Nuray Yozbatiran, PhD1, Jeffrey Berliner, DO,1 Marcia K. O’Malley, PhD2, Ali Utku Pehlivan, MSc2, Zahra Kadivar Z, PhD3, Corwin Boake, PhD1 and Gerard E. Francisco, MD1
From the 1University of Texas Health Science Center at Houston, Department of PM&R and UTHealth Motor Recovery Laboratory at TIRR Memorial Hermann, 2Department of Mechanical Engineering and Materials Science, Rice University and 3Department of PM&R, Baylor College of Medicine, Houston, USA
CASE REPORT: A 28-year-old woman, with incomplete spinal cord injury at the C2 level, classified as American Spinal Injury Impairment Scale C (AIS), participated in a robotic rehabilitation program 29 months after injury. Robotic training was provided to both upper extremities using the MAHI Exo-II, an exoskeleton device designed for rehabilitation of the upper limb, for 12 × 3-h sessions over 4 weeks. Training involved elbow flexion/extension, forearm supination/pronation, wrist flexion/extension, and radial/ulnar deviation.
RESULTS: Outcome measures were Action Research Arm Test, Jebsen-Taylor Hand Function Test, and AIS-upper extremity motor score. Safety measures included fatigue, pain and discomfort level using a 5-point rating scale. Following training, improvements were observed in the left arm and hand function, whereas the right arm and hand function showed no improvement in any of the functional outcome measures. No excessive pain, discomfort or fatigue was reported.
CONCLUSION: Data from one subject demonstrate valuable information on the feasibility, safety and effectiveness of robotic-assisted training of upper-extremity motor functions after incomplete spinal cord injury.
Key words: spinal cord injury; tetraplegia; arm and hand functions; robot-assisted; training.
J Rehabil Med 2012; 00: 00–00
Correspondence address: Nuray Yozbatiran, Department of PM&R and UTHealth Motor Recovery Lab at TIRR Memorial Hermann, University of Texas Health, Science Center at Houston, 77030 Houston, USA. E-mail: Nuray.Yozbatiran@uth.tmc.edu
Submitted July 26, 2011; accepted October 31, 2011
INTRODUCTION
In persons with tetraplegia, the residual strength of muscles affected by the injury is an important determinant of independence and function. Small improvements in upper-extremity strength can make a clinically significant difference in daily activities such as feeding and grooming. More than half of persons with tetraplegia indicated that regaining arm and hand function would most improve their quality of life (1).
Robotic training of the lower extremity has been studied extensively in the recovery of gait function after spinal cord injury (SCI) (2); however, only one publication by Krebs et al. (3) indicated upper extremity robotic training in incomplete cervical SCI and provided limited data on outcomes. This case report provides a robotic-assisted training protocol and demonstrates the feasibility and effectiveness of robotic training of elbow, forearm and wrist movement in persons with incomplete tetraplegia.
CASE REPORT
Subject
A 28-year-old woman, 29 months after an incomplete SCI at the C2 level, classified as American Spinal Injury Impairment Scale C (AIS), participated in this study. The subject had a Brown-Sequard Syndrome on initial presentation to acute rehabilitation. She gained strength acutely, but hit a nadir of recovery around the first year after injury in her upper extremity motor strength recovery. At the time of enrollment she presented with minimum voluntary movements (American Spinal Injury Association (ASIA) motor score 3) of her right upper extremity vs moderate voluntary movements on the left side (ASIA motor score 18). No pain was reported at baseline assessment. The subject signed the consent form approved by the local institutional review board.
Robotic rehabilitation device and training protocol
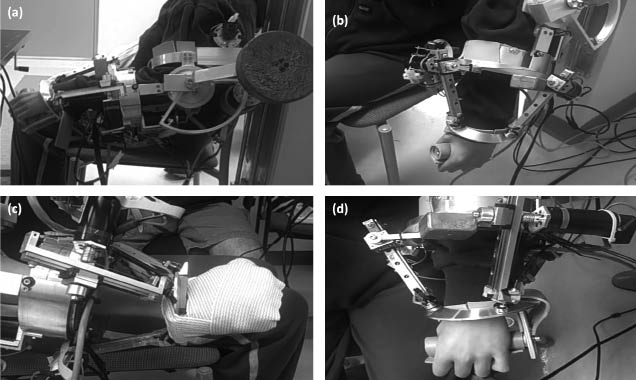
The MAHI Exo-II, a 5 degree-of-freedom robot, is an electrically actuated upper-extremity haptic exoskeleton device and has been designed for rehabilitation applications (4). Three therapeutic modes, described in detail by Guota et al. (5), enabled treatment to be tailored to the subject’s motor abilities: passive, triggered, and active-constrained. In the passive mode, the robot carried out the movement. In the triggered mode, the subject had to overcome a threshold resistance force before the robot took over and completed the movement. In the active-constraint mode, the subject executed movements against resistance (Fig. 1). The total time for each session, including set-up and frequent rest intervals, did not exceed 3 h. Actual training time for each side, as a proportion of the 3-h session, increased gradually over 4 weeks. The purpose of the single-joint exercises was to improve strength and active range of motion (ROM) of each joint.
Fig. 1. Training with the MAHI Exo-II exoskeleton. The subject is performing: (a) elbow flexion/extension; (b) forearm pronation/supination elbow extended; (c) wrist flexion/extension; (d) wrist radial/ulnar deviation.
Due to severe weakness of the right side, exercises were performed in the triggered mode for elbow flexion, wrist flexion/extension and wrist radial/ulnar deviation. Forearm pronation and supination were exercised in the passive mode.
Exercises on the left side were all performed in active-constrained mode. During training, a target-hitting task was displayed on the monitor and the subject was asked to move the pointer to hit the active target. After each movement, feedback was given as total number of hits. The treatment was progressed gradually, by increasing the number of repetitions, amount of resistance and amount of threshold force applied in the triggered mode. The patient received no additional therapeutic intervention for upper extremity training during the study period.
Outcome measures
Strength of selected muscles is scored according to upper extremity motor portion of the ASIA (range 0–25) (6). Arm and hand function performance were measured with the Jebsen-Taylor Hand Function Test (JTHFT) and the Action Research Arm Test (ARAT) (7, 8). A minimal clinically important difference (MCID) for ARAT has been set as 5.7 points (9). Fatigue, pain and discomfort after each training session was measured by asking 3 questions with expected response on a 5-point numeric scale (0 = strongly disagree, 1 = somewhat disagree, 2 = neither agree nor disagree, 3 = somewhat agree to, 4 = strongly agree; (a) this activity made me tired, (b) I was uncomfortable during this activity, and (c) I felt pain during this activity, respectively) (8).
RESULTS
After training, manual muscle test score of wrist extensor (C6) and finger flexor (C8) muscles increased from 1 to 2 on the right side and MMT score of finger abductor (T1) muscle increased from 2 to 3 on the left side. Positive improvements in functional outcome measures were observed for the left side only, while improvement reached a MCID for the ARAT (Table I and Fig. 1). The change in ARAT has exceeded the MCID of 5.7 points (Table I).
| Table I. Functional scores before and after robotic-assisted training |
| Task | Pre-treatment | Post-treatment |
| ASIA upper extremity motor score (0–25) Right Left | 7 18 | 9 19 |
| ARAT (0–57) Right Left | 3 41 | 3 49 |
| JTHFT (total time, s) Right Left | 1,080 151.64 | 1,080 80.4 |
| ASIA: American Spinal Injury Association; ARAT: Action Research Arm Test, JTHFT: Jebsen-Taylor Hand Function Test. The JTHFT was ended after 180 s. Lower times represent better performance. |
The subject’s self report on pain and discomfort level did not show any significant increase during therapy sessions (mean pain = 0.6, discomfort = 0.5). Level of fatigue showed an increase (mean fatigue = 3.8) after each session, but no therapy session was missed or had to be rescheduled because of the aforementioned symptoms.
DISCUSSION
This single case study demonstrates the preliminary results of a robotic training protocol for training of upper extremity movements after SCI. The results suggest that the MAHI Exo-II can be safely implemented in treatment of upper extremity motor function of a subject with incomplete tetraplegia. Positive gains in arm and hand functions were observed after 12 sessions of treatment on the left side with mild-moderate impairment level, whereas no detectable training effect was observed for the more severely impaired right upper extremity.
The current intervention used highly repeatable single-joint movements, focusing on elbow, forearm and wrist. The total number of active repetitive movements on the left side (elbow and wrist flexion/extension, forearm pronation/supination and wrist ulnar/radial deviation) increased from 87 to 800 repetitions. As described before, the treatment was gradually progressed by increasing the number of repetitions and resistance applied, so that at each session the subject was challenged to her maximal effort level. The specific factors that contributed most to the measured gains remain unclear; however, potential mechanisms may include activity-dependent neuroplastic changes, peripheral muscle strengthening, which might have caused a stronger tenodesis effect and improvement in muscle endurance.
Generalization has been demonstrated in similar studies with stroke patients using robotic assisted training as intervention (10). The gain from the repetitive training could be extended to overall arm function, as it was demonstrated with an improvement in hand functions measured with the JTHFT and ARAT. The improvement on left side ARAT score exceeded the MCID limit of 5.7 points.
Another key factor to consider in the current study was the safety of robotic training in subjects with SCI. Based on the findings of this pilot study, no adverse events were observed and use of the repetitive robotic exercises did not result in significant fatigue or discomfort as reported by the subject. This case report presents a rationale for performing larger controlled clinical studies to further evaluate the safety, feasibility and efficacy of using robotic-assisted training in patients with incomplete SCI in the future.
ACKNOWLEDGEMENT
We acknowledge the generous support of Mission Connect, a project of the TIRR Foundation.
REFERENCES