 15). Ventilation at a steady work intensity may differ between different forms of training because breathing is often associated with the working cycle. During arm cycling or wheelchair use the frequency of the arm motion is higher than that in double-poling, in which the distance covered by the hand is greater. Furthermore, the sitting position during arm cycling is upright and trunk movement in the forward–backward direction is small. These differences between training modes may explain the differences reported in ventilation. In double-poling the upper body moves from an extended position during pole plant to a flexed position during the return phase of the pole (8). The trunk’s cyclical motion during double-poling may have assisted the accessory breathing musculature, which could have contributed to the increase in ventilation after training. Mean power per stroke during double-poling increased by a mean of 15%, which was assumed to be a result of a variety of factors, such as improved aerobic and/or anaerobic capacity, and/or increased muscle strength, i.e. on both a local and central level. The improvement may also have been a result of improvement in poling technique; none of the participants had previously trained on an SDPE.
There are few studies exploring training effects of sub-maximal intensity levels for people with SCI. In a study by Hooker et al.’s (19), participants with SCI were divided into two groups; one group trained at low intensities of 50–60% and one trained at moderate intensities of 70–80% maximal heart rate reserve. No training effect was seen in oxygen uptake, ventilation, blood lactate or heart rate in the group training at low intensity. However, significantly lower heart rate and blood lactate were reported for the group training at moderate intensity. In the present study lower values were observed in ventilation (–13%) and blood lactate (–25.0%) after the training period, which might, as mentioned above, have been a result of improvement in technique. No significant differences in oxygen uptake were, however, expected at sub-maximal intensities after the training period as oxygen uptake should be correlated with work performed (23, 24).
Calculated work correlated significantly with oxygen uptake both at sub-maximal and maximum intensity (r2 = 0.911). This may imply that maximum oxygen uptake can, under certain conditions and predetermined work-load, be calculated for people with SCI (with injury levels below T5) in a similar fashion to Åstrand’s cycling test (24). However, the number of participants was small and further studies are required to explore this possibility. Moreover, the validity of the Dansprint display was controlled by comparison with simultaneously calculated power output using data from the force transducers and motion analysis. The correlation coefficient was found to be high (r2 = 0.982), which meant that a conversion factor would permit accurate presentation of the work-load on the ergometer display.
A limiting factor in this study was the relatively low number of subjects. The number of persons with thoracic SCI in the Stockholm area is limited to approximately 130 (1, 25, 26) and, of these, approximately 75 persons are included in the database of the consumer organization. After taking into account the exclusion criteria (diagnosed cardiovascular or lung disease or other diseases potentially interfering with an intensive training programme) the population declined further. In addition, participation in the study required a considerable time commitment, including numerous test and training sessions, which might have deterred some of the potential subjects. It would have been desirable to compare the results with a matched control group not participating in the training intervention. However, this was decided against due to difficulties in recruiting such a group. Extra care was instead taken to establish a stable pre-training level by requiring all participants to perform the entire test protocol twice before the start of the training. A comparison of these two tests generally showed no differences due to any learning effect. Another limiting factor was the heterogeneity of the group. Although all individuals participating in the study were wheelchair users, had paraplegia, and had completed their rehabilitation following the injury the group was quite heterogeneous in age, sex, years since injury and level of physical activity. It was therefore difficult to draw conclusions concerning each of these factors’ contribution to the training results.
In conclusion, regular interval training on the SDPE increased oxygen uptake and power output and can be recommended for people with paraplegia below T5 level due to SCI. When developing new training equipment and training methods for people with SCI, special attention should be given to gentle and effective movement patterns, as this population is exposed to high loads on the shoulders and arms during daily activities such as wheelchair use and transitions. Despite the high-intensity training in this study, no overload symptoms were reported. On the contrary, certain types of musculoskeletal and neuropathic pain seem to benefit from training on the SDPE (12). Furthermore, training on the SDPE could also be recommended for people with other disabilities, such as impaired balance and leg muscle strength and asymmetries in upper extremity strength. These possibilities should be explored in future research.
AcknowledgementS
The authors would like to thank the Promobilia Foundation and the Swedish Centre for Sports Research (CIF) for financial support and RG Active Rehabilitation for supporting the project. Special thanks are due to the participants, who made the training and the testing period a pleasant and rewarding time for all involved.
References