OBJECTIVES: Given the burden associated with vehicle-related trauma, there is interest in time and cost effective methods of providing information to assist recovery. This systematic review aims to address the question: “Do targeted early information interventions improve outcomes following vehicle-related injuries for persons of working age?”
Data Sources: Ovid Medline, EMBASE, PsychINFO and Cochrane databases were searched for studies published between 1990–April 2011.
Data Selection: Included studies were randomized or pseudo-randomized controlled trials of information interventions delivered to working age persons following vehicle-related injuries. Two reviewers independently selected and appraised the studies.
Data Synthesis: Sixteen publications (13 primary studies) met the inclusion criteria and were assessed for bias. Heterogeneity in terms of the information interventions and measured outcomes was encountered. In 4 of the included studies, the intervention was positively associated with at least one outcome reported. Methodological issues limited the conclusions that could be drawn.
CONCLUSION: Following vehicle-related trauma, people often experience difficulties in ongoing functioning. The current evidence neither supports nor fails to support the effectiveness of information interventions in promoting injury recovery. There is a need for larger more methodologically and conceptually rigorous randomized controlled trials that better consider the type and timing of the intervention.
Key words: information; interventions; controlled trials; outcomes; traumatic injuries; systematic review.
J Rehabil Med 2012; 44: 521–533
Correspondence address: Dr Fiona Clay, Institute for Safety Compensation and Recovery Research, Monash University, 499 St Kilda Road, Melbourne, Victoria, 3004, Australia. E-mail: Fiona.Clay@monash.edu
Submitted December 22, 2011; accepted March 23, 2012
INTRODUCTION
Vehicle-related traumatic injuries are a major public health problem. A leading cause of both morbidity and mortality, motor vehicle-related injuries cause a range of physical, cognitive and psychological disabilities that may seriously impact on the quality of life of affected individuals and their families (1–4). Depending on the nature and severity of the injuries, the socioeconomic burden following vehicle-related trauma may be associated with increased health service utilization, the need for carers, extended loss of workforce participation and medical, rehabilitation and wage replacement compensation payments.
The World Health Organization estimates that 20–50 million people are injured in motor vehicle crashes annually (5). In Australia in 2007, an estimated 50,000 new transport accident compensation claims were submitted (6). Vehicle-related trauma is conservatively estimated to annually cost the Australian community approximately $A18 billion (7). Vehicle-related trauma accounts for more than half of all severe traumatic brain injury and spinal cord injury. The lifetime costs of new cases of brain and spinal cord injury that occurred in Australia in 2008 is estimated at 10.5 billion (8).
In many jurisdictions internationally, persons injured as a result of motor vehicle accidents have an entitlement to personal injury compensation. While the level of personal injury compensation entitlements varies between jurisdictions; one of the aims of injury compensation is to promote recovery and independence. As such, there is interest in identifying potentially time and cost effective methods of providing information to assist injury recovery including the experience of the compensation claims process.
Under the International Classification of Functioning, Disability and Health, vehicle-related trauma can impact both body functions and structures but also result in limitations in activities and participation. Rehabilitation can be slow and the provision of information offers opportunities to aid recovery and return to activities as well as social and economic participation.
Research suggests that interaction with the compensation system can be a source of frustration and stress for those who are injured and may impact outcomes (9–11). Injured persons report a lack of information, and poor communication when interacting with compensation systems (11–13). In one study of the experiences of pursuing a personal injury claim, 40% of the injured participants reported dissatisfaction with the provision of information on legal proceedings (14). Conversely, compensation and health insurance systems have a unique opportunity to positively impact an injured persons recovery not only through the provision of effective and efficient treatment and rehabilitation services but also by providing information to facilitate the recovery of injured persons.
While previous systematic reviews have noted the potentially adverse effects of debriefing psycho-education following traumatic injury (15, 16) and the variable effectiveness of information provision for the self-management of neck pain and concussion (17, 18), the effectiveness of information provision following vehicle-related trauma is not well understood. A better understanding is critical to determining appropriate resource allocation in this area of health care. The specific aim of the systematic review was to address the question “do targeted early information interventions improve outcomes following vehicle-related traumatic injury for persons of working age?”
METHODS
Search strategy
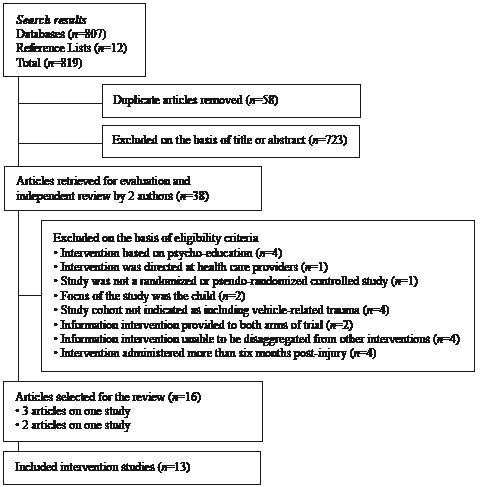
We searched the Ovid Medline, PsychINFO, Cochrane Central Register of Controlled trials (2nd quarter, 2011), Cochrane Database of systematic reviews and EMBASE databases for studies published from 1990 to April 2011 on vehicle-related traumatic injuries and information-education providing interventions. The search strategy is outlined in Fig. 1. Search terms were mapped to MESH terms or subject headings and synonyms were grouped together using Boolean operators. Therapy filters (sensitive) were applied where available. Guidelines of the Cochrane Collaboration together with assistance from a subject librarian were used to develop a search strategy that would identify relevant studies. A detailed description of the search strategy applied to the Medline and PsychINFO databases is provided in Appendix SI (available from http://www.medicaljournals.se/jrm/content/?doi=10.2340/16501977-0980). The reference lists of all relevant articles were screened for additional publications.
Fig. 1. Flow diagram for retrieval of included studies for this systematic review.
Results of the database searches were downloaded into Endnote X3 and duplicate papers excluded. One reviewer (FJC) initially screened all titles and abstracts for potentially relevant title and or abstract. Full text articles considered to be relevant together with articles where there was uncertainty as to relevance were screened by two authors (FJC, RJM) and a decision made as to which articles should remain. Disagreements were resolved by consensus.
Inclusion and exclusion criteria
The review was limited to peer-reviewed studies published in English and available as full text. Only randomized controlled or pseudo randomized controlled trials (RCT) were considered. Articles were selected for inclusion according to the following definition of an information-education intervention. An education or information based intervention was defined as any group based or individual intervention which predominantly provides only education or information about injury recovery including future difficulties, constructive ways of coping, getting back to normal activities. Other inclusion criteria were:
• Sample in the analysis of outcomes only included persons of working age (defined as 15–64 years of age) at the time of the injury.
• Studies that included a range of injury mechanisms were included only if the vehicle-related trauma comprised at least 30% of the recruited cohort.
• The recipient of the intervention was the injured person.
• Interventions were delivered in the early stages post-injury (operationalized as within 6 months of the date of injury).
The following studies were excluded:
• Studies where it was not possible to disaggregate the information-education intervention from other interventions given as part of a multilevel clinical care approach.
• Studies of psycho-education where the majority of the intervention comprised counselling techniques, e.g. treatment of post-traumatic stress disorder (PTSD) that includes a review of traumatic experience, encouragement of emotional expression and cognitive processing of experience. These studies have formed the basis of recent systematic reviews (15, 16).
• Primary injury prevention studies.
• Studies where the recipient of the intervention was a health care provider.
• Studies of neck or back school as these have been the subject of recent reviews.
Risk of bias assessment
A risk of bias assessment was carried out for each included study according to 7 criteria (Table I). The criteria which address the 6 major sources of bias in intervention studies were based on the Cochrane Collaboration’s tool for assessing risk of bias (19). The assessment addressed potential bias in the form of selection (random sequence generation, allocation of concealment), performance (blinding of participants and personnel), attrition (incomplete outcome data), detection (blinding of outcome assessment), reporting (selective reporting) and other bias. Other bias was defined as contamination by study group or co-interventions and analysis not intention to treat or significant variation from study design. No overall total quality score was determined as this is somewhat subjective and may not be informative as it ascribes equal weight to each of the nominated criteria. No studies were excluded on the basis of quality; however, the findings on the risk of bias were taken into account when drawing conclusions about the interventions. Two authors (FJC, RJM) independently assessed the risk of bias of each study. Disagreements were resolved by discussion.
| Table I. Criteria for assessing risk of bias of studies of information and education based interventions for injury recovery following vehicle related trauma |
| Type of bias | Impact of bias |
| Selection | Random sequence generation |
| | Allocation of concealment |
| Performance | Blinding of participants and personnel |
| Detection | Blinding of outcome assessment |
| Attrition | Incomplete outcome data |
| Reporting | Selective reporting on study design or of results |
| Other | Contamination between groups or due to co-interventions Analysis was not intention to treat Lack of compliance with intervention |
All included studies were also rated by one author (FJC) according to the CONSORT 2010 checklist. (www.consort-statement.org/consort-statement/) (20). The CONSORT Statement is intended to improve the reporting of a RCT and a better understanding of the trial’s design, conduct, analysis and interpretation, and to assess the validity of its results. The checklist comprises 25 items, 12 of which have two parts making a total of 37 items. Each item or sub-item identified as being reported in the study publication scored one point (maximum of 37 points). Where checklist items were considered as not applicable to a study, for the purpose of the review, the study was rated as having met those criteria.
Data extraction
Data was extracted from each study into preformatted tables. The data collection methods were pilot tested on two articles that did not form part of the review. After full review, the following data was extracted as they appeared in the original publication: study population and setting, baseline sample size, nature of injuries, mode of injuries, inclusion and exclusion criteria, study design, main outcomes, interventions delivered, follow-up time-points, compliance with the intervention, side effects of the intervention, extent of attrition, type of analysis, main results and overall findings. The following information was collected for all interventions: medium of information, form of intervention reinforcement, intervention provider, delivery timeframe, intervention duration. Due to the number of outcomes assessed, effect sizes are reported for significant results only. Statistical significance was set at p < 0.05.
RESULTS
Selection of studies
The search strategy identified 807 references from the 5 databases. Twelve potentially relevant references were identified from the reference lists of articles. After removal of duplicates, 761 references remained. Of these, 723 references were excluded based on either the title or abstract. Reasons for exclusion are provided in Appendix SII (available from http://www.medicaljournals.se/jrm/content/?doi=10.2340/16501977-0980). The full text of 38 articles were retrieved and examined in detail by 2 authors (FJC, RJM), 22 did not meet the inclusion criteria (see Appendix SIII (available from http://www.medicaljournals.se/jrm/content/?doi=10.2340/16501977-0980)). Reasons for exclusion included that the information was a co-intervention for all groups or could not be disaggregated from other aspects of clinical care, that the interventions was primarily focused on psycho-education, the study did not report the mechanisms of injury for the recruited cohort, the unit of analysis in the study was a child, or that the intervention was administered later than 6 months post-injury. After independent review by 2 authors, 16 publications focusing on 13 primary studies were included in the review. The search strategy is outlined in Fig. 1.
Risk of bias assessment
The two reviewers were in concordance 85% of the time after the first assessment. Consensus was achieved following discussion. The risk of bias assessment revealed methodological problems with many of the studies. A number of studies only reported that the participants were randomized but provided no details on how that was achieved. While randomization is supposed to ensure an even spread of known confounders, for some studies the intervention and comparisons group differed for important characteristics at baseline suggesting that randomization had not been ideal.
In two studies, selective reporting was such that the numbers in each trial arm were not reported. For the majority of studies, it was not possible to accurately establish the degree of blinding of participants and personnel or whether outcome assessment was blinded. The possibility of type 1 error was acknowledged in two studies, one of which reported on 66 outcome measures (21, 22). Two of the studies were pseudo randomized involving alternate allocation to trial arms raising the high probability that allocation of patients was not concealed (22, 23). Table II presents the risk of bias assessment for each of the included studies.
| Table II. Risk of bias for intervention studies included in the review. If more than one paper was written on the study, the risk of bias assessment is based on all the papers |
| Reference | Random sequence generation Selection bias | Allocation of concealment Selection bias | Blinding of participants and personnel Performance bias | Blinding of outcome assessment Detection bias | Incomplete outcome data Attrition bias | Selective reporting Reporting bias | Other biasa Performance- Measurement bias |
| Rosenfeld (31, 34, 40) | U | L | H | L | L | L | L |
| Paniak (27, 41) | L | U | U | L | L | L | L |
| Ferrari (28) | L | U | H | L | L | L | L |
| Kongsted (32) | L | U | H | H | H | L | L |
| Oliviera (22) | H | H | U | U | L | H | H |
| Ehlers (33) | L | U | U | U | L | L | L |
| Brison (29) | L | U | U | L | L | L | L |
| Turpin (26) | L | L | U | L | H | L | H |
| Scholes (30) | L | L | U | U | H | L | L |
| Mittenberg (24) | U | U | U | U | U | L | H |
| Alves (25) | U | U | U | U | U | U | U |
| Ponsford (23) | H | H | H | H | H | H | H |
| Scholten-Peeters (21) | L | L | H | L | L | L | L |
| aContamination between groups OR due to co-interventions, analysis not intention to treat, lack of compliance with intervention or study protocol. H: high risk; L: low risk; U: unclear risk. |
Agreement with the Consort statement
Included studies were examined for the number of items reported according to the Consort 2010 checklist of items to be reported on in RCT’s (20). If there was uncertainty with respect to the reporting of items, the item under questions was scored as being reported. None of the included studies reported all items on the checklist, all consistently did not report the clinical trial registration number or where the full study protocol could be accessed. Two studies reported on only 12 items (24, 25) and another two on 18 items (22, 23). It is clear that the reporting of randomised controlled trials on information interventions needs to be improved if there is a potential to apply the findings from such studies. The consort checklist score for each study is presented in Table III.
| Table III. Characteristics of the included studies |
| Reference | Country setting | Nature of injuries | Inclusion criteria | Exclusion criteria | Intervention(s) | Main outcomes | Follow-up time points (weeks) | Consort items reported n |
| Rosenfeld (31, 34, 40) | Sweden Primary care units Emergency wards Private clinics Traffic related: 100% | Acute neck strain as a result of rapid movements of the head | Exposure to whiplash trauma in automobile crashes Referred to the study within 96 hrs of the collision | Cervical fracture or dislocations, neurologic deficit, head injury, previously symptomatic chronic neck problems, alcohol abuse, dementia, serious mental disease, or diseases that could be expected to result in death before the study was completed | Active involvement INTERVENTION: active exercise protocol involving information, postural control and cervical rotation exercises and treatment by McKenzie principles if symptoms do not resolve Exercises to be performed 10 times every h as soon as symptoms allowed Information intervention: Written information on injury mechanisms, advice on suitable activities to be done a few times every day beginning at 2 weeks post injury and postural correction | Head, neck, shoulder pain, days of sick leave, change in pain intensity, range of movement, costs | 26, 156 | 25/37 |
| Paniak (27, 41) | Canada ED-hospital attendees Traffic related: 42.9% | Mild traumatic brain injury | Adults diagnosed according to the American Congress of Rehabilitations 1993 MTBI definition | History of inpatient treatment for any psychiatric disorder, diagnosis of mental retardation, insufficient English skills, history of TBI more severe than current injury, MTBI with 1 year of current study, central nervous system disorder, pregnant | INTERVENTION: Single session preventative education treatment for PCS in hospital emergency room with outpatient preventative treatment rehabilitation. Given the National Head Injury Foundations Minor Head Injury brochure and had one session with a psychologist Comparison group: Treatment as needed | Post concussive symptoms, satisfaction, community integration, head injuries cognitive, behavioural, physical problems All domains of problem checklist and SF-36 were considered as outcomes | 13, 52 | 21/37 |
| Ferrari (28) | Canada ED-hospital traffic related : 100% | Whiplash injury WAD grades 1–2 | Seated within the interior of a car, truck or van in a collision and had < 5 mins loss of consciousness and presented within 72 h of their collision ≥ = 18 years | Grade 3–4 WAD No fixed address, unable to communicate in English | INTERVENTION: one page educational pamphlet based on the Whiplash Book Comparison group: Usual care | Response to the question: “How well do you feel you are recovering from your injuries?” with responses ranging from “all better” to “much worse” Symptom severity, need to modify leisure activities, limitation of daily activities, resource use, work status, litigation | 2, 13 | 25/37 |
| Kongsted (32) | Denmark ED-attendees GP’s- attendees Traffic related: 100% | Whiplash injury Less substantial complaints | 18–70 years Exposed to a rear-end or frontal car collision Experienced WAD symptoms within 72 h of collision and seen within 10 days Danish speaker | Fractures or dislocations of the cervical spine, amnesia or unconsciousness in relation to the accident, injuries other than whiplash, significant somatic or psychiatric disease, known alcohol or drug abuse, high self reported neck pain in 6 months prior to the injury | Intervention 1: Personal patient education of 60 min from nurse at a home visit. Education aimed to reduce fear and uncertainty and encourage resumption of normal activities Intervention 2: patient education using an 8 page pamphlet that focused on reassurance and continuation of normal activities | Return to work, sick leave neck pain, headache, disability, being recovered | 13, 26, 52 | 29/37 |
| Table III. Contd. |
| Reference | Country setting | Nature of injuries | Inclusion criteria | Exclusion criteria | Intervention(s) | Main outcomes | Follow-up time points (weeks) | Consort items reported n |
| Oliviera (22) | USA ED attendees and urgent care facilities Most common cause of injury rear ended traffic collision (proportions not provided) | Acute cervical strain | Diagnosed acute cervical strain | Current fracture or dislocation, previous cervical spinal pathology, head trauma with loss of consciousness, history of cardiovascular disease, hospitalization for presenting complaints | INTERVENTION: 12 min cervical strain psycho-educational video at patients bedside plus neck strain aftercare instruction sheet plus a knowledge quiz Comparison group: Usual care Pseudo-randomized with alternate allocation to group | 66 outcome measures listed Workdays missed, life change due to injury, patient satisfaction, severity of pain, polypharmacy, legal involvement, health service utilization, musculoskeletal functioning | 4, 13, 26 | 18/37 |
| Ehlers (33) | United Kingdom ED-hospital Traffic related: 100% | Injured patients at increased risk of PTSD | 18–65 years Meeting diagnostic criteria for PTSD with moderate to severe symptoms | LOC for ≥ = 15 min post injury, having no memory of the accident, history of psychosis, current alcohol or substance dependence, borderline personality disorder, severe depression needing immediate treatment in its own right, insufficient English skills | Intervention 1: CBT: 12 weekly sessions Intervention 2: Self-help booklet-64 pages “Understanding your reactions to trauma” plus one session with a clinician Intervention 3: repeated but in frequent assessments of PTSD symptoms | Severity of PTSD symptoms, anxiety, depression, disability | 13, 39 | 31/37 |
| Brison (29) | USA ED-hospital Traffic related: 100% | Whiplash injury WAD 0–5 Rear-end MVC | ≥ = 16 years, involved in a simple rear-end motor vehicle collision, spoke English | Refused to be contacted for research purposes, were making a return visit to the ED for assessment, were an occupant in a vehicle from which another occupant had already been enrolled, could not be contacted within 7 days of MVC | INTERVENTION: 20 min educational video sent to patients home which outlined best available evidence regarding WAD management Comparison group: Usual care | Presence of persistent WAD symptoms Change in pain levels | 24 | 35/37 |
| Turpin (26) | United Kingdom ED-hospital attendees Traffic related:41.6% | Physical injury | 16–65 years, injuries sustained as a result of a road traffic accident, occupational injury or assault | Non-English speaking | INTERVENTION: 8 page, 550 word self help information booklet “Response to traumatic injury” describing and normalising reactions to traumatic injury sent 6–8 weeks after the injury Comparison group: Usual care received a letter about the study but not the booklet | PTSD, anxiety, depression | 2, 12, 26 | 25/37 |
| Scholes (30) | United Kingdom ED-hospital attendees Traffic related: 100% | Persons with acute stress disorder identified as at high risk of PTSD | 16–65 years, injuries sustained as a result of a road traffic accident, assault or occupational injury | Non-English speaking | INTERVENTION: Self help booklet on the sequelae of trauma and advice on cognitive behavioural strategies Comparison group: Usual care | PTSD, anxiety, depression, quality of life, compliance, usefulness | 4, 13, 26 | 27/37 |
| | | | | | | | | |
| Table III. Contd. |
| Reference | Country setting | Nature of injuries | Inclusion criteria | Exclusion criteria | Intervention(s) | Main outcomes | Follow-up time points (weeks) | Consort items reported n |
| Mittenberg (24) | USA Hospital Traffic related: 58% | Mild head injury | GCS 13–15 on admission | Patients with medically significant extracranial injuries, post traumatic amnesia exceeding 24 h, GCS below 13 at the time of admission to the ED | INTERVENTION: Patients received a 10 page printed manual “Recovering from mild head injury: a guide for patients” that addressed normal responses to stress, anxiety or depressive self statements and reattribution of symptoms to selective attention. Prior to discharge, patient met with a therapist to review the manual and check understanding Comparison group: Usual care | Post-concussive symptoms | 26 | 12/37 |
| Alves (25) | USA Hospital Traffic related: 56.6% | Uncomplicated mild head injury | GCS 13–15 with no evidence of skulls fracture, haemorrhage or contusion | Patients with extracranial trauma requiring hospitalization > 48 h | Information only: general information provided at discharge by a nurse about expected symptoms and prognosis Information and reassurance provided at discharge by a nurse. Information on expected symptoms and prognosis and reassurance that recovery should be uncomplicated and complete plus weekly phone calls Comparison group: Usual care | Post concussive symptoms | 13, 26, 52 | 12/37 |
| Ponsford (23) | Australia ED-attendees Traffic related: 34% | Mild head injury | ≥ = 16 years, English speaking, history of trauma resulting in loss of consciousness for less than 30 min, PTA < 24 h, GCS 13–15: ED arrival | Required surgery involving general anaesthesia or had focal neurological signs | Intervention group: Information booklet outlining common symptoms associated with mild head injury, likely time course and suggested coping strategies Comparison group: Usual care Pseudo-randomized with alternate assignment to group | Psychological adjustment, post concussion symptoms, concurrent life stresses | 1, 13 One week intervention group only | 18/37 |
| Scholten-Peeters (21) | The Netherlands ED-attendees and General practices Traffic related : 100% | Whiplash injury, acute WAD grade 1–2 | 18–55 years Acute WAD grade 1–2 as a result of a road traffic accident with symptoms of pain, headache and dizziness in the first 48 hrs. | Cervical hernia, past cervical spondylodesis, LOC, history of previous neck or head injury, co-morbidities, non Dutch speaker. not resident in the Netherlands | Intervention 1: Education and advice including advice on graded activity given by GP’s Intervention 2: Education, advice, graded activity, and exercise therapy given by physiotherapists Co-interventions: allied health care, psychological counselling | Neck pain, headache intensity, work activities in daily living Functional recovery, general health status, cervical range of motion, fear of movement, coping, disability in home and social activities | 8, 12, 26, 52 | 33/37 |
| MTBI: mild traumatic brain injury; WAD: whiplash-associated disorders; TBI: traumatic brain injuty; PCS: Physical component summary score; SF-36: Short Form-36; ED: emergency department; MVC: Motor Vehicle Collision; LOC: loss of consiousness; PTA: Post Traumatic Amnesia; PTSD: post-traumatic stress disorder. |
Assessment of statistical analysis
In the majority of studies, insufficient detail was provided in order to be able to make an appropriate assessment of the statistical quality or to fully understand the results. Some studies provided probability values but did not report the means or standard deviations (22, 23). In other studies, the analytic technique was outlined with insufficient detail for someone independent of the study’s authors to derive the same result. Features of the statistical analysis including the number of persons randomized, extent of attrition, main analytic technique and the significant results as reported in the papers are reported in Table IV.
| Table IV. Results from the included studies |
| Reference | Baseline | Attrition/ missing data Compliance | Analysis | Main results (significant findings only) Side effects Cost of care Co interventions | Overall conclusion on information intervention |
| Rosenfeld (31, 34, 40) | Active < 96 h n = 21 > 2 weeks n = 22 Standard < 96 h n = 23 > 2 weeks n = 22 | 9%: 6 months 25%: 3 years Compliance: Not reported | ANOVA χ2 t-tests | Both interventions associated with a reduction in pain intensity of 6 months and 3 years Active intervention associated with significantly greater pain reduction than standard treatment (p < 0.001) and in number of days of sick leave at 3 year follow-up No significant differences between groups for cervical range of motion Time of intervention administration did not influence outcome Active intervention given early and Standard treatment administered at 14 days had a greater impact on pain level Cost of intervention: Active involvement and intervention was less costly and more effective than standard treatment Co-intervention analysis: No statistically significant differences between groups | Intervention not effective |
| Paniak (27, 41) | Intervention n = 59 Treatment as needed n = 60 | 18% Compliance: Not reported | MANOVA ANOVA | No significant differences in outcomes between groups including patient satisfaction with services received. Both groups showed improvements and improvements at 3 months remained at the 12 months follow-up Cost of intervention: Not reported but authors argued that the brief intervention would be cost effective | Intervention not effective |
| Ferrari (28) | Intervention n = 55 Control n = 57 | 9% Compliance: 79.6–85.5% | t-tests χ2 | No significant differences in outcomes for pain intensity, functioning, limitations in daily activities, therapy use, medications used, days off work or global perceived effect Co-intervention analysis: no between group differences | Intervention not effective |
| Kongsted (32) | Oral advice n = 119 Pamphlet n = 63 | 50%: 3 months 13%: 12 months Compliance: Not reported | Regression Non-parametric tests Medians | No significant differences between groups on all outcomes Non significant trend to improved outcomes for group receiving oral advice | Intervention not effective |
| Oliviera (22) | 126 Numbers in each trial arm not reported | 13.4% Compliance reported as very high but frequency not stated | ANCOVA t-tests χ2 | Analyses conducted on 66 outcomes measures Video group relative to comparison group associated with significant (p < 0.05) improvements in numbers of health provider visits, polypharmacy utilization, requests for imaging (xrays, cat scans), use of neck brace, initial bed rest, lower pain levels, work days missed, patient satisfaction, life change as a result of injury Means and SD not reported for continuous measures | Intervention partially effective |
| Ehlers (33) | Cognitive therapy n = 28 Self help booklet n = 28 Repeated assessments n = 29 | 9.2% Compliance: Not reported | MANCOVA | Cognitive therapy associated with better outcomes (PTSD and associated symptoms and disability symptoms) than the self help booklet at post treatment and follow-up (p < 0.05) No difference between groups in credibility of intervention No difference between repeated assessment and self help booklet at post treatment and follow-up | Intervention not effective |
| Brison (29) | Intervention n = 206 Comparison n = 199 | 14%: 24 weeks 18%: 52 weeks Compliance (71.6–76%) | t-tests χ2 Non-parametric tests | Persistent symptoms decreased over time for both groups Intervention associated with an improvement in median pain score relative to control at 24 weeks (p = 0.016) Persistent pain symptoms (Trend toward reduced symptoms for video group) Co-intervention analysis of impact: Yes, significant difference in chiropractic use between groups | Intervention partially effective |
| Turpin (26) | Intervention n = 146 Comparison n = 145 | 70% Compliance: Not reported | MANOVA ANOVA | No significant differences in PTSD, depression or anxiety caseness between groups at either 3 or 6 mths follow-up Side effects: Control group less depressed and less PTSD case-ness than the intervention group at follow-up | Intervention not effective |
| Table IV. Contd. |
| Reference | Baseline | Attrition/ missing data Compliance | Analysis | Main results (significant findings only) Side effects Cost of care Co interventions | Overall conclusion on information intervention |
| Scholes (30) | High risk intervention n = 116 High risk control n = 111 Low risk control n = 120 | 52.2% Compliance: Not reported | MANOVA ANOVA | No significant differences in outcomes between groups at follow-up All groups showed improvements in symptoms | Intervention not effective |
| Mittenberg (24) | Intervention n = 29 Comparison n = 29 | Not reported Compliance: Not reported | t-tests χ2 | Information intervention associated with significantly reduced frequency (number of PCS symptoms) mean 3.10 (SD 3.19) to 1.62 (SD 2.04)) intensity (scale 1–10) mean 1.72 (SD 1.93) to 0.80 (SD 1.13)) duration of symptoms (days) (mean 51.19 (SD 45.10) to 33.18 (SD 35.62)) fewer symptomatic days (0.5 vs 3.1) | Intervention partially effective |
| Alves (25) | Usual care n = 210 Information only n = 176 Information and reassurance n = 201 | Not reported Compliance: Not reported | χ2 Descriptive | No significant differences between groups at follow-up, decrease in post concussive symptoms over time | Intervention not effective |
| Ponsford (23) | Intervention n = 136 Comparison n = 126 Numbers reported differently in two places in publication | 38% (intervention group) Comparison group (not reported) Compliance: Not reported | ANCOVA | No difference between groups in neuropsychological measures Improvements in sleep and levels of anxiety for intervention group (p < 0.05) Comparison group higher scores on symptom checklist global severity especially paranoia, hostility subscales (p < 0.05) No means or SD reported | Intervention partially effective |
| Scholten-Peeters (21) | GP care n = 42 Physio care n = 38 | 3.7% Compliance: Not reported | Mann-Whitney Cox and linear regression | No significant differences between groups for primary outcomes measures of neck pain intensity, headache intensity and work activities Cervical range of motion at 12 weeks post-injury favoured physiotherapy group (adjusted mean difference 12.3 degrees CI 2.7–12.9) Functional recovery at 1 year post injury favoured GP group (adjusted relative risk 2.3, 95% CI 1.0–5.0) | Intervention not effective |
| ANOVA: analysis of variance; MANOVA: multivariate analysis of variance; PTSD: post-traumatic stress disorder; SD: standard deviation; CI: confidence interval; GP: General Practitioner. |
Summary features of the included studies
Details of the information-education interventions pertaining to vehicle-related trauma or cohorts that included vehicle-related trauma are summarised in Table III. Data pooling was not appropriate given the range of different outcomes, timing and mode of intervention administration and periods of follow-up.
The included studies were from 7 countries with the majority conducted in an acute care or community setting. The most common cohort was whiplash trauma followed by traumatic brain injuries, mild head injuries and acute stress disorders. For one study, the injuries were not well specified being referred to only as physical injury (26). While the search strategy identified a number of information interventions in spinal injury cohorts, these studies were excluded because either the intervention was not delivered in the first six months post-injury or the study did not document the mechanism of injuries for the recruited cohort. All of the included studies focused on mild to moderate injuries. While all the cohorts included persons who had sustained vehicle-related trauma, 6 of the studies also included participants injured due to mechanisms other than motor vehicles (22–27).
The intervention was compared to usual care in 8 studies (22, 24–30). Only 3 studies reported on co-interventions (28–29, 31). The review was unable to identify any relevant studies that focused on persons from non-English speaking backgrounds.
More than 75 different measures of outcome were assessed across the 13 studies reviewed. One study was not well focused and evaluated 66 outcome measures (22). Two studies acknowledged the possibility of type 1 errors because of the number of outcomes analysed (21, 22). The range of outcomes measured reflected aspects of symptom frequency-severity, mental and physical health, quality of life, and health service utilization. Satisfaction with the intervention and increased knowledge following the intervention were also measured. The impact of the intervention on employment status was assessed in 5 studies (21, 22, 28, 31, 32).
Of the 13 included studies, 4 reported a positive impact of the intervention on at least 1 of the outcomes (22–24, 29), 8 reported that the intervention did not have a statistically significant effect, while 1 study reported a potentially negative impact of the intervention (26).
While all the studies reported on interventions delivered during the first 6 months post injury; the time period of intervention administration varied from the first 24 h post-injury to approximately 3 months post-injury (Table V). The time period of participant follow-up was relatively short, falling between 2 and 26 weeks post baseline in 7 studies and extending to 12 months or longer for the remaining studies. The most common provider of the intervention was a nurse (22, 25, 28, 32) followed by a physiotherapist (21, 31). In one study, the provider was not specified (23). There was no discernible association between the provider of the intervention and improved outcomes. No reinforcement of the intervention was provided for any intervention although indirect follow-up would have occurred when study participants were contacted to complete follow-up surveys or attended medical appointments. Only two of the studies involving a written material intervention measured compliance with the intervention (28, 29) and both reported high compliance rates. The length of written material that formed the basis of interventions varied widely, ranging between 1 and 64 pages.
| Table V. Components of the information – education intervention included in each study |
| Reference | Medium | Provider of intervention | Reinforcement of the intervention | Time post-injury of intervention administration | Duration of intervention |
| Rosenfeld (31, 34, 40) | Written | Physiotherapist | None | 96 h or 14 days | Self determined 1? |
| Paniak (27, 41) | Oral-written | Psychologist | None | 3 weeks | Self determined 1? |
| Ferrari (28) | Written | Nurse | None | 3 days | Self determined 1? |
| Kongsted (32) | Oral-written | Nurse | None | 10 days | 60 min |
| Oliviera (22) | Audiovisual | Nurse | None | 12 h (50%) | 12 min |
| Ehlers (33) | Written-oral | Clinician | None | ~ 3months | 40 min |
| Brison (29) | Audiovisual | N/A | None | 24 h | 20 min |
| Turpin (26) | Written | N/A | None | 6–8 weeks | Self determined 1? |
| Scholes (30) | Written | N/A | None | 1 month | Self determined 1? |
| Mittenberg (24) | Oral-written | Therapist | None | Not specified | 60 min |
| Alves (25) | Oral | Nurse | None | Discharge | 60–75 min |
| Ponsford (23) | Written | Not reported | None | 5–7 days | Not specified |
| Scholten-Peeters (21) | Oral | General practitioners or Physiotherapists | None | 4 weeks | GP’s: 10 min Physiotherapists: 30 min |
| N/A: not applicable; GP: General Practitioner. |
Methodological quality and risk of bias
A risk of bias assessment was carried out according to recommendations of the Cochrane collaboration (19). The assessment rates each study for the risk of bias in terms of selection, performance, detection, attrition and reporting.
The methodological quality of the reviewed studies varied substantially. The majority of studies had small sample sizes, for 4 studies the sample size at baseline in the intervention arm(s) was less than 50 persons (21, 24, 31, 33). One study did not report the number of persons in each intervention arm (22) and in another study the publication reported two sets of different numbers for the intervention arms (23). Study dropout leading to incomplete outcome data was a significant problem in around half of the studies; some of these studies had small sample sizes at baseline. For two studies attrition was greater than 50% of those recruited at baseline (26, 30). For 5 studies, it is not possible to make a conclusion about the effectiveness of the intervention as the study lacked a usual care control group (21, 27, 31–33). Compliance with the interventions was infrequently documented. The validity of many studies was affected by a low recruitment rate and an increased likelihood of a type 1 error. Finally, the reporting on a number of studies was sufficiently poor to make it difficult to assess the risk of bias due the lack of information reported (22–25).
Consequently, the results of the studies must be interpreted with caution and these methodological limitations must be considered when interpreting the following summary of the review results.
Further, very limited information on the personal injury compensation system, nature of injuries and the type of vehicle-related trauma was available for the majority of included studies. Only one study provided any description of the personal injury compensation system under which the recruited cohort operated (29). A further study while not describing the compensation system reported the proportion of participants engaged in litigation for compensation (24).
A range of information and education based interventions formed the basis of the studies. The mode of intervention delivery included, video or DVD, paper based pamphlets books and manuals and in person education. Some of the included studies examined more than one mode of information provision. Findings from these categories of intervention will now be discussed.
Paper-based interventions
A total of 9 studies examining the impact of paper-based interventions were reviewed. These interventions ranged in size from a 1 page pamphlet to a 64 page manual. Three of the studies focused on participants with head injury/mild traumatic brain injury, 3 were aimed at alleviating symptoms of PTSD and 3 studies focused on WAD. Overall, 3 of the studies reported at least 1 positive impact of the intervention, 1 reported a potentially adverse impact, and the reminder reported no impact.
Of the 3 studies focused on PTSD, 2 reported the intervention resulted in potentially adverse outcomes -increase in levels of depression at 6 months post injury or greater number of requests for treatment at follow-up. The third reported no effect of the intervention.
Face-to-face or ‘in-person’ interventions
Six studies examined the impact of ‘in person’ education or information. These interventions ranged from single sessions to multiple sessions conducted over different time-periods. In 3 of the studies, written information was also provided. For these studies, there was general improvement for all persons regardless of the trial arm to which they were randomized; one study demonstrated a positive impact of the intervention on post concussive symptoms following mild head injury.
Video or DVD intervention
One RCT identified a positive impact of 20 min educational video sent to the patient’s home in a group of patients with whiplash-associated disorders. The intervention was associated with improved self-rating of pain frequency, severity and location (29). A second RCT observed a positive impact of a 12 min educational video viewed at the bedside (in hospital) in patients with acute cervical strain. The intervention was associated with reduced pain ratings, less time away from work, less narcotic use and less health service utilization (22).
DISCUSSION
Sixteen articles reporting on 13 primary studies were included in our synthesis of information and education interventions for injury recovery following vehicle-related trauma.
Our synthesis identified a range of interventions including self-help written material, information delivered by DVD or video, and in person education. The majority of included studies addressed cohorts with whiplash trauma, traumatic brain injury, and acute stress disorder. The most common type of information intervention was based on self-help written material. In only 4 of the studies, the intervention was associated with a positive improvement in at least 1 of the outcomes measured.
Methodological limitations, or failure to report important aspects of the study design limit the usefulness of many studies that formed part of the review, and subsequently our ability to generalise conclusions on the basis of the literature reviewed. These included the heterogeneity of interventions, outcome measures, endpoints and injury populations studied as well as failure to adequately define source target and study populations (diagnostic criteria were seldom reported), failure to monitor or report on compliance with the intervention or any co-intervention, low retention rates and in some studies the lack of an appropriate control arm (e.g., usual care). Although all the studies were randomized or pseudo-RCT, most recruited small groups of participants, limiting the ability of the trial to estimate the relative effectiveness of an intervention. Large RCT are the most appropriate design for testing the safety and effectiveness of interventions.
The vast majority of studies did not report details of the personal injury compensation or health insurance system for the jurisdiction(s) in which the study took place. As such it is difficult to draw generalizable conclusions about interventions for promoting recovery from vehicle-related trauma, and very difficult to interpret the results of the review in terms of their applicability to the motor accident compensation environment.
The majority of studies included in the review focused on paper-based interventions. Results were highly variable among this group of studies with no discernible patterns emerging. For example, one interpretation of the paper-based intervention studies is that provision of ‘generic’ material is an ineffective early-intervention tool but that information tailored to the injured person, or delivered at the hospital beside, may be more effective. Other interpretations of these studies are also possible and hence the need for more detailed consideration before embarking on similar studies in the future.
Relevance to compensation settings
The studies included in this review arose from 7 countries. Ten of the studies were from English-speaking countries, 3 were from the UK, 4 from the USA, 2 from Canada and 1 from Australia. The personal injury compensation and healthcare arrangements in these countries vary greatly. Furthermore, the social and demographic differences between these jurisdictions limit the extent to which the outcomes of the studies reviewed can be directly translated to other contexts. We also note that none of the studies reviewed examined interventions focusing on providing information on the compensation system, claims and/or legal processes. This is a gap in the current research literature and an area worthy of further investigation.
The included studies in this review considered more than 75 outcomes and used different measures and questionnaires to measure outcomes. None of the studies in the review assessed information needs by way of validated information provision questionnaires. A potential explanation for the lack of effects may be that the duration and timing of the intervention were not appropriate or provided any means or reinforcement to be effective. This is supported by the findings of a meta-analysis of psychosocial interventions that established that the most effective interventions were those that lasted 12 weeks or more (35).
While the evidence synthesis from this review neither supports nor fails to support the effectiveness of information interventions in facilitating injury recovery, it should not be concluded that the provision of information-education is unnecessary. Insufficient information is a key issue highlighted in a number of studies of exploring claimant’s interactions with the personal injury compensation claims and legal process (9, 13, 14). For the studies included in the review that measured perceptions of the usefulness of the information or satisfaction with the information provided, all reported that the injured cohort found the information useful. That the information was not associated with measurable improvements in injury recovery may relate to the injured cohort randomized to the trial arms being so mildly injured that all patients improved irrespective of the provision of information. The two studies that delivered information using audio-visual techniques were associated with improvements in some of the outcomes assessed. The timing of the intervention was in the first 24 hours post-injury and the duration of the intervention was brief being between 12 and 20 min.
Strengths and limitations
The strengths of this review are that the methodology closely followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analysis) statement for the preferred reporting for systematic reviews of intervention studies (36). Other strengths are that we limited our inclusion criteria to studies in which the information component was standalone or could be disaggregated from other components of a multimodal intervention approach and excluded studies of psycho-education that primarily used counselling rather than education modalities. This enabled the review to more directly focus on the effects of information provision. The extent of heterogeneity was such that we were unable to pool the results to. While every effort was made to include all relevant articles; it is possible that articles were missed due to the terms employed in the search strategy although the likelihood of having missing key studies in the area is considered to be small. Limiting studies to those of working age and excluding studies where the information intervention was administered after the first 6 months post injury or could not be disaggregated from other aspects of clinical care may result in the loss of relevant findings. One example is spinal cord injured cohorts who may be too acutely injured to benefit from an information intervention delivered in the first six months.
Comparison with other reviews
Reviews of patient education following neck pain reported unequivocal results (17) or a trend to improved outcomes when education forms part of a multimodal strategy (37). One review of information needs following poly-trauma concluded that the timing and type of information and mode of delivery was critical to the effectiveness of the information provision. While acknowledging that the amount and type of information required can be complicated by the patient’s constellation of traumatic injuries, it recommended the need for information to be tailored to 3 post-injury phases subacute, acute and outpatient rehabilitation if care providers are to effectively support families in their care-giving roles (38).
Information provision has been the subject of research in the context of cancer survivors. One systematic review of information provision following cancer identified that patients with fulfilled information needs reported better health related quality of life and less anxiety and depression (39). Patient-centred information needs vary by gender, age, cultural background, education level and coping style. The review suggests that it is not the quantity but the quality of information that is important for adequate information provision. Given that the experience of health is a bio-psychosocial phenomena as well as the commonality of the overall findings in this review, there is potential to apply these findings to an injury setting.
Implications for research, policy and practice
Given the heterogeneity of the studies included in this review, there is a lack of evidence to support or fail to support the use of information interventions in practice. More rigorous studies that consider the type, timing, mode of delivery, content, quantity and quality of information provision are needed before it can be unequivocally determined if the provision of information has the potential to impact on injury recovery and be time and cost effective. Furthermore, the review identified a lack of published information in some areas. These include interventions based in culturally and linguistically diverse populations, interventions aimed at caregivers, interventions focusing on providing information on the compensation system claims and legal process, cost effectiveness studies, studies reporting the impact of cultural factors and health literacy factors on compliance with interventions and large-scale RCT. Finally, studies that direct the information intervention at health care providers rather than patients or caregivers would also be informative.
CONCLUSION
The studies included in this review highlight the challenges associated with recovery and return to functioning following vehicle-related trauma. While, overall the current evidence neither supports nor fails to support the effectiveness of information interventions in promoting injury recovery, there remains a need for further more methodologically rigorous specifically focused research in this area.
Acknowledgements
The authors wish to thank Beth Kilgour for advice on psycho-education and Janneke Berecki-Gisolf for useful discussions.
Conflict of Interest statement: All authors receive funding through a grant from WorkSafe Victoria and the Transport Accident Commission. The authors declare that there are no conflicts of interest.
Funding Source: This manuscript has been prepared from a project commissioned and funded by the Motor Accident Authority of New South Wales. The study sponsors had no involvement in the study design; collection, analysis and interpretation of data; the writing of the manuscript; and the decision to submit the manuscript for publication.
REFERENCES