OBJECTIVE: Most children with cerebral palsy have increased muscle tension in the lower extremities, which inevitably leads to abnormal gait characteristics. Proper management of excessive muscle tension is therefore of great importance. The aim of this study was to explore the effects of continuous passive motion on children with cerebral palsy, regarding their lower extremity spastic hypertonia and ambulatory function.
DESIGN: A repeated measures design.
SUBJECTS: Sixteen children with cerebral palsy.
METHODS: Intervention was applied to the subject’s knees with a continuous passive motion device (at velocities of 15 and 0º/s) for 20 min. Effects were evaluated via variables measuring range-of-motion, muscle tone, and ambulatory function before, immediately after, and 30 min after intervention.
RESULTS: For the 15º/s intervention, significant differences were found in time, intervention, and interaction among variables, including active range-of-motion of the knee (increased), relaxation index (increased), Modified Ashworth Scale (decreased), Timed Up-and-Go (decreased), and 6-Minute Walk test (increased). No difference was found in passive range of motion measurements. For the 0º/s control condition, none of the dependent variables demonstrated statistically significant differences.
CONCLUSION: Repetitive passive movement can reduce lower extremity spastic hypertonia in children with cerebral palsy, and improve ambulatory function in terms of walking speed.
Key words: cerebral palsy; spasticity; repetitive passive movement.
J Rehabil Med 2012; 00: 00–00
Correspondence address: Hsin-Yi Kathy Cheng, Graduate Institute of Early Intervention, Chang-Gung University, 259 Wen-Hwa 1st Rd, Kwei-Shan, Tao-Yuan, Taiwan 333. E-mail: kcheng@mail.cgu.edu.tw
Submitted June 23, 2011; accepted November 14, 2011
Introduction
Spastic clinical features occur in 70–80% of subjects with cerebral palsy (CP). These features include, but are not limited to, increased deep tendon reflexes and muscle tone, tremors, weakness, and abnormal gait characteristics, such as scissor gait and toe-walking (1). Spastic hypertonia is one of the most frequently observed phenomena after upper motor neurone lesions, including stroke, head injury, spinal cord injury, CP, etc. (2). A loss of muscle tone inhibition from the brain to the spinal cord, such that the muscles become overactive, results in decreased ability for the subject voluntarily to control muscle activity, and therefore leads to movement dysfunction. In order to prevent long-term structural damage to the lower extremities, and to improve abnormal gait, one of the most important goals is to manage the spastic, hyperactive musculature. Normalizing muscle tone can ease discomfort, and enhance walking ability and daily function, thus promoting independence of living.
Spastic hypertonia is usually managed by means of drug therapy, botulinum toxin injections to the muscle belly, phenol nerve blocks, physical therapy, bracing and surgeries; each of which has its specific indications. Physical therapy ranges from muscle stretching, therapeutic modalities and exercise, to functional training. Clinically, muscle stretching and joint mobilization are considered an integral part of the patient’s daily management of spastic hypertonia. Evidence indicates that, if performed regularly, they can prevent contractures and reduce the severity of spastic tone for several hours (3). Nevertheless, practice suggests that passive stretching has to be applied effectively for approximately 2 h per day to prevent contractures. This is beyond the scope of most physiotherapy services. In addition, prolonged static stretching can be painful or even unbearable, especially for very young children. The painful stretching may be an unpleasant experience for young children, and thus result in avoidance of treatment.
Continuous passive motion (CPM) has been shown to decrease muscle hypertonia and improve the function of the lower extremities in subjects with stroke and spinal cord injury (4–7). In 2006 Wu et al. (4) applied CPM to the ankle joint of stroke patients at a speed of 9 s per cycle for 15 min. They found a significant decrease in spasticity measurements of the ankle and significant performance improvement in the Timed Up and Go test (TUG) and the 10-min walking test. Chang et al. (5) administered a 60-min CPM to the ankle joint of subjects with spinal cord injury at a speed of 3.7 cycles per second. After the intervention, the H-reflex amplitude at the soleus muscle was depressed, and the median of Modified Ashworth Scale (MAS) scores decreased. Bressel & McNair (6) applied continuous passive ankle joint motion to stroke subjects at an angular velocity of 5º/s. They found a decrease in ankle stiffness after CPM intervention. Nuyens et al. (7) applied CPM to the knee joint in stroke patients, using isokinetic apparatus in a series of 10 repetitions at speeds of 60, 180 and 300º/s. The patients presented a significant torque reduction as movements were repeated at all 3 speeds, and the knee muscle electromyographic activity paralleled the variations in torque measurements in flexion conditions.
CPM is usually applied using a CPM device, which provides cyclical movements to the joint through a controlled range of motion, although the exact range depends on the individual joint. Unlike prolonged static stretch, CPM promotes dynamic stretch to the muscles and has been reported to be more effective than static holds on decreasing stiffness of the joint in healthy conditions (8, 9). It can also induce a decrease in spastic hypertonia through a combination of reflexive and mechanical factors (7). CP, similar to stroke and spinal cord injury, is a kind of upper motor neurone lesion featuring mostly spasticity. To our knowledge, no research has been carried out into the effects of CPM on the management of spastic hypertonia and functional improvements in individuals with CP. The purpose of this study was therefore to evaluate whether CPM demonstrates tone-reducing effects on the knee joints and improvements in ambulatory function in subjects with CP.
Material AND Methods
A repeated measures design was used. The independent variables were: CPM intervention (15 and 0º/s) and time (pre-CPM = time 1; post-CPM = time 2; 30 min post-CPM = time 3). The influences of CPM were evaluated via variables including active and passive range of motion (AROM and PROM) for both knee and ankle joints, relaxation index (RI) of Pendulum test, MAS, TUG and 6-Minute Walk test (6MWT).
Subjects
Sixteen children with CP between the ages of 6 and 12 years were recruited for this study. All of them had diagnoses of either spastic diplegia or spastic quadriplegia, total MAS scores for bilateral lower extremities greater than 2, and were able to walk for at least 6 min with or without the use of assistive devices. Inclusion criteria included being able to follow simple commands, and a score of Wechsler Intelligence Scale for Children-IV (WISC-IV) of greater than 70. Exclusion criteria were: subjects with a history that might interfere with the experiment, including: (i) lower extremity surgery within the past 6 months; (ii) botulinum toxin injection within the past 6 months; (iii) knee joint range-of-motion limitation greater than 10º; and (iv) epilepsy. Written informed consent was obtained from all participants and from the parent or guardian of children who met the inclusion requirements. The study was approved by the Institutional Review Board of Chang Gung Memorial Hospital. Subjects were required to stop taking anti-spastic medications 24 hours before the experiment.
Equipment
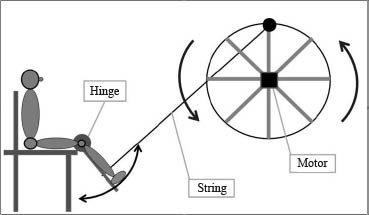
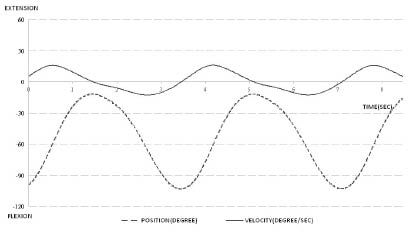
The equipment utilized in this study included electrogoniometers (SG110, Biometrics, Ltd, Cwmfelinfach, Gwent, UK), electromyography (EMG) electrodes (TSD 150A, Biopac System Inc., Santa Barbara, CA, USA) and a self-designed CPM device. The electrogoniometers, taped on the lateral sides of the knee and ankle joints, were used to measure the degree of flexion and extension of the joints. The surface EMG was used to monitor muscle activities during the intervention. The self-designed device was used to provide CPM to the knee joint at a peak angular velocity of 15º/s. This device consisted of a rotary bar driven by a motor (5IK90RGU-AF, Honto Denki Gear Motor Co., Ltd, output: 90 W, range of speed setting: 90–1650 rpm) with a speed-reducing gear (5GU50KB, Honto Denki Gear Motor Co., Ltd, reduction ratio 50:1) mounted on a standing frame, a string attached to the rotary bar on one end and a leg plate on the other, two pulleys, a control box for velocity adjustments, and a back-adjustable metal sitting frame. The whole CPM unit moved the lower leg by pulling the leg plate with a peak angular deflection of 15º/s (Fig. 1). The kinematic performance curves of the leg plate are shown in Fig. 2.
Fig. 1. The self-designed continuous passive motion device that provides continuous passive movements.
Fig. 2. The kinematic performance curves of the leg plate.
Protocol
The subject was seated in a comfortable position, with their back fully supported by the backrest and their legs hanging freely over the side of the metal frame. The seat depth and leg plate were adjusted to fit the subject’s lower extremities. For the application of EMG electrodes, the skin overlying the target muscles was prepared with an alcohol swab. The bipolar active electrodes were applied onto 6 muscles, including the rectus femoris (RF), the vastus medialis oblique (VMO), the biceps femoris (BF), the semi-tendinosus (ST), the tibialis anterior (TA), and the gastrocnemius (GA). A 2-min resting EMG data was collected as baseline.
Following measurement and preparation, each subject received CPM intervention for 20 min. The machine can move the knee in the range from –10º to 120º; however, the actual movement range for each subject was set at 80% of their available knee joint ROM. This range was chosen in order to not evoke a stretch reflex and to increase relaxation. Two angular velocities of movement, 15 and 0º/s, were executed in a counterbalanced order on two separate days. During the 0º/s control condition, the subject sat on the machine with their lower legs fastened to the leg plate with the knee in approximately 20º–30º flexion for 20 min. Subjects watched a self-selected cartoon and were asked to remain seated between times 2 and 3.
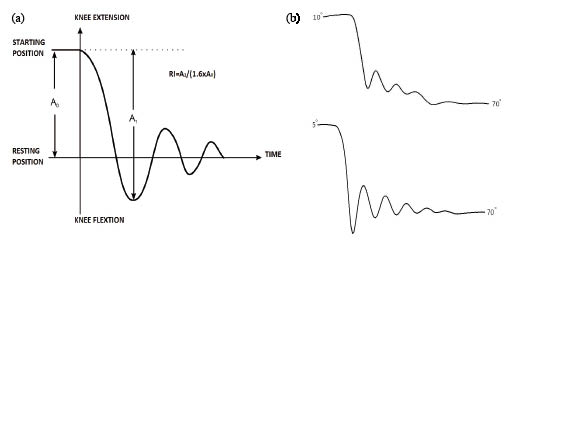
The following measurements were performed immediately before the intervention (time 1), immediately after the intervention (time 2), and 30 min after the intervention (time 3), in the following order: AROM and PROM measurement for knee and ankle joints, Pendulum test, MAS, two trials of TUG, and 6MWT. ROM of the ankle was measured, since the gastrocnemius muscle was moved during the intervention, and any changes in this 2-joint muscle might lead to variation in knee and/or ankle ROM. The Pendulum test evaluated muscle tone by using gravity to provoke stretch reflexes of the knee extensors during passive swinging of the lower limb. The oscillatory movements of the lower leg were captured by an electro-goniometer at the knee joint. The relaxation index was calculated as follows: RI = A1/A0 × 1.6 = (starting angle – first angle)/(starting angle – resting angle) × 1.6 (Fig. 3a) (10). The test-retest reliability of the relaxation index before the intervention was 0.76. MAS with a score of 0–4 was used to assess the resistance of knee flexors to passive movement. The MAS scores of bilateral extremities were added up to represent the muscle tone of the subject’s lower extremities. The TUG and the 6MWT were performed by having the subjects walk with shoes on at their preferred speed with or without assistive devices. The TUG measured the time required for an individual to stand up from a chair with armrests, walk 3 m, turn, walk back to the chair, and sit down. The mean performance time for two trials was calculated. The 6MWT is the distance walked within 6 min. According to the literature, the test-retest reliability values for the TUG (11) and the 6MWT (12) were high for children with CP. The TUG also demonstrated adequate validity in children (11).
Fig. 3. Relaxation Index of the Pendulum test. (a) Formula for Relaxation Index. (b) Graph representation of Pendulum test before and after the intervention in a child with cerebral palsy.
Data processing and analysis
All data were analysed using SPSS version 17.0 statistical software (SPSS Inc., Chicago, IL, USA). Descriptive statistics were used to calculate subjects’ demographics. A two-way repeated measures analysis of variance (ANOVA) (intervention (2) × time (3)) was performed for all variables except MAS. The alpha level was set at p < 0.05. If a repeated measures ANOVA identified a significant difference among the means, multiple comparisons between pairs of means were used to determine where the differences existed with Bonferroni adjustments of alpha level.
For the MAS score, Friedman’s ANOVA was performed. The level of significance was set at p < 0.05. Multiple comparisons were conducted between the paired time frames using Wilcoxon signed-rank procedures with alpha set at 0.017 (0.05/3) to compensate for alpha inflation with multiple testing.
Results
Sixteen children (9 boys and 7 girls, mean age 8.9 years (standard deviation (SD) 2.3)) with CP participated in this study. Eleven subjects had a diagnosis of spastic diplegia and 5 a diagnosis of spastic quadriplegia. The mean MAS score was 4.69 for bilateral lower extremities together. Six of the 16 patients were on anti-spastic medications. Almost all of them were able to walk independently without walking aids, except for 4 subjects who used 4-wheeled walkers for ambulation.
Significant differences were found in time, intervention, and their interaction among variables, including AROM of the knee, RI, MAS, TUG, and 6MWT. Post-hoc analyses revealed differences between times 1 and 2, and times 1 and 3, but not between times 2 and 3, except for the 6MWT. For the 6MWT, differences existed between times 1 and 2, and times 2 and 3, but not times 1 and 3. However, no difference was found in AROM of the ankle, or PROM of the knee and ankle joints.
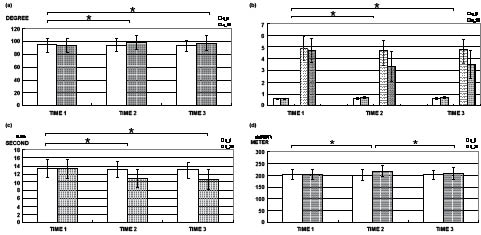
The means and SD for variables that were significantly different were as follows: the AROM of the knee joint before, after, and 30-min after the 15º/s intervention was 93.08º (SD 10.30º), 98.71º (SD 10.64º), and 97.41º (SD 10.52º), respectively (Fig. 4a). For the RI of knee extensors, the values were 0.59 (SD 0.07), 0.72 (SD 0.09), and 0.68 (SD 0.09) at the 3 measurement times. The results of the Pendulum test in one subject before and after CPM intervention are shown in Fig. 3b. For the MAS of knee flexors, the values were 4.69 (SD 1.01), 3.31 (SD 1.25), and 3.50 (SD 1.16) at the 3 different measurement times, respectively (Fig. 4b). As to the functional tests, the times in seconds for the TUG were 13.31 (SD 2.44), 10.10 (SD 2.22), and 10.70 (SD 2.46), respectively (Fig. 4c). The distance walked, in metres, in the 6MWT was 202.22 (SD 20.63), 217.37 (SD 24.65), and 208.35 (SD 24.80), respectively (Fig. 4d).
Fig. 4. Means and standard deviations of dependent variables for time 1 (before intervention), time 2 (after intervention) and time 3 (30 min after intervention) were depicted: (a) active range-of-motion for knee joint, (b) Relaxation Index of Pendulum test (graph bar without dots) and Modified Ashworth Scales for the hamstrings of bilateral lower extremity (graph bar with dots), (c) time in seconds for Timed Up and Go test, (d) distance in metres for 6-Minute Walk test. White bar: intervention in 0º/s, grey bar: 15º/s.
As for the variables that were not statistically significant, the AROM of the ankle joint before, after, and 30-min after the 15º/s intervention was 26.98º (SD 6.48º), 37.58º (SD 5.30º), and 37.67º (SD 5.46º), respectively (p = 0.421). The PROM of the knee joint before, after, and 30-min after the 15º/s intervention was 104.39º (SD 11.05º), 105.32º (SD 10.72º), and 103.69º (SD 11.23º), respectively (p = 0.108). The PROM of the ankle joint before, after, and 30-minutes after the 15º/s intervention was 48.82º (SD 7.11º), 48.76º (SD 4.69º), and 49.82º (SD 4.35º), respectively (p = 0.737). The results for each variable after 0º/s intervention are shown in Table I. None is statistically significant.
Moreover, correlation results revealed that the TUG was significantly correlated with the RI (r = –0.565, p < 0.05), but not significantly correlated with the MAS (r = 0.299, p = 0.261). The 6MWT correlated significantly only with the TUG (r = –0.597, p < 0.05), and not with the RI or MAS. As to the EMG signals, no concurrent changes in EMG activity were noted during the CPM intervention.
| Table I. Variables measured before (time 1), after (time 2), and 30-minutes after the intervention (time 3) of continuous passive motion device |
| | RI* Mean (SD) | MAS* Mean (SD) | TUG* Mean (SD) | 6MWT* Mean (SD) | AROM of the knee* Mean (SD) | AROM of the ankle Mean (SD) | PROM of the knee Mean (SD) | PROM of the ankle Mean (SD) |
| 15º/s | | | | | | | | |
| Time 1 | 0.59º (0.07º) | 4.69º (1.01º) | 13.31º (2.44º) | 202.22º (20.63º) | 93.08º (10.30º) | 26.98º (6.48º) | 104.39º (11.05º) | 48.82º (7.11º) |
| Time 2 | 0.72º (0.09º) | 3.31º (1.25º) | 10.10º (2.22º) | 217.37º (24.65º) | 98.71º (10.64º) | 37.58º (5.30º) | 105.32º (10.72º) | 48.76º (4.69º) |
| Time 3 | 0.68º (0.09º) | 3.50º (1.16º) | 10.70º (2.46º) | 208.35º (24.80º) | 97.41º (10.52º) | 37.67º (5.46º) | 103.69º (11.23º) | 49.82º (4.35º) |
| 0º/s | | | | | | | | |
| Time 1 | 0.59º (0.07º) | 4.88º (0.96º) | 13.49º (2.24º) | 202.34º (20.59º) | 94.08º (11.03º) | 26.98º (6.48º) | 104.20º (11.09º) | 48.82º (7.11º) |
| Time 2 | 0.60º (0.08º) | 4.69º (0.87º) | 13.10º (1.94º) | 200.58º (24.40º) | 93.97º (9.81º) | 27.65º (6.43º) | 104.21º (10.65º) | 48.53º (6.91º) |
| Time 3 | 0.61º (0.08º) | 4.75º (0.86º) | 12.10º (2.03º) | 200.69º (20.51º) | 93.37º (8.43º) | 27.19º (6.46º) | 104.05º (10.53º) | 48.70º (7.02º) |
| *Statistically significant difference in 15/s intervention (p < 0.05). RI: Relaxation Index; MAS: Modified Ashworth Scale; TUG: Timed Up and Go; 6MWT: 6-Minute Walk test; AROM: active range of motion; PROM: passive range of motion. |
DISCUSSION
The CPM device is a tool that may be valuable for use by children with CP in order to manage spastic hypertonia. The results of this study show that a 20-min CPM intervention to the knee joint decreased subjects’ spastic hypertonia, and improved their speed of walking. Typically, spastic hypertonia is assessed by measuring resistance to passive joint motion. Spastic hypertonia is believed to involve two mechanisms, with a reflexive and a mechanical component (7). According to Lance (13), the term spasticity is defined as “a motor disorder characterized by a velocity-dependent increase in tonic stretch reflexes”. It characterizes the reflexive part of spastic hypertonia, and can be measured via H-reflex or muscle EMG. Other than this reflexive contribution, the mechanical properties of the muscle, i.e. the passive viscoelastic elements of soft tissues and the biomechanical restraint from muscle or connective tissue, also contribute to the perceived resistance.
The MAS and the Pendulum test are commonly used clinical assessment tools to rate subjects’ spastic hypertonia. The results of this study indicate that, after CPM intervention, children with CP demonstrate a decrease in spastic hypertonia, as measured with MAS and RI. This decrease was seen immediately after the intervention, and lasted for 30 min after the intervention. Similar results were found by Krause et al. (14), who showed that the MAS and RI both improved after a 30-min passive cycling training in patients with spinal cord injury. Since no concurrent changes in EMG were noted during the CPM intervention, the primary contributor to the reduction in knee spastic hypertonia should be the changes in the mechanical components. This result is in agreement with those found for the ankle joint by Bressel & McNair (6). These researchers applied CPM to the ankle joint in stroke subjects, at an angular velocity of 5º/s. By measuring ankle joint stiffness, calculated from torque change divided by angle change, they found a decrease in ankle stiffness after CPM intervention. They claimed that the mechanical component was the primary contributor to stiffness reduction, since the EMG activities of the tibialis anterior and lateral gastrocnemius were less than 1% of the Maximum voluntary contraction.
Other research has shown that the mechanical component is not the only contributor to spastic hypertonia. Lindberg et al. (15) created a biomechanical model to measure spasticity, and found that the reflexive neural component dominated spastic behaviour in most patients. Clinically, Nuyens et al. (7) stated that, other than the decreased resistive torque after repeated passive movements of the knee, the EMG activity was obvious in the first movement repetition and faded thereafter. Since the EMG activities paralleled the variations in torque measurements, the authors stated that reflex activity had a role in the generation of increased resistance during passive movements.
In addition, Rosche et al. (16) reported that the mean F-wave amplitude, the mean F-wave/M-response ratio, and the maximum F-wave/M-response ratio were significantly lower after leg training with a motorized exercise-bicycle, documenting a decrease in the reflexive component of spasticity. Chang et al. (5) also applied CPM to individuals with spinal cord injury and found that the H-reflex amplitude decreased immediately after the intervention, but had mostly recovered 10 min later, while the MAS scores remained depressed. The results suggested that the contribution from the reflex component to decreasing spastic hypertonia could not be ruled out immediately after CPM.
Significant improvement was also noted in the AROM measurements for the knee joint immediately after and 30 min after the intervention. Although AROM correlated with spasticity at a significant level (17), none of the studies that used CPM to manage spastic lower extremities measured joint ROM (4–7, 14). Interestingly, by measuring AROM, the authors found significant increases after the intervention. Taylor et al. (18) developed an experimental model to evaluate the response of muscle tendon units to stretch. They concluded that cyclical stretching could increase flexibility and reduce tensile stress of the unit. AROM is defined as the joint movement through which a person can actively move using the adjacent muscles. Since spasticity can be triggered by voluntary movement (19), and spastic muscle properties can be affected by length changes in adjacent structures (20), a flexible and less-tense muscle tendon unit might be more efficient in muscle force transmission and therefore achieve a larger AROM. Further research is required into the link between CPM and its effect on joint AROM.
For PROM, no difference was seen before and after the intervention. This result is similar to that found in Cadenhead’s study (21), which indicated that a PROM exercise protocol did not have an effect on the lower extremity PROM measurements of the participants. Clinically, measurement of PROM is done by moving a joint passively to its extreme position. This movement is slow and should not elicit reflex activity. This indicated that the value of PROM cannot be interfered with the reflexive component of spastic hypertonia. Rather, the limitation in PROM originates mainly from mechanical constraints, such as the length of the musculature surrounding the joint, the flexibility of the joint capsule, and the contour of the bones. Since the CPM used in this study did not reach the end range of knee ROM, the authors conclude that it probably changed the viscoelastic elements of the muscles and nearby soft tissues, but did not impose any stretch effect on the joint capsule. This may explain why the PROM did not change significantly after the intervention.
In addition, subjects also showed better performance in functional evaluations, including TUG and 6MWT. Different from the Ashworth scale, the TUG and 6MWT assessed the velocity-dependent components of spastic function. Because spastic muscles exhibit velocity-dependent hypertonic reflexes, patients with measurable spasticity showed reduced knee angular velocity during walking and functional performance (22). In addition, passive stiffness is higher in spastic muscles, which leads to slower walking speed. In consequence, the spasticity of the knee affects gait efficacy in children with CP. Based on the results, the spasticity of the knee decreased after the CPM intervention. Adequate knee control during gait is important for a normal gait pattern. The analysis also revealed a moderate correlation (r = –0.565, p < 0.05) between TUG and Pendulum test RI. With less interference from spasticity, both reflexively and mechanically, subjects performed better in walking. Speed of walking was increased. However, since gait is a complex movement that requires coordination between joints of the lower extremities, spastic hypertonia over the ankle will also hinder a subject’s function. As such, further research is required to evaluate the effects of CPM on hypertonia in other joints, such as the ankle.
There are some limitations to this study. First, the results revealed that the decrease in spastic hypertonia persisted for up to 30 min after CPM intervention. This suggests that children with CP can benefit from this one-time intervention, in terms of both spastic hypertonia and ambulatory function. However, further investigation is required into how long this effect lasts in this population, and whether the device velocity and repetition values selected in this study lead to the best results. Furthermore, at this stage, CPM is an external device that is available to children with CP only in hospital or other clinical settings. It may be beneficial to design and develop a CPM device for daily use by patients at home.
References