OBJECTIVE: To investigate the association between rehabilitation timing and the occurrence of post-total knee arthroplasty complications and related medical service utilization.
METHODS: Data from Taiwan’s National Health Insurance Research Database from 2003–2006 were used to perform a retrospective study on patients who received their initial total knee arthroplasty during 2004–2005 (a total of 21,143 subjects). All subjects were divided into 1 of 3 groups based on the timing of their rehabilitation after total knee arthroplasty, namely, the within 2 weeks group, the after 2 weeks group or the no-rehabilitation group.
RESULTS: We found that patients in the no-rehabilitation group and the after 2 weeks group had higher incidences of prosthetic infection (odds ratio (OR) = 1.29, p = 0.0409; OR = 1.66, p = 0.0012) and deep venous thrombosis (OR = 1.51, p = 0.0099; OR = 2.07; p = 0.0007) than in the within-2-weeks group. In addition, compared with the within-2-weeks group, the after 2 weeks group had higher total medical expenses (exponentiated regression coefficient: Exp. (β) = 1.07, p = 0.0211), and the no-rehabilitation group had lower total medical expenses (Exp. (β) = 0.01, p < 0.0001).
CONCLUSION: The results of this study indicated that, because the incidence rates of complications and medical service utilization among total knee arthroplasty patients in the within 2 weeks group were lower than in the after 2 weeks group, the timing of rehabilitation may be 1 factor affecting post-total knee arthroplasty complications and promoting high levels of medical service utilization. These findings could be useful for clinicians and health policymakers attempting to improve total knee arthroplasty services.
Key words: total knee arthroplasty; timing of rehabilitation; medical service utilization.
J Rehabil Med 2012; 00: 00–00
Correspondence address: Ching-Wen Chien, Institute of Hospital and Health Care Administration, National Yang-Ming University, 112 Taipei, Taiwan. E-mail: ihhca@yahoo.com.tw
Submitted February 10, 2011; accepted January 17, 2012
INTRODUCTION
The number of patients who are disabled due to arthritis is increasing as the global geriatric population rises rapidly. Similar to many other developed countries, such as the USA, Taiwan has over 2 million arthritis patients, and nearly 100,000 of these are disabled due to degenerative arthritis (1). Late-stage arthritis usually involves severely damaged joints that can significantly limit knee function, often leading physicians and patients to opt for total knee arthroplasty (TKA) (2).
TKA typically alleviates 85–95% of patients’ pain, thus improving their quality of life (QoL) (3). However, there are some post-TKA complications, including prosthetic infection (PI), deep venous thrombosis (DVT), improper wound healing, wound infection, bone fracture and joint loosening, which may negatively impact TKA patients’ QoL. PI and DVT are the worst complications. For example, Chesney et al. (4) followed 1509 cases for up to 5 years and found that there was a 3.3% chance of superficial infection and a 1% chance of deep infection. SooHoo et al. (5) retrospectively studied 222,684 patients in Los Angeles who received TKA between 1991 and 2001 and found that there was a 0.71% chance of acquiring an infection within 90 days after surgery and a 0.41% of a pulmonary embolism caused by DVT, and that the incidence rate was higher in females than in males. Quinlan et al. (6) examined 3,500 patients and found that the odds of post-TKA DVT was 1.8% . The occurrence of DVT is related to the time a patient spends lying down. In the worst-case scenario, DVT may result in necrosis or even amputation of a limb. Previous studies have indicated that failing to prevent the occurrence of DVT after TKA increases readmission, morbidity and mortality (7–9). In addition, PI is also a serious problem, because, once it occurs, a patient requires antibiotics, the infected knee must be cleaned, function might be lost, and sometimes the prosthesis needs to be removed; the mortality rate ranges from 2.7 to 18% (10, 11). Treatment of PI often requires removal of the infected prosthesis and prolonged intravenous antimicrobial therapy. The cost of each episode is estimated to be > 50,000 USD (12). In addition to the cost of the process, it can affect a patient’s health and, subsequently, their QoL.
The extent of rehabilitation can affect the outcome of TKA, as documented by previous studies (13, 14). From a health policy perspective, the rehabilitation of TKA patients has important managerial implications: in an attempt to limit health expenditures, Taiwan’s Bureau of National Health Insurance (BNHI) has paid for TKA procedures under Diagnosis Related Group (DRG) since November of 1997, but also offers clinical pathways (CP) to ensure the quality of TKA (15). However, because the BNHI does require rehabilitation to follow TKA, some TKA patients never receive rehabilitation or receive rehabilitation long after TKA. It is clear that rehabilitation is complementary to TKA, but previous studies have not found a relationship between the timing of rehabilitation and TKA outcomes (16). This study examined the association of different rehabilitation timings with adverse outcomes (PI and DVT), medical service utilization in terms of outpatient, inpatient expenses related to PI and DVT, and rehabilitation expenses for TKA patients.
METHODS
Data sources
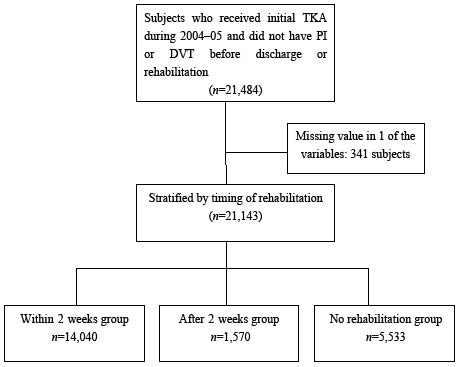
This study analysed Taiwan’s 2003–2006 National Health Insurance Research Database (NHIRD) released by the National Health Research Institutes (NHRI) for public research purposes. A retrospective design was used in this study. The NHIRD is an administrative database containing all medical care claims for outpatient, inpatient and emergency room services of all NHI patients, which is 99% of Taiwan’s 23 million people. It is one of the largest and most complete nationwide population-based data-sets in the world. Important information included in this database are diagnostic codes from the International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM), detailed medical expenditures, treatments, prescriptions, hospital size, and each enrolee’s age and gender. The NHIRD consists of de-identified secondary data that can be released for research purposes; the applications for data-sets are reviewed by the NHRI and data are released in cases meeting NHRI ethical and scientific criteria. The subjects of this study were those who were discharged from their initial TKA without related complications, based on BNHI standards, during 2004–2005. Patients who developed PI or DVT before discharge or rehabilitation were excluded from this study to reduce possibility of over-or under-estimation of the incidence and total medical expenses. A total of 341 subjects were removed from this study due to missing values for one of the studied variables. The study population consisted of 21,143 subjects. Every post-TKA complication was verified by matching diagnostic and procedural codes (ICD-9-CM) with prescriptions and treatments used in this study (Fig. 1).
Fig. 1. Selection and assignment of subjects. TKA: total knee arthroplasty; PI: prosthetic infectio; DVT: deep venous thrombosis.
Variables
The independent variable in this study was the timing of rehabilitation. In Taiwan, TKA rehabilitation is still not a mandatory medical treatment. TKA postoperative rehabilitation is based on a protocol found in handbooks of orthopaedic rehabilitation (17). In the protocol, TKA patients initiate isometric exercise, such as ankle pumping, and begin continuous passive motion (CPM) on the first day after surgery. From the second day to the second week, patients begin passive range of motion (ROM) exercises, such as knee extension, knee flexion and heel slides within a ROM of 0–90 degrees. From the tenth day to the third week, patients practice walking with a walker. In the sixth week, patients begin weight-bearing and stationary cycling. Patients were divided into 1 of 3 groups receiving inpatient or outpatient rehabilitation services: those who received rehabilitation within 2 weeks after discharge (within 2 weeks group), those who received rehabilitation more than 2 weeks after discharge (after 2 weeks group) or no rehabilitation at all after discharge (no rehabilitation group). The main reason for using a 2-week post-surgery cut-off point is because wound healing after surgery occurs in approximately 7–14 days. In Taiwan, the mean hospital stay after TKA is between 7 and 14 days. The usual site of adhesion after TKA is the suprapatellar pouch. According to Brotzman’s Handbook of orthopaedic rehabilitation (17), if manipulation of the adhesion is to be carried out, it is better to perform it early. An early manipulation (e.g. approximately 2 weeks) can be carried out with minimal force. After this time period, adhesions become stronger and can cause contracture of the knee. For this reason, we selected a cut-off point of 2 weeks after discharge as the appropriate time to start rehabilitation.
Dependent variables of the study included post-TKA-associated complications and total medical expenses within 1 year after discharge. Post-TKA-associated complications were measured by the occurrence of PI and DVT within 1 year after discharge. PI and DVT were defined as TKA patients who had an ICD-9-CM code (PI: 996.66; DVT: 453, 453.2, 453.3 and 453.8) in outpatient, emergency and inpatient medical services within one year after discharge and were treated with antibiotics (ATC code: J01CA12, J01CF01, J01CF02, J01CA04, J04CA05, J01DA11, J01DA24, J01EA01, J01EC01, J01XA01, J01XA02, J01DD02, J01DE01 and A07AA09) during the indexing of medical records. Total medical expenses were measured by rehabilitation expenses, outpatient and inpatient expenses related to PI and DVT within 1 year after discharge. Confounding variables included patients’ gender, age, exemption status for cost sharing, and Charlson Comorbidity Scores (CCS) (18). Exemption from cost sharing was defined as the medical expenses that were not paid by the patient. The CCS was first developed by Charlson et al. (18). Subsequently, Deyo et al.(19) used the ICD-9-CM code to define the original CCS categories.
Statistical analysis
This study used SAS 9.1.3 (SAS Institute, Cary, NC, USA) for statistical analyses. χ2 and analysis of variance (ANOVA) analyses were used to compare associations and differences in post-TKA-associated complications and medical expenses among different rehabilitation groups. A multiple regression analysis, including adjustment for the confounding variables, was used to assess the influence of the different rehabilitation schedules on total medical expenses, including outpatient and inpatient expenses related to PI and DVT and rehabilitation expenses. Because those expenses did not fit a normal distribution, a logarithmic function was used to transform them before regression analysis. A logistic regression analysis was used to assess the odds ratio of post-TKA-associated PI and DVT events for the different rehabilitation schedules.
RESULTS
As shown in Table I, subjects in the 3 groups were significantly different in age, CCS and total medical expenses. These 3 factors were significantly associated with gender, exemption from cost sharing, PI and DVT. When we compared total medical expenses of the 3 rehabilitation groups, we found that the no rehabilitation group had the lowest total medical expenses (4,603.42 New Taiwan Dollars (NTD)(1 USD = 32.51 NTD as of June 30, 2005)) and that the after-2-weeks group had the highest total medical expenses (6,913.98 NTD). The percentages of patients who developed a PI or DVT also differed among the 3 groups; the within 2 weeks group and no rehabilitation groups had the lowest rates of PI (1.7%), and the within 2 weeks group had the lowest rate of DVT (0.8%).
| Table 1. Descriptive statistics |
| Variable | All subjects | Timing of rehabilitation | p-value |
| Within 2 weeks | After 2 weeks | No rehabilitation |
| Total, n (%) | 21,143 | 14,040 (66.4) | 1,570 (7.4) | 5,533 (26.2) | |
| Gender, n (%) | | | | | < 0.0001 |
| Female | 15,898 (75.2) | 10,689 (76.1) | 1,173 (74.7) | 4,036 (72.9) | |
| Male | 5,245 (24.8) | 3,351 (23.9) | 397 (25.3) | 1,497 (27.1) | |
| Exemption from cost sharing, n (%) | | | | < 0.0001 |
| No | 18,718 (88.5) | 12,615 (89.9) | 1,316 (83.8) | 4,787 (86.5) | |
| Yes | 2,425 (11.5) | 1,425 (10.1) | 254 (16.2) | 746 (13.5) | |
| Age, mean (SD) | 69.68 (8.0) | 69.56 (7.9) | 69.30 (8.5) | 70.08 (8.1) | < 0.0001 |
| CCS | 2.06 (1.86) | 2.08 (1.86) | 2.21 (1.91) | 1.97 (1.85) | < 0.0001 |
| Total medical expenses, NTD, mean (SD)a | 3,607.37 (8,750.33) | 4,603.42 (9,551.60) | 6,913.98 (10,661.53) | 141.66 (3,350.08) | < 0.0001 |
| PI, n (%) | | | | | < 0.0001 |
| No | 20,760 (98.2) | 13,808 (98.3) | 1,515 (96.5) | 5,437 (98.3) | |
| Yes | 383 (1.8) | 232 (1.7) | 55 (3.5) | 96 (1.7) | |
| DVT, n (%) | | | | | < 0.0001 |
| No | 20,936 (99.0) | 13,926 (99.2) | 1,541 (98.1) | 5,469 (98.8) | |
| Yes | 207 (1.0) | 114 (0.8) | 29 (1.9) | 64 (1.2) | |
| a1 New Taiwan Dollars (NTD) = 0.031 US dollars (the average exchange rate from 2004–2006). CCS: Charlson Comorbidity Scores; SD: standard deviation; PI: prosthetic infection; DVT: deep venous thrombosis.. |
Table II shows the results of a multiple regression analysis after the statistical influence was adjusted for confounding variables (including patients’ gender, age, exemption status for cost sharing and CCS). Because the medical expenses were transformed by natural log, the exponential regression coefficients are presented as the percentage change in medical expense resources. For example, the exponential regression coefficient (1.2) was presented as 1.2-fold growth in medical expense resources relative to the reference group. The no-rehabilitation group had lower total medical expenses than the within 2 weeks group (0.01-fold). The after 2 weeks group had higher total medical expense than the within 2 weeks group (1.07-fold).
| Table II. Results of the multiple regression analysis of total medical expenses |
| Variable | Total medical expenses Exp. (β)a | p-value |
| Timing of rehabilitationb | | |
| After 2 weeks | 1.07 | 0.0211 |
| No rehabilitation | 0.01 | < 0.0001 |
| CCS | 1.01 | 0.1630 |
| Age | 1.00 | 0.6449 |
| Gender , m | 1.03 | 0.1063 |
| Exemption from cost sharing, yes | 0.93 | 0.0049 |
| F | 25,390.1 | < 0.0001 |
| Adj R2 | 0.894 | |
| aExp. (β) = exponentiated regression coefficients. bAbove items were compared with the within 2 weeks group, the OR of timing of rehabilitation were from the model in that CCS, age, gender and exemption from cost sharing were controlled. CCS: Charlson Comorbidity Scores. |
Logistic regression was performed to analyse the effect of rehabilitation timing on post-TKA-associated complications and medical expenses among patients 1 year after TKA (Table III). After adjusting for the effect of the confounding variables (including patients’ gender, age, exemption status for cost sharing and CCS), the after 2 weeks group had higher odds by 1.66-fold and 2.07-fold than the within 2 weeks group, respectively.
| Table III. Results of logistic regression analysis on prosthetic infection (PI) and deep vein thrombosis (DVT) after total knee arthroplasty |
| Variable | PI | | DVT |
| OR | 95% CI of OR | p-value | | OR | 95% CI of OR | p-value |
| Timing of rehabilitationa | | | | | | | |
| After 2 weeks | 1.66 | 1.22–2.25 | 0.0012 | | 2.07 | 1.36–3.15 | 0.0007 |
| No rehabilitation | 1.29 | 1.01–1.66 | 0.0409 | | 1.51 | 1.10–2.07 | 0.0099 |
| CCS | 1.06 | 1.00–1.11 | 0.0395 | | 1.03 | 0.99–1.07 | 0.2170 |
| Age | 0.99 | 0.97–0.99 | 0.0192 | | 1.11 | 1.02–1.21 | 0.0135 |
| Gender | | | | | | | |
| Male | 1.96 | 1.58–2.44 | < 0.0001 | | 1.00 | 0.98–1.02 | 0.1916 |
| Exemption from cost sharing | | | | | | | |
| Yes | 1.15 | 0.86–1.52 | 0.3474 | | 1.03 | 0.68–1.55 | 0.8981 |
| LR test | | 198.46 | < 0.0001 | | | 41.99 | < 0.0001 |
| Cb | | 0.716 | | | | 0.619 | |
| aAbove items were compared with the within 2 weeks group, the OR of timing of rehabilitation was from the model in that CCS, age, gender and exemption from cost sharing were controlled. bC is equivalent to the well-known measure receiver operating characteristic curve. C ranges from 0.5 to 1, where 0.5 corresponds to the model randomly predicting the response, and a 1 correspond to the model perfectly discriminating the response. CI; confidence interval; CCS: Charlson Comorbidity Scores; OR: odds ratio; LR test: likelihood ratio test. |
DISCUSSION
The results of this study suggest that rehabilitation within 2 weeks after TKA lowers the odds of acquiring PI and DVT compared with the other 2 rehabilitation schedules. Although total medical expenses in the no rehabilitation group were the lowest, the results demonstrate that patients who received early rehabilitation after TKA had much lower medical expenses than patients who received the later rehabilitation. These findings have important implications for decision-making and for health policymakers establishing new standards for insurance payment.
It is not clear why patients in the no-rehabilitation group did not receive any rehabilitation. Patients who received rehabilitation within 2 weeks after discharge had a lower rate of post-TKA complications than patients who received rehabilitation more than 2 weeks after discharge. This finding suggests that the timing of rehabilitation may be a factor contributing to post-TKA complications. Previous studies have indicated that age, gender, health insurance status, comorbidities and volume of TKA at a hospital could contribute to higher rates of post-TKA infection (5). DVT was caused mainly by vascular injury due to surgery and a decreased level of activity because of post-operational pain (20). Zuckerman et al. (21) found that patients who receive rehabilitation after TKA were less likely to develop complications requiring intensive care. Sherrington & Lord (22) found that post-surgical rehabilitation improved the patients’ muscle strength and agility. None of these studies were able to show a correlation between rehabilitation timing and the occurrence of post-TKA complications. Notably, there are no standard guidelines for appropriate rehabilitation timing. Most TKA patients re-visit their surgeons to have their stitches removed in the second week after surgery. Based on the findings of this study, 2 weeks may be an appropriate time to evaluate the quality of rehabilitation or to order rehabilitation for TKA patients.
Secondly, this study found that patients who received rehabilitation within 2 weeks after discharge from TKA utilized outpatient, inpatient, and emergency services related to PI and DVT less than those who received rehabilitation more than 2 weeks after TKA, but more than those who did not receive rehabilitation after TKA. In this study, total medical expenses were the sum of rehabilitation service expenses and medical expenses related to DVT and PI; therefore, we speculate that the reason the no rehabilitation group had lower total medical expenses than the other 2 groups was that they did not incur rehabilitation expenses. In addition, because this study only tracked the medical expenses within 1 year after discharge, some of the follow-up PI and DVT expenses may have been excluded, resulting in underestimation of medical expenses related to major complications. Despite this, the study indicates an impact of rehabilitation timing on medical expenses from early and delayed rehabilitation. The study showed that total medical expenses of the within 2 week group were 66.6% of those of the after 2 week group, even after controlling for age, gender, exemption from cost sharing and CCS. Previous studies have shown that post-operative rehabilitation can reduce healthcare expenses if properly executed. For instance, Husni et al. indicated that patients managed on a full clinical pathway (including physical therapy) had a mean length of stay 0.5 days shorter than patients not managed on a pathway (23). Larsen et al. (24) found the accelerated peri-operative rehabilitation protocol to be significantly less costly than the standard protocol, with an average reduction in cost of 18,880 Danish kroner (approximately 4,000 USD). Mahomed et al. (25) found that the total episode-of-care costs (in Canadian dollars (CanD)) for the inpatient rehabilitation and home-based rehabilitation arms were 14,532 CanD and 11,082 CanD, respectively. However, there were no differences in pain, functional outcome, or patient satisfaction between the group that received home-based rehabilitation and the group that received inpatient rehabilitation. This finding also indicates that, regardless of where patients receive rehabilitation, analysis of post-TKA outcomes is informative. Our study further notes that the first 2 weeks after TKA are a good time to receive rehabilitation, which may result in the utilization of fewer medical services.
Thirdly, our findings carry special meaning for those who craft health policy. Because health insurance companies want to control over-utilization of medical services by employing DRGs, many hospitals adopt CP to control quality and limit costs in response (26). However, if a CP is poorly designed, it may not improve patients’ health after discharge from TKA. In Taiwan, many hospitals do not include rehabilitation as an optional procedure in the TKA CP because the BNHI does not require it. As a result, many orthopaedic doctors rarely consult rehabilitation doctors to address patients’ rehabilitation needs. In contrast, orthopaedic doctors in the USA often consult with the rehabilitation department the day before surgery and frequently set the first off-bed time for rehabilitation within 2–8 days after surgery, which is atypical in Taiwan (27). In addition, many TKA patients are not educated prior to surgery about the importance of rehabilitation (28), resulting in poor health outcomes and unnecessary medical expenses.
Some studies have indicated that the extent of rehabilitation depended on either personal reasons or accessibility to medical services after discharge (14). However, because Taiwan’s health insurance does not restrict accessibility to medical services or frequency of use, patients are free to choose where and when to seek medical attention. In this context, accessibility to medical care is widely available. Therefore, it is a lack of coordination between physicians that may prevent patients from receiving appropriate rehabilitation in a timely fashion.
Limitations
There are 3 main limitations in this study. First, this study uses NHIRD data for all analyses. Although the NHIRD is a population-based administrative database containing information for 23 million Taiwanese, some coding errors might exist in the database; such errors could underestimate medical expenses as well as the occurrence of PI and DVT. However, because the BNHI has closely monitored TKA and related claims before and after TKA and the diagnosis of PI and DVT are not difficult, the influence of misdiagnosis should be minimal. Secondly, there is likely to be residual confounding in the study results. Therefore, in this study, the total medical expenses only included the rehabilitation expenses related to rehabilitation treatment services in the index visit as well as outpatient and inpatient expenses related to PI and DVT within 1 year after discharge. In addition, because the total medical expenses did not fit a normal distribution, the study used a logarithmic function to transform these expenses before regression analysis. In addition, the study included the variables of age, gender, CCS and exemption from cost sharing as control variables in the regression model to minimize confounding of the actual total medical expenses. Through these methods, we believe our study results more accurately reflect the real impact of TKA rehabilitation timing on medical expenses within 1 year after discharge. Thirdly, this study explored whether the timing of TKA rehabilitation was related to the medical expenses and complications within 1 year after discharge and whether the patients starting rehabilitation within 2 weeks after TKA would have a better prognosis and fewer medical expenses in the following year. However, the further relationship between the exact timing of rehabilitation and the outcome of TKA should be confirmed. The study suggests that future researchers could conduct clinical trials to verify the relationship between the timing of rehabilitation and post-surgical prognosis.
ACKNOWLEDGMENT
The authors thank Miss Chun-Pei Weng who assisted us to revise the discussion section of this manuscript.
References