OBJECTIVE: To assess the effectiveness of a multidisciplinary ambulatory rehabilitation programme for women following definitive breast cancer treatment in an Australian community cohort.
METHODS: Eighty-five women in the community randomized to a treatment group (n = 43) for individualized high-intensity programme, or a control group (n = 42) comprising usual activity. The primary outcome Depression Anxiety Stress Scale (DASS) scale measured restriction in participation. Secondary measures included Perceived Impact Problem Profile (PIPP) and Cancer Rehabilitation Evaluation System Short-Form (CARES-SF); and Functional Independence Measure (FIM) motor subscale for activity limitation. Assessments were at baseline and 4 months.
RESULTS: Intention-to-treat analysis of data showed a significant difference between both groups in DASS Depression scores (p = 0.006) (moderate effect size, r > 0.3), PIPP Mobility (p = 0.05) and Participation (p = 0.04) scales, and CARES-SF Global score (p = 0.02) (small effect size, r < 0.3). The treatment group, compared with control group, showed significant improvement in the DASS Depression scores: 22/42 (52.4%) vs 12/37 (32.4%) (p = 0.02). No difference between groups was noted in the FIM scale.
CONCLUSION: Rehabilitation can benefit participation in breast cancer survivors. Evidence for specific rehabilitation interventions is needed. Integrated cancer programmes allow opportunities to evaluate patients in various settings, but require outcome research to develop service models for survivorship issues.
Key words: breast cancer; rehabilitation; disability; participation; Functional Independence Measure; Depression Anxiety Stress Scale.
J Rehabil Med 2012; 00: 00–00
Correspondence address: Fary Khan, Department of Rehabilitation Medicine, Royal Melbourne Hospital, Poplar Road, Parkville, Melbourne VIC 3052, Australia. E-mail: fary.khan@mh.org.au
Submitted January 5, 2012; accepted April 18, 2012
Introduction
Breast cancer (BC) is a major cause of morbidity and mortality, and the most common malignancy in women worldwide. The global incidence of BC is increasing (1). In Australia, 1 in 9 women will develop BC by 2015, with the projected population of women with BC expected to increase to 15,400 (2). The BC survival rates vary between 40% and 80% in low- and high-income countries, respectively. A number of modifiable risk factors have been identified for targeted intervention (physical inactivity, obesity, alcohol use) (3). The World Health Organization (WHO) promotes BC control within national cancer control programmes integrating: prevention, early detection, diagnosis, treatment, rehabilitation and palliative care (1, 4). Rehabilitation services are considered integral to cancer control systems (1).
The rehabilitation model in cancer presents opportunities for intervention throughout the disease continuum phases (5). These may include, for example, Phase I: Staging/pre-treatment (patient education, functional preservation of range of movement, mobility aids), II: Primary treatment (effects of treatment, preserve function, lymphoedema and pain management), III: After treatment (develop, implement daily routines to restore mobility and self-care, maintenance exercise programmes), IV: Recurrence (education, adaptive equipment, exercise), V: End of life (maintain independence, equipment, education, energy conservation) (5). The various BC treatments (surgery, radiotherapy/chemotherapy) (6) and their common complications, e.g. wound sepsis, seromas and upper-limb dysfunction (pain, decreased shoulder range of movement, lymphoedema) are well-documented (7). Cognitive, psychological and mood abnormalities, sexual dysfunction and/or body dysmorphism have also been reported (8). The majority of women make good functional recovery after BC treatment; however, in some the impact of BC on activities of daily living, work, social activities and quality of life (QoL) is considerable and prolonged. Issues related to health, wellbeing and participation become increasingly important. In the community, adjustment issues may surface during transition (self-worth, self-image), coping with new demands associated with increased care needs, inability to return to driving and work, financial constraints, marital stress and restriction in participation.
A recent systematic review of multidisciplinary (MD) care for BC patients (9) identified only two randomized controlled trials (RCT) of ‘poor methodological quality’ that provided ‘weak evidence’ for inpatient MD rehabilitation in producing short-term gains at the levels of impairment (shoulder range of movement), psychosocial adjustment and QoL after BC treatment. The randomization procedures in these studies were unclear, the concealed allocation and blinding procedures were not mentioned. Although intention-to-treat (ITT) analyses were reported, there was discrepancy in the final patient numbers. A priori compliance was not specified. The aim of our study was to conduct a RCT addressing the above-mentioned methodological issues for effectiveness of MD ambulatory rehabilitation programmes in persons with BC in an Australian community cohort.
Patients and Methods
Participants and setting
This study was part of a prospective rehabilitation outcomes research programme for BC survivors at the Royal Melbourne Hospital (RMH), a tertiary referral centre in Victoria, Australia. The study was approved by its ethics committee (number 2010.203).
The 298 consecutive patients discharged to the community following acute treatment at RMH between 2007 and 2011; with the International Classification of Diseases (ICD) Code (C50) for BC (main diagnosis) incorporating all 9 sub-codes that localize the breast tumour (C50.1–C50.9) (first admission only) were identified. The RMH Access Database was used for cross-indexing of diseases from the Patient Administrator System of Hospital Information Systems, Department of Health, Victoria, Australia. The source of these patients was a pool of persons residing in the community, referred to the RMH from public and private medical clinics across greater Melbourne in Victoria. All participants were aged > 18 years and fulfilled standard diagnostic criteria for BC (10), currently disease-free and assessed by a surgeon/oncologist at the RMH. Exclusion criteria were: if current survival time was less than 4 months; and those with severe disease and unable to participate in the rehabilitation programme.
Procedure
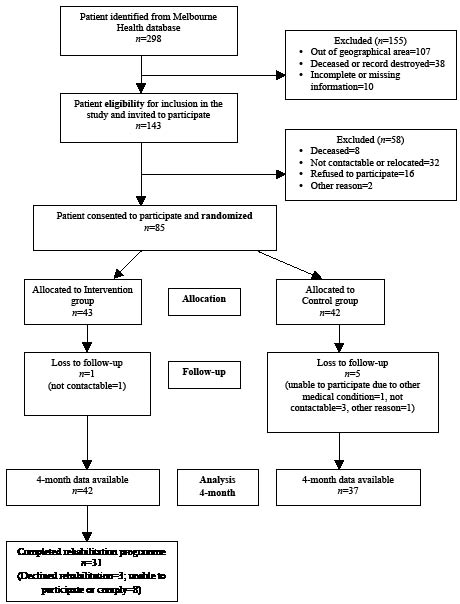
Randomization. Of the 298 women on the RMH BC Database, 143 were eligible for this study due to entry criteria (Fig. 1). All were invited by post to participate in the study, and the 85 who consented were recruited. The treatment group (n = 43) received an individualized intensive ambulatory (centre-based) rehabilitation programme, while the control group (n = 42) continued with their usual activity in the community (see details below). Computer-generated block randomization with stratification for tumour grade/severity was used; opaque sealed envelopes prevented selection bias.
Fig. 1. Recruitment process.
Assessment interviews. All baseline assessments were completed in hospital clinics (or participants’ homes) in a 6-week period, using a structured format, by 3 independent assessors. These assessors (2 physicians, 1 research officer) were trained in cognitive and functional ability assessments (examined and accredited by a National body, the Australian Rehabilitation Outcomes Dataset Centre). They were not in contact with the acute surgical/oncological services or the rehabilitation treating teams. They did not share information about participants or assessments, and received separate and different clinical record forms at each interview. They completed demographic, functional assessments and health-related QoL measures using standardized instruments (see measures). These assessment interviews took approximately 1 h. The assessors did not prompt participants, but provided assistance for those who had difficulty completing the questionnaires.
The treatment group was evaluated at recruitment and at 4 months after completion of their rehabilitation programme. The assessors did not have access to previous assessments, treatment schedules or treating rehabilitation therapy team documentation. Participants were instructed to make no comments on whatever treatment they received in the time interval between examinations and only to report any concurrent illness or hospitalization. The control group was assessed at recruitment and at 4 months follow-up. They were monitored in the community as per usual by their treating general practitioners. All assessments were secured and filed, and opened only at the time of entry into the database by an independent data entry officer.
Treatment schedules
The RMH BC programme provides acute surgical/oncological and rehabilitative care for inpatients and in ambulatory setting, 3–5 days per week for up to 8 weeks to minimize activity limitation and enhance participation. Participants in the treatment group received an individualized ambulatory rehabilitation programme (for up to 8 weeks) over the study period. An assessment of each participant’s potential to benefit from this high-intensity programme (within available resources; see below) was based on clinical features, individual need and accessibility to services, and made by a treating therapy team at the rehabilitation campus, RMH. The treating therapy teams were not aware of participant allocation in the trial. They assessed these participants along with the usual referrals from the community referred by general practitioners, health centres and other hospitals for a range of disabilities.
The intensive rehabilitation included treatment beyond symptomatic management of BC, and education to improve ‘activity’ and ‘participation’ within the limits of disease. The elements included individualized, achievable, time-based, functional goal-oriented MD treatment with active patient participation. The methods used, for example, included: physiotherapy for shoulder range of movement, strengthening, lymphoedema care; occupational therapy for energy conservation and task re-acquisition strategies to improve everyday function (domestic, community tasks), lymphoedema care, driving and return to work; and clinical psychology for counselling, coping strategies and support as required. The treatment programme included up to 3 one-hour sessions of interrupted therapy/week, involving all relevant disciplines based on participant need and team consensus. This comprised half-hour blocks of therapy sessions (social, psychology, occupational and physiotherapy), 2–3 times per week for up to 8 weeks. An a priori compliance with treatment was participant attendance in > 80% of treatment sessions.
Rehabilitation assessments for the treatment group were completed within 1 week of admission to the programme. Participant progress and goal setting were assessed in structured weekly meetings. The control group continued with their usual activity at home (local gym, yoga, community activities) and received fortnightly telephone calls to note activity levels, and to obtain information about interim medical/hospital visits. Those who needed more intensive rehabilitation were offered treatment if required. Adverse effects of rehabilitation were noted (falls, injury during treatment).
Measurement
The International Classification of Functioning, Disability and Health (ICF) (11) was used as a conceptual basis for choice of best outcomes for measurement. The effectiveness of rehabilitation in these women is expected primarily in domains of ‘participation’ and ‘activity.’ As the BC participants were generally well-functioning and in the community, the primary outcome of interest was improvement in their participation (psychosocial reintegration, mood, QoL) rather than function alone.
Breast cancer-related measures. Information included disease-related data (surgery, pathology, treatments received), signs and symptoms at admission and discharge from acute service at RMH.
Measures for participation and quality of life. The Depression Anxiety Stress Scale-21 (DASS) (12), a 3 7-item self-report scales, was used to measure the negative emotional states of depression, anxiety and stress. Participants rated the extent to which they experienced each state over the past week on a 4-point Likert rating scale. Subscale scores were derived by totalling the scores, and multiplying by 2 to ensure consistent interpretation with the longer DASS 42-item version.
The Perceived Impact of Problem Profile (PIPP) (13), a 23-item scale with 5 subscales (Mobility, Self-care, Relationships, Participation and Psychological-Wellbeing), assessed the impact associated with a health condition. For each item, respondents were asked to rate ‘how much impact has your current health problems had on (item of function or activity) using a 6-point scale (‘no impact’ and ‘extreme impact’), with high scores indicating greater impact.
The Cancer Rehabilitation Evaluation System – Short Form (CARES-SF) (14), a self-administered 59 items assessed the cancer specific rehabilitation needs and QoL. Global scores indicate QoL with summary scores for 5 domains (Physical, Psychosocial, Medical interaction, Marital and Sexual function). The participant rated the degree to which a given problem applied during the 4 weeks before the survey. Scoring was based on a 4-point Likert scale, with higher scores indicating more difficulty or impairment.
Measure for activity and functioning. Functional Independence Measure (FIM) (motor) (15), a 13 items with 4 subscales (Self-care, Transfers, Locomotion, Sphincter control) assessed function (activity) and need for assistance. Each item was rated on a scale of 1–7 (1 = total assistance, 5 = needs supervision, 7 = independent). The score reflects burden of care in each area measured. FIM has good reported reliability and validity.
Ethical approval
The study was approved by the Royal Melbourne Hospital Ethical Committee and informed consent was obtained from all subjects.
Statistical analysis
The primary outcome was defined as the impact of rehabilitation on participation in BC survivors, measured by the DASS scale. A change of 4 in DASS in participants was considered minimally clinically important difference. A sample of 36 participants in each group was needed for an 80% chance to detect a 4-point change in DASS score from baseline to 4 months in intervention vs control group (2-sided α = 0.05).
Mann-Whitney U tests compared change scores on each of the outcome measures (baseline minus post-treatment) for the treatment and control groups. Effect size statistics (r) were calculated and assessed against Cohen’s criteria (0.1 = small, 0.3 = medium, 0.5 = large effect) (16). The χ2 statistic compared the percentages of cases in the control and intervention groups who improved or deteriorated. Additional analyses were conducted comparing change scores on all measures. A p-value of < 0.05 was considered statistically significant.
A ‘complete case’ approach was used throughout the study with only those participants who provided information at both time-points included in each of the analyses. Analyses were undertaken on an ITT basis.
Results
The total sample of 85 participants were randomized to treatment (n = 43) and control groups (n = 42). Six were lost to follow-up and not contactable (5 in the control group, 1 in the treatment group). There were no significant differences in those participants lost to follow-up and those providing post-treatment results in age, years since diagnosis and median total scores on measures at baseline.
Seventy-nine (93%) participants provided scores at both time-points (42 treatment and 37 control group) (Fig. 1). Of the 42 participants randomized to the treatment group, 31 (74%) completed the rehabilitation programme (3 declined, 8 were unable to participate due to work or home duties). None in the control group required treatment during the study period.
Baseline characteristics
Participant characteristics and comparison of baseline scores in both groups for all variables are summarized in Table I. Age ranged from 33 to 80 years (median (Md) = 57 years, inter-quartile range (IQR) = 47.4–63.9), and time since diagnosis from < 1 year to 24 years (Md = 2.2 years, IQR = 1.4–4.9). The majority were tertiary educated (n = 43, 51%) and married (n = 43, 62%). Approximately half the sample in both groups had Bloom-Richardson-Elston tumour Grade 3, and the majority were oestrogen-receptor positive with lymph node involvement. More participants in the treatment group reported lymphoedema (41% vs. 16.7%) and limitation in shoulder range of motion (ROM) (48.8% vs. 16.7%). There were no significant differences between groups for demographic factors, other clinical characteristics and median total scores on measures used. However, the control group had slightly longer disease duration compared with the treatment group (median 4 years, IQR 1.8–8.9 vs. 2.3 years, IQR 1.6–3.3 years), but this was not statistically significant. Participants in both groups had high levels of functional independence. Two-thirds in both groups reported pain; shoulder dysfunction was also a concern (Table I). The mean duration of the rehabilitation programme was 21 days (range 14–21days). No adverse events were reported in either group.
| Table I. Socio-demographic characteristics of participants (n = 85) |
| | Intervention group (n = 43) | Control group (n = 42) |
| Demographic factors |
| Age, years, median (IQR) | 52.3 (47.7, 60.7) | 60.7 (47.5, 64.8) |
| Marital status, n (%) | | |
| Married/partner | 27 (62.8) | 26 (61.9) |
| Single | 5 (11.6) | 7 (16.7) |
| Living with, n (%) | | |
| Alone | 9 (20.9) | 8 (19.0) |
| Partner/family | 34 (79.1) | 34 (81.0) |
| Education, n (%) | | |
| Secondary | 14 (32.6) | 23 (54.8) |
| Tertiary | 27 (62.8) | 16 (38.1) |
| Smokers, n (%) | 5 (11.6) | 8 (19.0) |
| Consumes alcohol, n (%) | 20 (46.5) | 26 (61.9) |
| Have children, n (%) | 31 (72.1) | 34 (80.9) |
| Clinical characterisitics |
| Disease duration, years, median (IQR) | 2.3 (1.6, 3.3) | 4.0 (1.8, 8.9) |
| Bloom-Richardson-Elston grading, n (%) | 42 | 41 |
| Grade 1 (low) | 5 (11.9) | 5 (12.2) |
| Grade 2 (intermediate) | 16 (38.1) | 12 (29.3) |
| Grade 3 (high) | 21 (50.0) | 24 (58.5) |
| Oestrogen receptor positive (n = 82), n (%) | 36 (83.7) | 34 (87.2) |
| Lymph node affected, n (%) | 33 (76.7) | 23 (54.8) |
| Menopause, n (%) | 35 (81.4) | 37 (88.1) |
| Type of surgery, n (%) | | |
| Mastectomy (with or without AC) | 22 (51.1) | 18 (38.1) |
| Lumpectomy (with or without AC) | 20 (66.3) | 23 (54.8) |
| Chemotherapy, n (%) | 35 (81.4) | 28 (66.7) |
| Side-effects | 34 (97.1) | 26 (92.9) |
| Severe side-effects | 15 (42.9) | 8 (28.6) |
| Radiotherapy, n (%) | 33 (76.7) | 30 (71.4) |
| Side-effects | 25 (75.7) | 22 (73.3) |
| Severe side-effects | 3 (9.1) | 5 (16.7) |
| Reconstructive surgery or alternatives, n (%) | 12 (27.9) | 13 (31.0) |
| Co-morbidities, n (%) | | |
| Hypertension | 12 (27.9) | 15 (35.7) |
| Diabetes | 2 (4.7) | 3 (7.1) |
| Depression | 13 (30.2) | 15 (35.7) |
| Shoulder limitation in range of movement, n (%) | 21 (48.8) | 7 (16.7) |
| Shoulder limitation due to pain, n (%) | 18 (41.9) | 8 (19.0) |
| Lymphoedema, n (%) | 18 (41.9) | 7 (16.7) |
| Pain, n (%) | 33 (76.7) | 30 (71.4) |
| VAS Pain score (0 = no pain; 10 = extreme pain), median (IQR) | 3.0 (2,6) | 4.0 (2,5) |
| Phantom breast pain, n (%) | 2 (4.7) | 3 (7.1) |
| Phantom breast sensation, n (%) | 5 (11.6) | 8 (19.0) |
| Outcome measures |
| DASS, median (IQR) | | |
| Depression (0–42) | 8 (0,16) | 4 (0,11.5) |
| Anxiety (0–42) | 6 (2,10) | 2 (2,8) |
| Stress (0–42) | 10 (4,16) | 6 (4,14) |
| DASS group, n % | | |
| Depression | | |
| Normal/mild (0–13) | 34 (79.1) | 32 (76.2) |
| Moderate/severe/extreme severe (≥ 14) | 9 (20.9) | 10 (23.8) |
| Anxiety | | |
| Normal/mild (0–9) | 36 (83.7) | 33 (78.6) |
| Moderate/severe/extreme severe (≥ 10) | 7 (16.3) | 9 (21.4) |
| Stress | | |
| Normal/mild (0–18) | 38 (88.4) | 37 (88.1) |
| Moderate/severe/extreme severe (≥ 19) | 5 (11.6) | 5 (11.9) |
| PIPP, median (IQR) | | |
| Psychological (1–6) | 2.2 (1.4, 2.4) | 2.0 (1.2, 3.1) |
| Self Care (1–6) | 1.0 (1, 1) | 1.0 (1, 1) |
| Mobility (1–6) | 1.4 (1, 1.8) | 1.0 (1, 1.4) |
| Participation (1–6) | 2.0 (1, 3.4) | 1.2 (1, 2.3) |
| Relationship (1–6) | 1.3 (1, 2.3) | 1.0 (1, 1.6) |
| CARES-SF Global, median (IQR) | | |
| Physical (0–4) | 0.5 (0.3, 1.3) | 0.4 (0.2, 0.9) |
| Psychological (0–4) | 0.4 (0.3, 1) | 0.4 (0.2, 1.1) |
| Marital (0–4) | 0 (0, 0.5) | 0 (0, 0.04) |
| Sexual (0–4) | 1 (0, 2) | 1 (0, 2.7) |
| Misceallenous (0–4) | 0.3 (0.1, 0.6) | 0.3 (0, 0.7) |
| Overall (0–4) | 0.5 (0.4, 1) | 0.5 (0.2, 1) |
| FIM, median (IQR) | | |
| Self care (6–42) | 36 (36, 36) | 36 (36, 36) |
| Sphincter control (2–14) | 12 (12, 12) | 12 (12, 12) |
| Mobility (3–21) | 18 (18, 18) | 18 (18, 18) |
| Locomotion (2–14) | 12 (12, 12) | 12 (12, 12) |
| Total (13–91) | 78 (78, 78) | 78 (78, 78) |
| AC: axillary clearance, CARES-SF: Cancer Rehabilitation and Evaluation System Short-Form, DASS: Depression Anxiety Stress Scale, FIM: Functional Independent Measure; IQR: interquartile range, Md: median, MRC: Medical Research Council scale; PIPP: Perceived Impact of Problem Profile, SD: standard deviation, VAS: visual analogue scale. |
Outcome measurements change scores
Mann-Whitney U tests revealed a significant difference between treatment and control groups in DASS Depression scores (p = 0.006) with moderate effect size (ES) (r > 0.3), but no significant difference in the DASS Anxiety (p = 0.55) and Stress (p = 0.23) subscales. Significant differences were also detected for PIPP Mobility (p = 0.05) and Participation (p = 0.04) scales, and the CARES-SF Global score (p = 0.02), but the ES were small (r < 0.3 for all). No difference between groups was noted in the FIM motor subscale (Table II).
| Table II. Summary of per protocol analysis of outcomes of breast cancer rehabilitation programme |
| Scale | Intervention (n = 42) | Control (n = 37) | Mann-Whitney U test |
| Median | IQR | Median | IQR | z | p-value | Effect size |
| DASS | | | | | | | |
| Depression | 2 | 0 to 12 | 0 | –6 to 4 | –2.76 | 0.006* | 0.31 |
| Anxiety | 2 | –2 to 4 | 0 | 0 to 2 | –0.61 | 0.545 | 0.07 |
| Stress | 0 | –4.5 to 4 | 0 | –7 to 2 | –1.21 | 0.228 | 0.14 |
| PIPP | | | | | | | |
| Psychological | 0.2 | –0.2 to 0.8 | 0 | –0.2 to 0.4 | –0.98 | 0.330 | 0.11 |
| Self-care | 0 | 0 to 0 | 0 | 0 to 0 | –0.19 | 0.854 | 0.02 |
| Mobility | 0 | 0 to 0.4 | 0 | –0.4 to 0 | –1.97 | 0.049* | 0.22 |
| Participation | 0.1 | 0 to 0.8 | 0 | –0.3 to 0.2 | –2.11 | 0.035* | 0.24 |
| Relationship | 0 | –0.5 to 0.3 | 0 | –0.3 to 0 | –0.43 | 0.667 | 0.05 |
| CARES-SF (global scores) | | | | | | | |
| Physical | 0.05 | –0.3 to 0.4 | 0 | –0.2 to 0.2 | –0.39 | 0.693 | 0.04 |
| Psychological | 0 | –0.4 to 0.2 | 0.1 | –0.2 to 0.2 | –0.86 | 0.390 | 0.10 |
| Medical | 0 | 0 to 0.1 | 0 | 0 to 0.3 | –0.44 | 0.657 | 0.05 |
| Marital | 0 | –0.2 to 0.04 | 0 | 0 to 0 | –0.13 | 0.896 | 0.01 |
| Sexual | 0 | –1 to 0.4 | 0 | 0 to 0.3 | –1.06 | 0.291 | 0.12 |
| Overall | –0.3 | –0.5 to 0 | –0.1 | –0.3 to 0.2 | –2.33 | 0.020* | 0.26 |
| FIM | | | | | | | |
| Self-care | –6 | –6 to 0 | –6 | –6 to –1 | –0.37 | 0.712 | 0.04 |
| Sphincter | –2 | –2 to –2 | –2 | –2 to –2 | 0 | 1.000 | 0.00 |
| Locomotion | –2 | –2 to 0 | –1 | –2 to 0 | –1.09 | 0.277 | 0.12 |
| Mobility | –3 | –3 to 0 | –3 | –3 to 0 | –0.26 | 0.797 | 0.03 |
| Total | –11.5 | –13 to –2 | –12 | –13 to –3.5 | –0.39 | 0.700 | 0.04 |
| *p < 0.05. CARES-SF: Cancer Rehabilitation and Evaluation System Short-Form, DASS: Depression Anxiety Stress Scale, FIM: Functional Independent Measure; PIPP: Perceived Impact of Problem Profile; SD: standard deviation, Md: median, IQR: interquartile range. |
Over the study period significantly more participants in the treatment group showed a decrease in their DASS Depression scores (22/42: 52.4%), compared with the control group (12/37: 32.4%, p = 0.02).
Discussion
To our knowledge this is the first report of effectiveness of an ambulatory MD rehabilitation programme in BC population in an Australian community cohort. The treatment group showed improved participation in depression (DASS), Mobility and Participation (PIPP) scales, and CARES-SF Global score, compared with the control group at 4 months. There was no change in ‘activity’ using the FIM motor subscales, probably due to the high functioning BC participants in the community (ceiling effect) (see below). These results provide some support for rehabilitation for psychosocial adjustment and QoL after BC treatment, consistent with other reports (17, 18). The participants in this study are similar to those in other studies for age, socio-demographic features, disease severity and treatment (18, 19). The rehabilitation programme provided standard treatment and management in accordance with existing BC care guidelines (20).
Our preliminary analysis (21) showed that despite good functional recovery following definitive treatment for BC, participants reported residual neurological deficits (motor/sensory) with weakness of the upper limb on the affected side, limited shoulder movement (adhesive capsulitis), pain limiting shoulder range; and lymphoedema, consistent with other reports (22, 23). Although the medium- to long-term effects of BC treatment are usually considered minimal, the associated long-term physical and psychological morbidity has been under-estimated (22). Three-quarters of participants in the present study reported some degree of breast-specific pain (musculoskeletal, neurogenic, mixed patterns), similar to other reports (6); shoulder dysfunction and lymphoedema were also reported. A comprehensive report of pain, shoulder dysfunction and lymphoedema, however, was beyond the scope of this study. With significant progress in BC care and improved survival rates, survivorship issues (pain, fatigue, nausea, low mood, psychosocial needs, the physical effects of treatment and consequences, and gynaecological/reproductive concerns) have been identified, which may negatively influence QoL (24). The reported risk factors for depression include: cancer treatment characteristics, physical and psychosocial functioning, and health behaviours (24, 25). The younger women with anxiety and distress need more social supports (26). Although there are reports of women adapting over time (27), younger age is a risk factor for depression and anxiety up to 5 years after diagnosis. Depression can influence cancer progression, lower QoL (28) and prevent attainment of previous levels of functioning (29). Recently, BC survivors (median time since diagnosis 2 years), reported elevated levels of anxiety and depression (22%) (higher compared with normative Australian data) (21), in contrast to a previous study of psychological distress that showed a decrease in psychological morbidity over a 5-year study period (26). This has important implications for long-term monitoring, education, health promotion, support and counselling of the BC patients (and their families) (22, 23, 28). Multidisciplinary care including rehabilitation can provide an integrated approach for many survivorship issues, and provide appropriate services, support groups and specialized programmes.
The optimum functional outcome assessment tools in BC care are yet to be identified, and vary in different studies. Instruments measuring ‘activity’, e.g. the FIM, have successfully measured functional gains in inpatient rehabilitation; however due to its ceiling effect at a higher level of function (as in this study), the FIM is less useful in ambulatory settings and in long-term survivors with residual deficits due to their disease or its treatment (6). Other tools, such as CARES-SF, and PIPP (14), provide participatory information, show clinical change with treatment, but low statistical significance (ES). The measurement of QoL is difficult, as many factors influence it. The ICF (11) provides a framework for describing the impact of disease at the level of limitation in ‘activity and participation’. One study assessed functional limitation in women after BC using the ICF domains (30), and linked patient reported problems with categories of existing ICF BC Core Set (31) to highlight the patient perspective; so that a ‘core set’ of selected disabilities can be validated in different MD care settings. Similar to other core sets (32), these in the future may enable more comprehensive measurement of participatory issues in BC population using item banking and scale development techniques (33).
There were many challenges in conducting this RCT in a rehabilitation setting, similar to other reports (34, 35). The BC participants presented with a range of survivorship issues and required individualized approach. Methodological issues included: blinding, attrition (especially control group), heterogeneous patient characteristics, multilayered treatments, interdependent components, individual interventions and ethical considerations. Standardizing therapy was difficult in the ambulatory setting, therefore ‘manualization’ of treatments was used (i.e. a described intervention provided by therapist X, e.g. a 30 min treatment session included a stretching and muscle strengthening protocol) (36). However, determining the effective dose, intensity, components and combination of treatment modalities in rehabilitation in the study population was not possible, and further research is needed.
This study was conducted in the ‘real world’ setting of a tertiary public hospital with finite resources. It was difficult to recruit participants as most were well, working, studying and living in the community. The MD treatment goals were individualized for each participant, based on need and survivorship issues (such as fatigue management, coping, adjustment, self-image and self-worth, driving, work). Many treating medical/surgical staff struggled with need for referral to rehabilitation service given lack of no ‘acute’ issues. This required education of various treating teams and integration of existing services that operated in ‘silos’, with fragmented service delivery. The control group were informed of the wait time for rehabilitation services as per usual practice, and were not unduly disadvantaged. Operationally, it was beyond the resources of our hospital to provide therapy for this many patients simultaneously. Rehabilitation is an expensive intervention. The implications of this study include triaging and prioritizing the BC survivor who needs targeted rehabilitation input. Emphasis should be on a longer-term monitoring of maintenance of function and psychological sequelae in the community.
The randomization was stratified based on disease severity. The intervention group had more severe grade of BC, however these differences were not statistically significant and the study results support effectiveness of the programme and clinical significance. Comparison and generalizability of these results is difficult, larger sample sizes in different settings are needed to confirm these findings. Selection bias cannot be ruled out as participants were listed on a single RMH database who agreed to participate. However, all eligible participants on the database were contacted, irrespective of their demographic or disease status. The patient attrition rate was consistent with other studies in similar settings (34, 35). There was no statistical difference in any of the study variables between participants who completed post-treatment assessment and those lost to follow-up. We acknowledge that other factors may have impacted depression and QoL in BC participants and were not studied. More research into ongoing pain, shoulder dysfunction and lymphoedema outcomes is needed.
To reduce potential bias the treating therapists and assessors were blinded. The assessors were independent of the rehabilitation or acute hospital teams. Whilst a comprehensive approach to outcome measurement was undertaken, other important outcomes such as impact on carers and families may have been missed. Analysis of costs associated with care was beyond the scope of this study. The impact of other rehabilitation modalities and interventions is unknown.
This study provides some evidence to support rehabilitation for improved participation in BC survivors in the community. More research in the effectiveness of ‘specific’ rehabilitation interventions is needed. Cancer rehabilitation services can benefit BC patients throughout disease continuum at acute or subacute levels. This, however, requires integrated cancer care that includes rehabilitation services to allow opportunities for evaluating patients in various settings (6). More emphasis on physician/patient education and outcome-orientated research is needed to explore service models and strategies to implement individualized treatment and integrated MD care programmes to address BC survivorship issues.
Acknowledgement
We are grateful to all participants with breast cancer in this study. We particularly wish to thank Ms L. Oscari and Drs N. Zhang, M. Demetrious, L. Ng and G. Abbott for patient assessments; T. Khan for data entry and A. Gorelik for power statistics. We also acknowledge Professor B. Mann and Dr A. Skandarajah of Cancer Services at the Royal Melbourne Hospital.
Conflict of interest statement. The authors declare no conflicts of interest.
References