Mikhail Saltychev, MD1, Katri Laimi, PhD2,3, Ashraf El-Metwally, PhD4,5, Tuula Oksanen, PhD6,7, Jaana Pentti,BSc6, Marianna Virtanen, PhD6, Anne Kouvonen, PhD8, Mika Kivimäki, PhD 6,9 and Jussi Vahtera, PhD3,6
From the 1Department of Rehabilitation, 2Department of Physical and Rehabilitation Medicine, Turku University Hospital, 3Department of Public Health, University of Turku and Turku University Hospital, Turku, Finland, 4King Abdullah International Medical Research Center, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Kingdom of Saudi Arabia, 5Epidemiology Group, University of Aberdeen, Aberdeen, UK, 6Finnish Institute of Occupational Health, Helsinki, Finland, 7Department of Society, Human Development and Health, Harvard School of Public Health, Boston, MA, USA, 8Warsaw School of Social Sciences and Humanities, Wroclaw Faculty, Wroclaw, Poland and 9Department of Behavioral Sciences, University of Helsinki, Finland
Objective: To evaluate the effect of a 4-week primary prevention programme on health-risk behaviours amongst employees at increased risk of work incapacity.
METHODS: Based on survey data and health records from 53,416 public sector employees in Finland, we identified 872 employees who participated in early rehabilitation after the baseline survey. We selected 2,440 propensity-score-matched controls for these rehabilitants. Changes in the prevalence of physical inactivity, obesity, heavy drinking, and smoking, as well as in the intensity of leisure-time physical activity, weight, and alcohol consumption after the intervention were examined between the baseline and two subsequent surveys representing short-term (mean follow-up 1.7 years) and long-term (mean 5.8 years) follow-ups.
RESULTS: There were no statistically significant differences between the rehabilitants and controls in terms of changes in weight, alcohol consumption, intensity of leisure-time physical activity, or prevalence of obesity, heavy drinking and physical inactivity during short-term or long-term follow-ups. During short-term follow-up, a higher rate of smoking cessation was observed for rehabilitants than controls (31.7% vs. 20.2%, p = 0.037).
CONCLUSION: Vocationally oriented multidisciplinary early rehabilitation had little effect on health risk behaviours.
Key words: health behaviour change; health risk behaviour; propensity score; modifiable risks.
J Rehabil Med 2012; 44: 370–377
Guarantor: Jussi Vahtera, Department of Public Health, University of Turku, Turku, Finland. E-mail: jussi.vahtera@ttl.fi
Submitted May 8, 2011; accepted December 13, 2011
Introduction
Tobacco smoking, alcohol consumption, obesity, poor diet and physical inactivity are the most important potentially modifiable behaviour-related risk factors responsible for over half of the disease burden in developed countries (1). Furthermore, a particular health risk behaviour rarely occurs alone. Instead, they tend to co-occur, causing multiplied risk of disease and premature death (2, 3). For example, only 3% of all adults in the USA have succeeded to avoid all 4 of the major health risk behaviours: smoking, overweight, physical inactivity and poor diet (4).
In addition to the co-occurrence of health risk behaviours, a co-variation of multiple health behavioural change has been observed. This implies that successful improvement in one health behaviour can lead to improvement in other health behaviours (5). Thus, public health professionals are trying to develop effective and efficient measures to reduce not just one, but multiple health risk behaviours simultaneously over the course of the same intervention programme. These measures should also take into account the contextual environment in which the person lives and works (6, 7). Multiple health behavioural changes to prevent cardiovascular diseases have been studied widely during the last few decades (8), but the evidence on successful measures to affect health risk behaviours remains inconclusive (2, 5, 9, 10).
Multidisciplinary prevention or rehabilitation programmes may constitute a means of helping participants make positive changes in their health behaviours, as these changes are associated with better health, assuring the work ability of the participants (11–16). In the present study, we examined the most common multidisciplinary rehabilitation programme in Finland, which aims at preventing long-term work disability. The programme includes physical and psychological training targeted at achieving multiple positive health behavioural changes. Although this preventive programme has been used since the early 1980s, only a few studies have evaluated its effectiveness in terms of health behavioural changes. These studies, mostly conducted without a control group and based on a relatively small number of participants (17–21), found no improvement in physical activity levels among participants (18, 19). However, we are not aware of previous studies that have simultaneously examined the effectiveness of this programme on multiple behaviour-related risk factors, such as physical inactivity, smoking, overweight, and alcohol abuse. We have reported previously that the programme is of limited value in reducing the risk of a long-term work disability (22); the hazard ratio for incident all-cause work disability was 0.98 (95% confidence interval (CI) 0.76–1.25) in cases compared with their propensity score matched controls. The corresponding hazard ratios for diagnosis-specific work disability was 0.86 (95% CI 0.57–1.30) for musculoskeletal diseases and 1.08 (95% CI 0.67–1.74) for mental disorders.
The objective of this study was to evaluate the short- and long-term effects of a vocationally oriented, in-patient, multidisciplinary preventive programme on smoking cessation, weight change, increase in leisure-time physical activity, and decrease in alcohol consumption.
Methods
Study population
Finnish Public Sector Study. The present study is part of the Finnish Public Sector Study (FPSS), which is an ongoing prospective study amongst employees working in 10 towns and 21 hospitals. The study was approved by the ethics committee of the Finnish Institute of Occupational Health. The study covers all 151,618 employees with a ≥ 6 month job contract in any year from 1991/1996 to 2005 in 10 towns and 6 hospital districts in Finland. Questionnaire surveys targeted 94,494 employees who were working in the years 1997–1998 (phase 1, sub-cohort), 2000–2002 (phase 2), or 2004–2005 (phase 3). All of the respondents have been followed with repeated surveys (2006, phase 4; 2008–2009, phase 5; 2010, phase 6). In phases 1–3 and phase 5, identifiable questionnaire data on psychosocial factors at work, individual factors, health, and health behaviours were gathered. Through the use of the unique personal identification codes that are assigned to all citizens in Finland, all of the participants have been linked to employers’ records and national health registers.
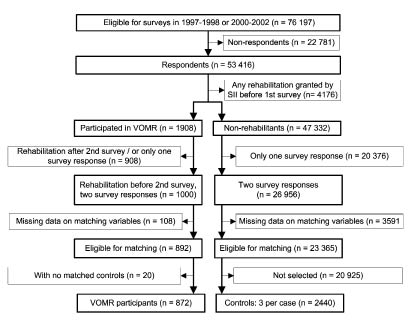
Case-control selection procedure. We used data from phases 1–3 and 5 and included those who responded to 3 consequent identifiable surveys. The first survey response was considered as the baseline (i.e. 1997–1998 or 2000–02) and the following surveys as the first (2000–2002 or 2004–2005) and second follow-ups (2004–2005 or 2008–2009). The earliest survey response was considered for those who participated in both baseline surveys. This approach yielded a sample of 53,416 employees (response rate 70%, 81% of whom were women). We excluded participants who had been granted any rehabilitation by the Social Insurance Institution of Finland (SII) before the baseline survey (n = 4,176) or with missing data on any of the matching variables (n = 3,699). Eligible cases were those who had entered vocationally oriented medical rehabilitation (VOMR) between the first (baseline) and second (first follow-up) survey. By using propensity score matching (see the next section), we identified a study population of 872 cases and 2440 non-cases of VOMR (Fig. 1).
Fig. 1. Case-control selection procedure. SII: Social Insurance Institution of Finland; VOMR: vocationally oriented medical rehabilitation.
Propensity score matching. We used the propensity score approach to approximate the exchangeability of the comparison groups, which, in theory, would differ only in the receipt of VOMR (23, 24). Propensity score is the conditional probability of being assigned “treatment”, here VOMR, given the observed covariates. In order to calculate the propensity score, we used binary logistic regression models for VOMR (dichotomous outcome) including 24 pre-treatment variables known to be associated with rehabilitation and the health-risk behaviours available in the data, and their interactions with gender, socio-economic status, and age group. Once we had estimated the propensity score, each case was matched with 1–3 controls (non-VOMR recipients) according to a pre-defined calliper width of +0.01, and the unmatched cases were discarded, resulting in a total of 3,312 subjects (872 participants and 2,440 propensity-score-matched controls) for the statistical analysis (Table I). The balance achieved by matching was studied using the χ2 test.
| Table I. Definitions of the variables used in the propensity score matching |
| Variable | Definition |
| Demographic characteristics | |
| Age groupa | ≤ 40 years, 41–50 years, or ≥ 51 years |
| Gendera | Male/female |
| Occupational gradea | International Standard Classification of Occupations (ISCO) grades: 1–2 – managers and professionals, 3 – technicians and associate professionals, 4 – clerks, 5 – service workers, or 6–9 – manual workers |
| Educational levelb | High school: yes/no |
| Marital statusb | Married or cohabiting vs single, divorced or widowed |
| Type of employera | Municipality or hospital district |
| Residential regiona | Southern, Northern, or Central Finland |
| Work characteristics | |
| Type of job contracta | Permanent/temporary |
| Length of the contracta | < 1 year, 1–9 years, or ≥ 10 years |
| Shift workb | Yes/no |
| Intention to leave workb | Continue the job, switch jobs, or give up the job |
| Job insecurityb | Two questions, which estimate the threat of long-term unemployment or dismissal (from 1 = very little to 5 = very much). A mean score was computed and divided into tertiles. |
| Job controlb | 9 items derived from the Job Content Questionnaire |
| Health behaviour | |
| Current smokingb | Yes/no |
| Heavy drinkingb | Yes (> 210 g pure alcohol per week)/no |
| Obesityb | Yes (body mass index (BMI) ≥ 30 kg/m2))/no |
| Physical inactivityb | Yes (≤ 2 metabolic equivalent task (MET) h/day)/no |
| Health indicators | |
| Sickness absencec | Yes (> 60 absence days during the last 3 years)/no (0 or 1–60 absence days) |
| Psychological distressb | Yes (psychological distress for at least 4 items of GHQf)/no |
| Anxietyb | 6-item Trait Anxiety Inventory: low, intermediate, or high anxiety |
| Self-rated healthb | Sub-optimal (average or worse)/optimal (good or very good health) |
| Baseline physical healthd | Yes (presence of a chronic diseaseg)/no |
| Use of prescribed painkillerse | Yes (> 30 defined daily dosages during the survey year (ATCh code N02 and M01A))/no |
| Use of prescribed antidepressantse | Yes (> 30 defined daily dosages during the survey year (ATCh code N06A))/no |
| aObtained from employers’ records; bObtained from survey; cObtained from the Sickness Absence Register of the Finnish Social Insurance Institution; dObtained from the Drug Reimbursement Register of the Finnish Social Insurance Institution; eObtained from the Drug Prescription Register of the Finnish Social Insurance Institution; f12-item General Health Questionnaire (GHQ); gIndicated by special reimbursement for the medical treatment of hypertension, cardiac failure, ischaemic heart disease, diabetes, asthma or other chronic obstructive lung disease, and rheumatoid arthritis; hAnatomical therapeutic chemical. |
INTERVENTION: vocationally oriented multidisciplinary rehabilitation
In Finland, VOMR is the most common rehabilitation programme sponsored by SII. It accounts for 12.3% of SII’s annual rehabilitation budget (25). In 2009, the median age of the VOMR participants was 50 years (25).
VOMR is a group-based multidisciplinary rehabilitation programme targeted towards employees at workplaces and occupations in which workers are subjected to considerable physical, mental or social strain that may lead to health problems and a deterioration in work capacity. Briefly, one of its selection criteria is the absence of recent long-term sick-leaves or severe long-standing illnesses.
The VOMR programme contains 3–4 periods of extensive multimodal and multiprofessional inpatient rehabilitation (a total of 15–21 days) implemented as group-based (8–10 persons) and individual sessions of supervised activity 4–6 h per day. Between the inpatient periods, the participants are expected to follow an individual exercise plan at home, which usually consists of self-reliant physical activities and psychological exercises. The participants are guided by professionals, the aim being better aerobic capacity, muscle strength and endurance through the adoption of more regular and comprehensive leisure-time physical activity and healthy dietary habits, cessation of smoking, and reduction in alcohol consumption (26).
Outcome: change in behaviour-related risk factors
Using 3 repeated questionnaire surveys, we measured two types of outcome. Firstly, we measured the changes in the prevalences of obesity, leisure-time physical inactivity, smoking, and heavy drinking. Secondly, we measured the changes in weight, intensity of leisure-time physical activity, and alcohol consumption.
The body mass index (BMI; kg/m2) was derived from self-reported weight and height and dichotomized to indicate obesity (BMI ≥ 30). The change in self-reported weight (kg) was measured for those who were obese or non-obese at baseline.
The participants’ reports of the quantity of their physical activity equivalent to walking, brisk walking, jogging, or running was used to estimate the metabolic equivalent of task (MET) hours per day. Physical inactivity was defined as ≤ 2 MET h (no/yes) (27). The change in MET hours/day was assessed for those who were physically active and for those who were physically inactive at baseline.
Smoking status (never, ex-smoker and current smoker) was operationalized as current smoking (yes/no). The change in smoking status amongst the baseline smokers was used to identify smoking cessation.
Participants reported their mean weekly consumption of beer, wine and spirits in units. The units were converted into grams of pure alcohol, and > 210 g pure alcohol per week was considered the cut-off for heavy drinking (no/yes) (28, 29). Binge drinking was determined by enquiring whether the participant had passed out due to heavy alcohol consumption once or more often during the past 12 months (30). The Finnish term used for “pass-out” refers to alcohol-related loss of consciousness, but without reference to loss of memory (blackout) (30). The change in alcohol consumption (g/week) was measured by the heavy drinking status at baseline.
Statistical analysis
We applied repeated-measures log-binomial regression analysis with the generalized estimating equations (GEE) method for studying the changes in the prevalence of the behaviour-related risk factors of the participants and controls (31, 32). The results were reported as percentages of the estimated prevalence, prevalence ratios and their 95% confidence limits and p-values.
We performed a repeated-measures analysis of variance to study the changes in the continuous variables (weight, physical activity and alcohol consumption) and reported the results as the mean values, their 95% confidence limits and p-values. Data on the baseline characteristics were gathered before the beginning of the intervention (mean 1.8 years (SD 1.07)). The short-term follow-up ended with the first and the long-term follow-up with the second follow-up survey. The follow-up began immediately after the beginning of the rehabilitation. The first follow-up survey (short-term follow-up) took place on average 1.7 years (SD 1.01, range 0.003–4.5 years) after the start of the rehabilitation; for 19% of the rehabilitants, the rehabilitation programme was not yet completed. The second follow-up survey (long-term follow-up) was performed on average 5.8 years (SD 1.13, range 3.12–9.16) after the rehabilitation.
All of the statistical analyses were performed using SAS© 9.2 software (SAS Institute, Cary, NC, USA).
Results
The prevalences of the health risk behaviours were relatively low amongst the participants before the intervention: only 13% were smokers, 22% were physically inactive, 10% were obese and 7% were heavy drinking. Three-quarters of the participants reported good self-rated health and a similar proportion did not use prescribed painkillers. Only 5% of the participants used prescribed antidepressants (Table II). Supporting the success of the propensity score matching, no differences were observed between the participants and their controls with respect to the individual variables used to calculate the propensity score, except for employer type (Table II).
| Table II. Differences between the cases and controls as regards the covariates after the propensity score matching |
| Covariates used in the propensity score matching | Participants (n = 872) n (%) | Controls (n = 2440) n (%) | χ2-test p-value |
| Propensity score, mean (range) | 0.111 (0.001–0.548) | 0.093 (0.001–0.549) | |
| Gender | | | | | 0.162 |
| Women | 789 (90) | 2,166 (89) | |
| Men | 83 (10) | 274 (11) | |
| Age group, years | | | | | 0.055 |
| ≤ 40 | 138 (16) | 410 (17) | |
| 41–50 | 532 (61) | 1,558 (64) | |
| ≥ 51 | 202 (23) | 472 (19) | |
| ISCO gradea | | | | | 0.946 |
| 1–2 (managers) | 310 (36) | 894 (37) | |
| 3 | 223 (26) | 594 (24) | |
| 4 | 41 (5) | 109 (4) | |
| 5 | 205 (24) | 585 (24) | |
| 6–9 (manual) | 93 (11) | 258 (11) | |
| Type of employer | | | | | 0.002 |
| Municipality | 590 (68) | 1,785 (73) | |
| Hospital district | 282 (32) | 655 (27) | |
| Residential region | | | | | 0.353 |
| Southern Finland | 500 (57) | 1,396 (57) | |
| Central Finland | 259 (30) 113 (13) | 684 (28) | |
| Northern Finland | 360 (15) | |
| Table II. Differences between the cases and controls as regards the covariates after the propensity score matching |
| Covariates used in the propensity score matching | Participants (n = 872) n (%) | Controls (n = 2440) n (%) | χ2-test p-value |
| Propensity score, mean (range) | 0.111 (0.001–0.548) | 0.093 (0.001–0.549) | |
| Gender | | | | | 0.162 |
| Women | 789 (90) | 2,166 (89) | |
| Men | 83 (10) | 274 (11) | |
| Age group, years | | | | | 0.055 |
| ≤ 40 | 138 (16) | 410 (17) | |
| 41–50 | 532 (61) | 1,558 (64) | |
| ≥ 51 | 202 (23) | 472 (19) | |
| ISCO gradea | | | | | 0.946 |
| 1–2 (managers) | 310 (36) | 894 (37) | |
| 3 | 223 (26) | 594 (24) | |
| 4 | 41 (5) | 109 (4) | |
| 5 | 205 (24) | 585 (24) | |
| 6–9 (manual) | 93 (11) | 258 (11) | |
| Type of employer | | | | | 0.002 |
| Municipality | 590 (68) | 1,785 (73) | |
| Hospital district | 282 (32) | 655 (27) | |
| Residential region | | | | | 0.353 |
| Southern Finland | 500 (57) | 1,396 (57) | |
| Central Finland | 259 (30) 113 (13) | 684 (28) | |
| Northern Finland | 360 (15) | |
| Marital status | | | | | 0.869 |
| Married/cohabiting | 672 (77) | 1,887 (77) | |
| Single | 200 (23) | 553 (23) | |
| High educational level | | | | | 0.440 |
| No | 406 (47) | 1,099 (45) | |
| Yes | 466 (53 | 1,341 (55) | |
| Job contract | | | | | 0.665 |
| Permanent | 810 (93) | 2,277 (93) | |
| Fixed-term | 62 (7) | 163 (7) | |
| Length of job contract,years | | | | 0.286 |
| < 1 | 156 (18) | 480 (20) | |
| 1–9 | 599 (69) | 1,673 (69) | |
| ≥ 10 | 117 (13) | 287 (12) | |
| Shift work | | | | | 0.679 |
| No | 560 (64) | 1,586 (65) | |
| Yes | 312 (36) | 854 (35) | |
| Intention to leave work | | | | | 0.450 |
| Continue the job | 462 (53) | 1,260 (52) | |
| Switch jobs | 221 (25) | 672 (28) | |
| Give up the job | 189 (22) | 508 (21) | |
| Job insecurity | | | | | 0.916 |
| Low | 396 (45) | 1,090 (45) | |
| Intermediate | 352 (40) | 1,004 (41) | |
| High | 124 (14) | 346 (14) | |
| Job control | | | | | 0.594 |
| Low | 266 (31) | 753 (31) | |
| Intermediate | 305 (35) | 889 (36) | |
| High | 301 (35) | 798 (33) | |
| Obesity | | | | | 0.963 |
| No | 781 (90) | 2,184 (90) | |
| Yes | 91 (10) | 256 (10) | |
| Smoking | | | 0.353 |
| No | 758 (87) | 2,090 (86) | |
| Yes | 114 (13) | 350 (14) | |
| Alcohol consumption, g/week | | | | 0.814 |
| 0–210 | 807 (93) 65 (7) | 2,264 (93) | |
| > 210 | 176 (7) | |
| Physical inactivity | | | | | 0.897 |
| No | 683 (78) | 1,906 (78) | |
| | | | |
| | | | | |
| | | | |
| | | | |
| | | | |
| | | | | |
| | | | |
| | | | |
| | | | | | |
| | | | |
| | | | |
| | | | | | |
| | | | |
| | | | |
| | | | | | |
| | | | |
| | | | |
| | | | |
| | | | | |
| | | | |
| | | |
| | | | | | |
| | | | |
| | | | |
| |
Changes in the prevalences of behaviour-related risk factors
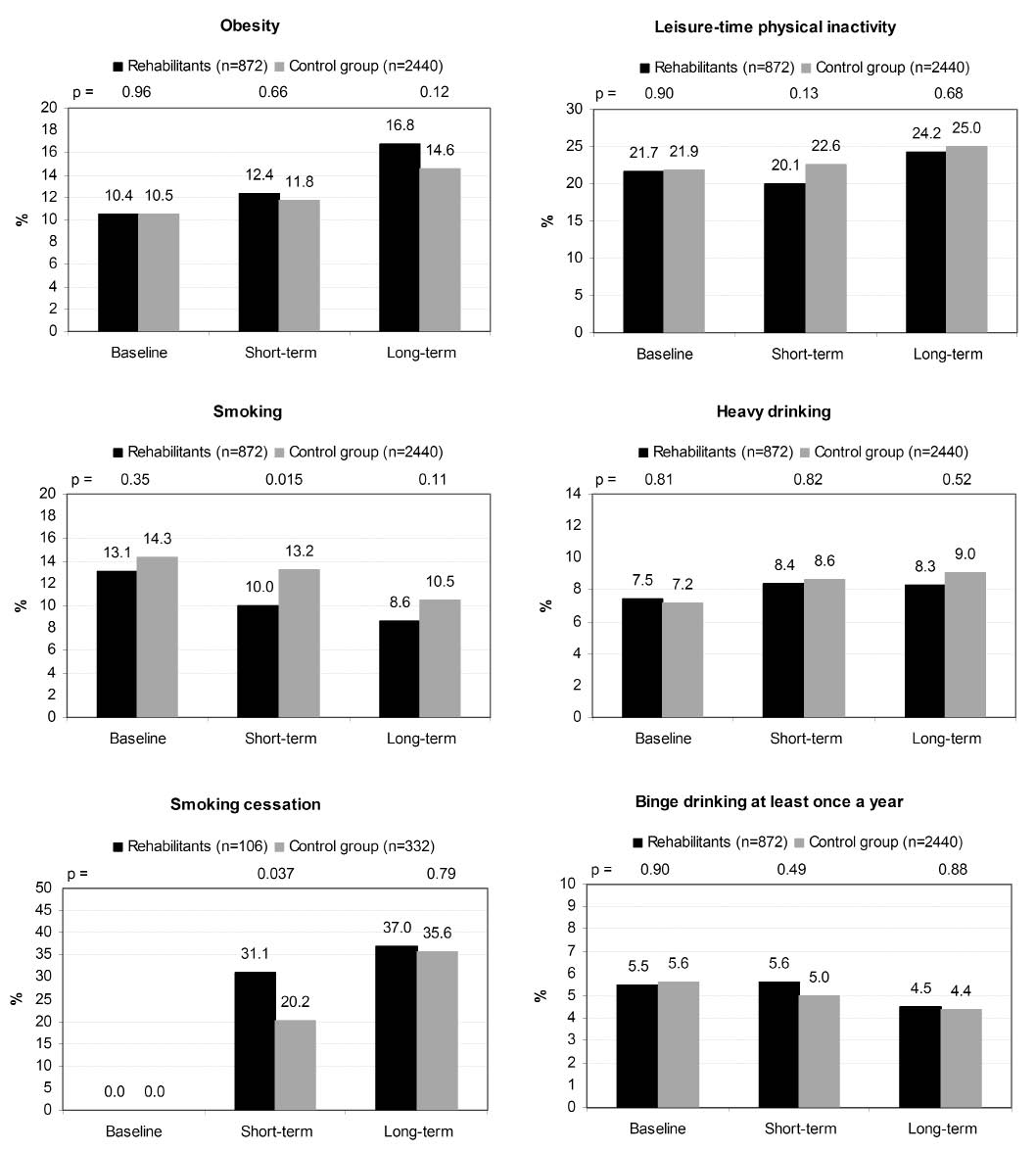
Fig. 2 shows the changes in the prevalence of behaviour-related risk factors shortly after the intervention (mean 1.7 years (SD 1.01, range 0.003–4.55)) and in the long-term follow-up (mean 5.8 years (SD 1.13, range 3.12–9.16)). The prevalence of obesity increased amongst the participants and controls (by 6.4% and 4.1%, respectively) during an entire follow-up without a significant difference between the two groups. The prevalence of smoking decreased in both groups during an entire follow-up, amongst the participants by 4.5% and amongst the controls by 3.8%. Although the participants quit smoking (p = 0.037) more often than the controls did during a short-term follow-up, this difference disappeared during a long-term follow-up. The prevalence of physical inactivity increased slightly amongst the participants and controls in the long-term follow-up (by 2.5% and 3.1%, respectively) without a significant difference between the groups (p =0.68). The prevalence of heavy and binge drinking remained almost unchanged in both groups.
Fig. 2. Prevalence of participants’ behaviour-related risk factors at baseline and at short-term (mean 20 months) and long-term (mean 70 months) follow-ups in comparison with controls.
Changes in weight, intensity of physical activity, and alcohol consumption
Table III shows the changes in weight (kg), intensity of physical activity (MET h/day), and alcohol consumption (g/week). There was a minor increase in body weight amongst the participants who were not obese at baseline when they were compared with their controls (mean increase by 3.5 kg and 2.8 kg, respectively) in the long-term follow-up (p = 0.005). Amongst the participants who were obese at baseline, no significant difference in weight change was observed. The physically inactive cases and controls at baseline increased their physical activity in the short-term follow-up (mean 1.66 and 1.69 MET h/day, respectively), and the improvement also lasted through the entire follow-up (mean 1.46 and 1.71 MET h/day, respectively), with no difference between the two groups. At the same time, the cases and controls physically active at baseline slightly reduced their activity throughout the entire follow-up. Also in relation to changes in alcohol consumption, no significant difference was observed between the two groups during follow-up.
| Table III. Changes in the behaviour-related risk factors of the participants and controls |
| Type of change and risks before rehabilitation | Short-term follow-up | Long-term follow-up |
| Mean | 95% CI | p-value | Mean | 95% CI | p-value |
| Increase in weight, kg | | | | | | |
| No obesity at baseline | | | | | | |
| Participants (781) | 1.80 | 1.51 to 2.10 | 0.010 | 3.45 | 3.08 to 3.83 | 0.005 |
| Controls (2184) | 1.36 | 1.20 to 1.52 | | 2.83 | 2.61 to 3.05 | |
| Obesity at baseline | | | | | | |
| Participants (91) | –0.26 | –1.98 to 1.46 | 0.651 | 0.03 | –2.23 to 2.30 | 0.053 |
| Controls (256) | 0.18 | –0.63 to 1.00 | | 2.47 | 1.51 to 3.42 | |
| Increase in physical activity, MET h/day | | | | | | |
| No physical inactivity at baseline | | | | | | |
| Participants (683) | –0.59 | –0.89 to –0.29 | 0.835 | –0.76 | –1.10 to –0.41 | 0.275 |
| Controls (1906) | –0.63 | –0.81 to –0.44 | | –0.98 | –1.16 to –0.79 | |
| Physical inactivity at baseline | | | | | | |
| Participants (189) | 1.66 | 1.30 to 2.02 | 0.901 | 1.46 | 1.16 to 1.77 | 0.206 |
| Controls (534) | 1.69 | 1.45 to 1.92 | | 1.71 | 1.48 to 1.95 | |
| Increase in alcohol consumption, g/week | | | | | | |
| No heavy drinking at baseline | | | | | | |
| Participants (807) | 9.46 | 5.31 to 13.6 | 0.402 | 8.08 | 3.44 to 12.7 | 0.145 |
| Controls (2264) | 11.68 | 8.55 to 15.8 | | 12.11 | 9.35 to 14.87 | |
| Heavy drinking at baseline | | | | | | |
| Participants (65) | –37.34 | –75.7 to 1.07 | 0.054 | –86.35 | –116 to –56.7 | 0.679 |
| Controls (176) | –84.16 | –112 to –56.1 | | –95.22 | –125 to –65.4 | |
| MET: metabolic equivalent of task; CI: confidence interval. |
As it is possible that the longest duration of the short-term follow-up in some cases exceeded the shortest duration of the long-term follow-up, we ran a sensitivity analysis including the 750 cases with short-term follow-up of 3 years or less, and the long-term follow-up was at least 4 years. The results did not differ from those of the main analyses: we observed no benefits other than a higher likelihood of quitting smoking in the short-term among the cases (data not shown).
Discussion
In this prospective cohort study of 872 public sector employees who underwent an in-patient primary prevention programme to reduce the risk of early retirement on health grounds, no evidence of a favourable change in behaviour-related health risks was found when they were compared with their 2,440 propensity-score-matched controls, except for a temporary decrease in smoking. The aim of the programme was to prevent long-term work disability by helping the participants to adopt a healthier lifestyle composed of more regular and more comprehensive leisure-time physical activities, healthy dietary habits, a reduction in or cessation of smoking, and a reduction in alcohol consumption.
Our finding that obesity, leisure-time physical inactivity, and heavy drinking had not changed in comparison with the controls’ respective behaviours after the rehabilitation is in line with the results of most previous studies on modifiable health risk behaviours, which also reported only minor or null effects of individual-based primary prevention in a low-risk population (2, 33–35). Improving participants’ motivations and skills to endure more-intense leisure-time physical activity is the main tool used by VOMR teams to achieve changes in other health behaviours as well. However, as in previous studies of VOMR and other preventive rehabilitation programmes, VOMR seemed to be ineffective in improving the leisure-time physical activity of the participants (18, 19, 36). We are not aware of previous studies on the effectiveness of VOMR with respect to smoking, weight control, or alcohol consumption with which to compare these results. In relation to smoking, our results are in accordance with the results of a previous study reporting that multidisciplinary rehabilitation may be effective in helping participants to quit smoking (37). However, the improvement found in our study was not sustained in the long-term.
A failure to select participants at increased risk of early retirement is a potential explanation for the inability of VOMR to contribute to health behavioural changes in our study. Indeed, VOMR is more likely to be granted to employees with few known risk factors (38). Failed selection may partially explain the inability of VOMR to affect the health behaviours of the participants. Because all of the 4 health risk behaviours studied have been shown to have an impact on work disability (11–16), the selection of low-risk participants to VOMR is potentially weakening the possibilities of the intervention to decrease the risk of work disability, the ultimate goal of VOMR.
The strengths of this prospective study are its large study population and its use of propensity score matching based on an explicit counterfactual framework. Although the distribution of the covariates used to derive the propensity score is the same for cases and controls, propensity-based matching might not remove bias due to unmeasured confounding when a strong selection bias exists (39). Information on patient prognosis and physician decision-making behaviours is typically not available in observational data-sets, such as ours, although the likelihood of being treated depends on clinical judgment and referral selection. Inability to take these factors into account is likely to result in an overestimation of the benefit in case lower-risk patients were selected for treatment and an underestimation if higher-risk participants entered rehabilitation. However, propensity score matching is likely to reduce such bias, given that the distribution of unmeasured prognostic factors are more likely to be similar when considering therapies with similar clinical indications and risk. Under such conditions, randomized clinical trials and observational studies have been shown to present the greatest similarities (40, 41). Because we focused on a low-risk population (22, 38) in terms of work disability, strong selection bias and major confounding from unmeasured factors seem unlikely. The study population consisted only of full-time public sector employees from a developed European country, and therefore the generalizability of the findings may be reduced. Our study assessed the effectiveness of VOMR in achieving health behavioural changes only, and hence it is possible that this type of a preventive intervention programme affects other risk factors of early retirement on health grounds, such as levels of experienced work stress, anxiety, psychological distress, or self-rated health.
In conclusion, our results suggest that long-term change in behaviour-related risk factors, such as smoking, obesity, physical inactivity, and heavy drinking, may not be achieved by the vocationally oriented multidisciplinary rehabilitation programme widely used in Finland. Further research is needed to identify the reasons for the apparent ineffectiveness of this costly early intervention programme and to develop more effective preventive measures to reduce modifiable risks in working populations.
Acknowledgements
The Finnish Public Sector Study is supported by the Academy of Finland (projects 124271, 124322, and 132944) and the participating organizations.
REFERENCES