OBJECTIVE: To investigate the effect of a 10-week training programme on persons with a lower limb amputation and to determine if this training is sufficient to enable running.
SUBJECTS: Seven transtibial, 8 transfemoral and 1 bilateral amputee (all resulting from trauma, tumour or congenital) were randomly assigned to a training (n =8) or control group (n = 8).
METHODS: Isokinetic hip flexor and extensor strength at 60 and 120º/s and oxygen consumption while walking at 1.0 m/s were tested pre- and post- a 10-week period. The training group followed a twice weekly hip strengthening programme, while the control group continued with their usual activities. Running ability was determined pre-testing, and attempted after post-testing for the training group only.
RESULTS: The training group increased hip strength and decreased oxygen consumption. Six amputees who were previously unable to run were able to after training. The control group decreased intact limb hip extensor strength.
CONCLUSION: The training programme is sufficient to improve hip strength and enable running in persons with a lower limb amputation. As hip strength was reduced in those not following the training programme, it is recommended that strength training be undertaken regularly in order to avoid losing limb strength following amputation.
Key words: amputee; muscle strength; hip; running; training.
J Rehabil Med 2012; 00: 00–00
Correspondence address: Lee Nolan, Laboratory for Biomechanics and Motor Control, Department of Neuroscience, Karolinska Institutet and The Swedish School of Sport and Health Sciences, GIH, Stockholm, Sweden, Box 5626, SE-11486 Stockholm, Sweden. E-mail: lee.nolan@gih.se
Submitted February 25, 2011; accepted October 21, 2011
Introduction
Few healthy persons with a lower limb amputation who are otherwise able to exercise take up sport. The most common reasons for persons with a lower limb amputation not to participate in recreational activities are: an inability to run, an inability to jump, decreased speed of movement, and decreased endurance and fatigue (1). Whilst it is generally known that training or exercising improves muscle strength and speed, reduces fatigue and improves overall health, few people with a lower limb amputation feel that they know what exercises to do and many perceive themselves as too fatigued, slow or weak (1) to simply join in a training session or a sport.
Studies investigating strength in persons with a lower limb amputation have concluded that strengthening exercises for residual limb thigh muscles should be undertaken in order to return to an acceptable level of function following amputation (2–4). Furthermore, with the “correct training”, it is expected that the residual limb will have the same training response as the intact limb (3). However, which muscles, how and how often one should train in order to obtain the best effect has not been previously proposed or tested scientifically. Designing a training programme to target the specific muscles that compensate for the partial loss of a lower limb, but which are usually weak, should give sedentary persons the opportunity to be able more quickly to overcome the common reasons for lack of participation in recreational activities following amputation.
It is known that persons with a lower limb amputation compensate at the hip for the lack of a fully functioning knee and/or ankle joint during walking, running and jumping (5–8). It has been suggested that persons with a transtibial amputation (TTA) with better preserved thigh muscle strength have good walking capacity (9), and that weakness of residual hip muscles is a contributing factor in gait abnormalities for persons with a transfemoral amputation (TFA) (10, 11). In addition, a study reported hip extensor strength to be a strong predictor of performance in a 6-min walk test for persons with a lower limb amputation (12). Thus, theoretically, in this population hip strength is a major limiting factor in being able to walk well, run or jump.
The aim of this study was to investigate the effect of a 10-week training programme on hip strength in persons with a lower limb amputation. In addition, the study aims to test whether those who are unable to run prior to the training, are able to run afterwards. This test will determine whether the 10-week training programme is suitable to develop sufficient strength in order to enable running.
Methods
Subjects
Seven persons with transtibial amputations, 8 with transfemoral amputations and 1 with bilateral (1 limb transtibial, 1 limb transfemoral) amputation took part in the study. All participants had amputations resulting from trauma, tumour or congenital problems and were established walkers using their prosthesis daily (see Table I for individual details). The participants were initially contacted by a physiotherapist or prosthetist and those interested in volunteering were given further information about the study. Ethical approval was given by the Karolinska Institutet Regional Ethics committee and written informed consent was obtained from all participants.
All participants completed the same pre- and post-testing, with their post-test occurring 10 weeks after their pre-test. Prior to pre-testing, the participants were divided into two groups, as matched as possible based primarily on gender, amputation level and years as an amputee. One group (training group) went on to complete 10 weeks of the training programme described in this study, while the other group (control group) continued with the same form and amount of exercise they had been doing regularly for the past 3 months. This included walking, Nordic walking, swimming, aerobics, physiotherapy or no exercise at all (Table I). Mean age with standard deviation (SD), height, body mass and years as an amputee were 41.1 years (SD 8.4), 1.8 m (SD 0.12), 91.5 kg (SD 25.5), and 8.2 years (SD 9.2), respectively, for the training group, and 49.0 years (SD 9.1), 1.7 m (SD 0.08), 76.2 kg (SD 14.9), and 8.3 years (SD 11.3), respectively, for the control group.
| Table I. Subject characteristics |
| Gender/ ages, years | Amputation level | Weight (kg) | Height (m) | Years as amputee | Reason for amputation | Prosthesis (knee, foot) | Group | Exercise per week (sessions) | Exercise type |
| M/49 | TF | 113.0 | 1.94 | 1.5 | Trauma | Mauch, flex foot | Training | 0 | |
| M/35 | TF | 80.6 | 1.80 | 8.0 | Trauma | Black max II, flex foot | Training | 0 | |
| M/38 | TF | 66.0 | 1.80 | 1.0 | Tumour | Black max II, flex foot | Training | 0 | |
| F/28 | TT | 68.0 | 1.65 | 28.0 | Congenital | Black max II, flex foot | Training | 0 | |
| M/54 | TT | 68.0 | 1.67 | 13.0 | Trauma | Black max II, dynamic foot | Training | 7 | Sit-ups, push-ups |
| M/47 | TT | 133.5 | 1.97 | 2.5 | Trauma | Black max II, dynamic foot | Training | 1 | Physiotherapy |
| M/40 | TT | 112.8 | 1.91 | | Trauma | Black max II, dynamic foot | Training | 2 | Boxing, water aerobics |
| F/38 | BiLat | 90.0 | 1.73 | 10.0 | Trauma | Mauch, dynamic foot Mauch, dynamic foot | Training | 0 | |
| M/39 | TF | 76.5 | 1.78 | 15.0 | Trauma | Mauch, flex foot | Control | 0 | |
| M/53 | TF | 83.8 | 1.80 | 2.5 | Trauma | Mauch, flex foot | Control | 1 | Physiotherapy |
| M/55 | TF | 101.5 | 1.89 | 1.5 | Trauma | c-leg, dynamic foot | Control | 7 | Nordic walking |
| F/58 | TF | 67.0 | 1.68 | 3.0 | Trauma | Mauch, flex foot | Control | 0 | |
| F/49 | TF | 65.0 | 1.64 | 2.5 | Trauma | Mauch, flex foot | Control | 3 | Swimming |
| M/59 | TT | 60.0 | 1.70 | 34.0 | Trauma | Mauch, Flex foot | Control | 2 | Walking |
| F/45 | TT | 64.0 | 1.70 | 2.5 | Trauma | Mauch, Flex foot | Control | 2 | Gym (aerobics) |
| M/34 | TT | 91.5 | 1.69 | 5.0 | Trauma | Mauch, Flex foot | Control | 0 | |
| M: male; F: female; TF: transfemoral; TT: transtibial; BiLat: bilateral. |
Apparatus and procedure
All participants underwent hip strength, oxygen consumption and gait tests prior to and after the 10-week period. For the training group, post-tests were performed within two days of completing the training.
Strength. An isokinetic dynamometer (13), calibrated prior to each testing session, measured concentric hip flexor and extensor strength. The participant lay prone without their prosthesis. Their free limb and lower back was strapped down and the dynamometer adjusted so that the hip joint centre corresponded with the position of the axis of rotation of the lever arm. A custom made cuff was placed as distally as possible on the thigh of the limb being measured. This corresponded to just above the knee joint for those with a transtibial amputation, or, for those with a transfemoral amputation, as distally as possible along the residual limb without allowing the cuff to either slip off or cause pain or discomfort.
Initially, the participant was instructed to relax while the isokinetic dynamometer moved their limb at 60º/s through a range of 10º hip extension to 70º hip flexion. This was repeated until the subject felt comfortable with their position and the movement. The participant was then instructed to relax completely, and initial flexion and extension trials were collected to determine the torque due to gravity and the mass of the leg. A warm-up was then undertaken, consisting of flexing and extending the hip throughout the measuring range of motion with progressively more effort until the subject was close to maximal effort.
Hip strength in both limbs was then measured, intact limb first. Maximal concentric flexor and extensor strength measurements at 60º/s and 120º/s were performed in random order with verbal encouragement throughout the entire range of motion. Correct contraction speeds were ensured with a 5º ramp set, i.e. the dynamometer reached the selected speed during the initial 5º and slowed down to a stop during the last 5º of the range of motion. So as not to fatigue the subjects, two trials with a brief rest period of at least 60 seconds between, were allowed for each condition. Output angle (degrees) and torque data (Nm) were sampled at 100 Hz, using a Powerlab® data acquisition system (ADInstruments Ltd, Chalgrove, Oxfordshire, UK).
Oxygen consumption. Oxygen consumption was monitored using an Oxycon-Pro (Jaeger, Hoechberg, Germany). Participants wore a heart rate monitor (Polar Electro, Kempele, Finland) and were strapped into a harness suspended from the ceiling over a treadmill (Rodby, Vänge, Sweden). Familiarization of the test walking speed on the treadmill was then undertaken. Walking speed was gradually increased, with feedback from the participant at each increment in speed as to when they felt comfortable and balanced and did not have to use the sides of the treadmill for support. The target speed was 1.0 m/s. After the target speed was reached, the treadmill was stopped and a brief rest was allowed. The oxygen mask was then fitted and the test begun. Participants walked at 1.0 m/sfor approximately 5–6 min, or until they reached 4–5 min of steady state. All participants were able to complete the test.
Gait analysis. A ProReflex movement analysis system (Qualisys, Gothenburg, Sweden) and an AMTI force platform (AMTI, Watertown, MA, USA) were used to collect gait data pre- and post- the 10-week period whilst walking at 1.0 m/s for all participants. These data will not be presented in this study.
Running. During the pre-tests, all participants were asked if they could run with their prosthetic limb, and if they answered yes or did not know, were asked to demonstrate running overground. This applied to only one participant (a transtibial amputee in the training group) who stated that he had previously been able to run with a prosthetic limb. On demonstration, he was able to run leg-over-leg, but for less than 3 consecutive strides.
Running ability was monitored qualitatively for the training group after all post-testing. Those that wanted to attempt running (7 of the 8 participants) were strapped into a ceiling mounted safety harness over a treadmill (Rodby, Vänge, Sweden) and given brief instruction on leg-over-leg running technique, taken from Gailey (14). The harness was used in case of falls and was set up so that it did not in any way support the participant. The treadmill speed was increased steadily until the participant was forced to change from walking to slow jogging. After that, treadmill speed was increased or decreased depending on feedback from the participant. They were also allowed to stop and rest at any point and continue with this as long as they felt they were not too fatigued. If at any point the participant started to stumble, the treadmill was slowed then stopped and they were forced to take a break. Successful running was determined as continuous leg-over-leg running for at least 10 s on the treadmill at a speed faster than they could walk. All running was attempted with the participant’s everyday prosthesis set up for walking.
Training programme. Participants in the training group underwent 2 training sessions per week with at least 1 day rest in between for 10 weeks. All training sessions were led by an instructor. The training programme, designed to be able to be performed at home, consisted of a warm-up, balance and co-ordination exercises, hip strengthening exercises and a cool-down for each session. The warm-up consisted of 20 min easy, steady pace one-legged or bilateral cycling on a stationary bicycle. Balance and co-ordination exercises were performed for approximately 5–10 min and consisted of one of the following per session: balancing on an unstable surface, where balance difficulty was increased slightly every week, stepping over obstacles, sit-ups and push-ups, walking along a narrow line on the floor placing one foot in front of the other, walking through a series of small hoops placed flat on the floor with one footstep in each hoop until the end of the series, or standing on one leg and touching each of 3 separate markers on the floor with the other foot, then changing stance foot.
The hip strengthening exercises included “slow” hip flexion and extension and “fast” hip flexion and extension. All movements were performed with an ankle weight (Fig. 1) placed around the distal part of the thigh and all exercises were performed with the prosthesis on.
Hip flexion movements were performed with the participant holding onto a support while standing on one leg, flexing the free hip and raising their thigh until it was parallel with the ground, then lowering. Hip extension movements were performed with the participant holding onto a support while standing on one leg, extending their free hip and lifting their leg backwards as high as possible without rotating the pelvis, then lowering. If a participant could not weight-bear on their prosthetic limb, they could either sit on a suitably high surface for the hip flexion movements or lean over a suitably high surface for the hip extension movements. However, they were encouraged to progress to being able to weight-bear on their prosthetic leg with only slight support.
Fig. 1. Ankle weights used for hip strength training. To increase weight, either multiple ankle weights were used, or a dumbbell was fastened to the “ankle” weight using Velcro.
For the “slow” movements, participants were instructed to choose as heavy a weight that they could lift 10 times in succession. For the “fast” movements, participants were instructed to choose a lighter weight and perform 15 repetitions (reps) as fast as possible. For the first 2 weeks, participants performed 2 × 10 reps for “slow” flexion and extension on both legs, and 2 × 15 reps for the “fast” flexion and extension on both legs. From week 3, they increased to 3 × 10 reps for the “slow” movements and 3 × 15 reps for the “fast” movements.
All participants recorded how many kilograms they had used to remind them of what weight to start with in their next session. Weight, starting at around 1–1.5 kg, was not increased in the first week, was slowly increased in the next 2 weeks, and after that was increased depending on how the participants felt. This was done by either adding more or heavier ankle weights, or by attaching a dumbbell to the ankle weight. All participants managed to train with 8–9 kg by the end of the 10 weeks. Some managed more. An instructor monitored the movements to make sure they were being performed correctly. Verbal encouragement was also given.
Stretching was then performed prior to cool-down. For cool-down, participants walked for approximately 5–10 min.
Data analysis
Strength. For each condition (flexion, extension, 60º/s, 120º/s), the greatest peak torque of the 2 strength trials obtained was chosen for further analysis. The gravity torque was then subtracted from, or added to, the flexion and extension trials, respectively. The initial and final 5º of motion were removed, resulting in a range of motion of 5º hip extension to 65º hip flexion to ensure contraction speed was constant throughout the trial. In addition to flexion and extension peak torque, flexion and extension mean torques over the analysed range of motion were calculated. Torques were normalised to the body mass of each individual.
A flexion extension strength ratio (peak flexion torque/peak extension torque) was calculated for the intact and residual limbs at each speed in order to determine the relative strength of the hip flexors to the hip extensors.
An asymmetry index (ASI): where ASI = (L–R)/0.5 × (L+R) × 00 (15)was used to indicate peak and mean torque differences between the intact (R) and residual (L) limbs of the unilateral amputees. Here, higher values indicate greater asymmetry.
Oxygen consumption. Data files were exported from the Oxycon Pro (Jaeger, Hoechberg, Germany) and the analysis performed in Excel. For each subject, the VO2 values from 4 min of the test where the participant had reached steady state were averaged and normalised to body mass.
Statistical analysis
Data were checked for normality. For the strength tests, due to the purpose of comparing intact with residual limb, the bilateral amputee’s data were removed from the training group and presented separately. A Mann-Whitney U test was used to compare the groups at pre-test, and at post-test for all calculated variables. A Wilcoxon test was used to determine any differences between the pre- and post-tests for the intact and residual limb for normalised strength in each group.
If a group underwent a significant change in body mass between pre- and post-testing, non-normalised absolute hip strength was also reported for that group. A Wilcoxon test was performed on intact and residual limb non-normalised hip strength values to determine any differences between pre-and post-testing that were not dependent on body mass changes.
Non-normalised absolute values were tested within-group only to determine the change of body mass on the results. Absolute values were not tested between-group, as normalizing to body mass is an effective method of removing body size dependence, removing unwanted anthropometric variables and allowing comparisons between different populations (16).
An independent t-test was used to compare groups at pre-testing, and at post-testing in order to establish whether there were initial differences in oxygen consumption. If a group underwent a significant change in body mass between pre- and post-testing, non-normalised oxygen consumption values were also tested for that group. Paired t-tests were performed for each group between the pre- and post-tests for oxygen consumption. The alpha level was set at 5%.
Results
There were no significant differences between the training and control groups for height, mass, age, years as an amputee, strength or oxygen consumption at pre-testing.
The training group significantly reduced body mass post-training, whereas the control group did not. However, there was no significant difference for body mass between the two groups at post-training.
Strength
The mean strength results were statistically similar to the peak strength results. Therefore, peak strength variables only are presented.
Training group (normalised hip strength) without bilateral amputee
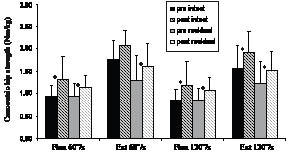
For the intact limb, all flexor and extensor strength variables with the exception of the intact limb peak extensor strength at 60º/s, increased significantly post-training. For the residual limb, all strength variables increased significantly (Fig. 2).
Fig. 2. Mean and standard deviation of peak concentric hip strength for the training group without the bilateral amputee. *Significant difference pre- vs post-testing.
No significant changes were seen in the training group for the flexor/extensor ratio for either the intact or residual limbs post training (Table II).
| Table II. Peak flexor/extensor ratio |
| Variables | 60º/s | 120º/s |
| Pre-testing Mean (SD) | Post-testing Mean (SD) | Pre-testing Mean (SD) | Post-testing Mean (SD) |
| Training group, without bilateral amputee |
| Intact limb | 0.54 (0.10) | 0.62 (0.14) | 0.57 (0.11) | 0.60 (0.14) |
| Residual limb | 0.80 (0.34) | 0.74 (0.19) | 0.73 (0.20) | 0.74 (0.22) |
| Bilateral amputee | | | | |
| TT limb | 0.55 | 0.78 | 0.40 | 0.67 |
| TF limb | 1.06 | 1.01 | 0.75 | 0.78 |
| Control group | | | | |
| Intact limb | 0.63 (0.17) | 0.95 (0.28)* | 0.79 (0.26) | 0.86 (0.19) |
| Residual limb | 0.75 | 0.73 | 0.75 | 0.67 |
| | (0.25) | (0.18) | (0.25) | (0.21) |
| *Significant difference pre- vs post- testing. TT: transtibial; TF: transfemoral. |
Peak extensor strength asymmetry reduced after training at both 60º/s and 120º/s for the training group (Table III).
Training group (non-normalised hip strength) without bilateral amputee
As the training group reduced body mass post-training, non-normalised strength values were also statistically tested for this group. For the intact limb, all flexor and extensor strength variables, with the exception of intact limb peak extensor strength at 60º/s, increased significantly post-training. For the residual limb, all strength variables increased significantly.
Training (bilateral amputee)
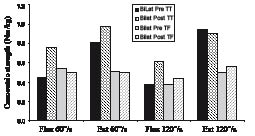
The bilateral amputee appeared to exhibit strength differences between her transtibial and transfemoral limbs. Initially, her transfemoral limb hip flexors were stronger than her transtibial limb hip flexors at 60º/s, and similarly at 120º/ss. Post-testing, her transtibial limb hip flexors appeared to be stronger than transfemoral limb flexors at both speeds (Fig. 3). Hip extensor strength, however, appeared to be greater in her transtibial limb than transfemoral limb at pre-testing and continued to be so at post-testing (Fig. 3). An increase in transtibial limb strength was seen mainly at 60º/s, while an increase in transfemoral limb strength was seen mainly at 120º/s.
Fig. 3. Peak concentric hip strength for the bilateral amputee. Bilat. bilateral; TT: transtibial; TF: transfemoral.
The bilateral amputee increased her flexion/extension ratio post-training at both contraction speeds for her transtibial limb. Thus her hip flexors became stronger relative to her extensors, post-testing. There was very little change for her transfemoral limb. She also increased strength asymmetry in all but extensor strength at 120º/s. This was seen as an increase in her transtibial relative to transfemoral limb strength.
Control group (normalised hip strength)
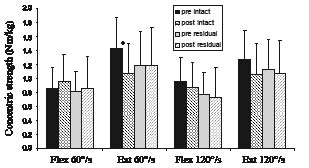
There was no significant increase in strength in either limb for the control group. However, intact limb peak extensor strength at 60º/s significantly reduced between pre- and post-testing (Fig. 4).
Fig. 4. Mean and standard deviation of peak concentric hip strength for the control group. *Significant difference pre- vs post-testing.
As a consequence of the loss of intact limb extensor strength, the peak flexor/extensor ratio at 60º/s increased significantly (Table II). Thus, intact limb hip flexor and extensor strength were now similar. No significant changes in strength asymmetry were seen (Table III).Training vs control group strength (normalised) at post-testing
| Table III. Asymmetry index (ASI) |
| | 60º/s | 120º/s |
| Flexion | Extension | Flexion | Extension |
| Pre-testing Mean (SD) | Post-testing Mean (SD) | Pre-testing Mean (SD) | Post-testing Mean (SD) | Pre-testing Mean (SD) | Post-testing Mean (SD) | Pre-testing Mean (SD) | Post-testing Mean (SD) |
| Training group | 37.5 | 30.5 | 46.4 | 30.3* | 36.7 | 35.3 | 45.1 | 32.5* |
| (%) without bilateral amputee | (20.9) | (19.3) | (38.5) | (27.6) | (23.5) | (18.7) | (27.9) | (30.4) |
| Bilateral amputee | 19.3 | 40.2 | 41.7 | 64.4 | 1.5 | 33.5 | 61.6 | 47.6 |
| Control group | 25.9 | 31.6 | 25.8 | 28.8 | 33.6 | 40.7 | 24.3 | 22.4 |
| (%) | (23.2) | (23.3) | (32.5) | (27.9) | (22.5) | (35.0) | (21.8) | (24.8) |
| *Significant difference pre- vs post-testing. |
Whilst the training group were seen to exhibit greater hip strength compared with the control group at post-testing, not all differences were found to be statistically significant. The training group had significantly stronger intact limb hip extensor strength at both speeds post-testing than the control group. They also exhibited significantly greater residual limb hip flexor and extensor strength at 120º/second compared with the control group.
Oxygen consumption (normalised)
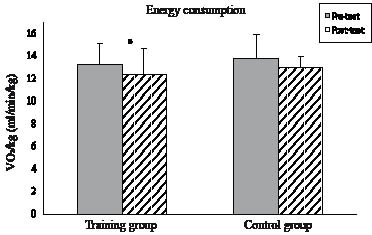
The training group significantly reduced their oxygen consumption after training whilst the control group exhibited no significant change (Fig. 5). There was, however, no significant difference between the groups at post-testing.
Fig. 5. Mean and standard deviation of oxygen consumption during walking at 1.0 m/s for the training and control groups. *Significant difference pre- vs post-testing.
Oxygen consumption (non-normalised)
As the training group reduced body mass post-training, non-normalised oxygen consumption values were also statistically tested for this group. The training group significantly reduced their non-normalised oxygen consumption values post-training, while no change was seen for the control group.
Running
From the training group participants, one transtibial amputee had been able to run in the past and was able to run again during week 3 of the training programme. A further 2 transtibial amputees who stated they had never run before, began running in weeks 7 and 8 of the training programme, respectively. These 3 individuals all tried by themselves without encouragement, whenever they felt ready or able to run, and ran overground. The remaining transtibial amputee attempted to run for the first time after the post-testing in the more controlled running environment on the treadmill with a safety harness. However, after 2 brief attempts, he decided not to continue. He was unable to run for 10 s continuously on the treadmill and stated that he “felt unsure” or was a little afraid to push himself.
None of the 3 transfemoral amputees had been able to run previously. All stated that either they had felt they had not been able to run during the training programme, or they had not tried. They all stated that they did not think it would be possible for them to run but were willing to try on the treadmill with the safety harness. After brief instruction on the treadmill and 1–2 brief rests, all were able to run leg-over-leg for at least 20 s. Additionally, all 3 transfemoral amputees stated that after the 10 weeks training they now had a better “fit” of their socket as they felt they were able to tense their residual limb muscles and “grip” inside the socket. This, they stated, felt as though it particularly improved their gait during the swing phase, which made it feel easier to walk. The bilateral amputee chose not to attempt running.
Discussion
The results showed that the 10-week training programme that can be undertaken at home was sufficient to increase concentric hip flexor and extensor strength, reduce sub-maximal oxygen consumption and enable running in persons with a lower limb amputation. Additionally, a 10-week period of occasional light activity, such as walking, swimming, physiotherapy, or aerobics instead of strength training, resulted in a decrease in hip extensor strength in persons with a lower limb amputation.
As was to be expected, several strength measurements improved for the training group, while no strength measurements improved for the control group. All participants in the present study exhibited pre-test hip flexor strengths similar to that previously reported for sedentary persons with TTA (17). In the training group, hip flexor strength significantly improved for both the intact and residual limbs at both contraction speeds, and this was found to be true for absolute strength and not just dependent on body mass changes. Low isometric hip flexor strength previously found in sedentary persons with TTA was suggested to be due to the hip flexors naturally being less exercised than the hip extensors, which function as antigravity muscles. In addition, an inability to run or walk quickly would be expected to be a result of inadequate training of these hip flexors (18). While the training group exhibited similar intact limb hip flexor strength at post-testing to physically active persons with TTA (17), residual limb hip flexor strength was lower. Thus, while hip flexor strength increased in both limbs, 10 weeks of training is not sufficient to reach the residual limb strength values reported in highly active persons with a lower limb amputation, but does appear to be sufficient to start to learn to run.
Despite an overall improvement in hip flexion strength, the training group’s hip flexion asymmetry did not significantly change, remaining around 30–35%, with the residual limb the weakest. This is high compared with a previous study on physically active persons with a lower limb amputation (17) who exhibited 8% hip flexion strength asymmetry with their residual limb the strongest. However, as the training group had just begun to exercise and run it is not yet known how much stronger, particularly in their residual limb, or symmetrical they might have become had they continued.
Hip extensor strength in the training group significantly improved for all measurements except intact limb extensor strength at 60º/s, where a small but non-significant improvement in strength was seen. These findings were the same regardless of normalizing to body mass or not. While pre-test hip extensor values are comparable with that previously reported for sedentary persons with a lower limb amputation (17), the training group’s post-test hip extensor strength was weaker (1.6–2.1 Nm/kg) than that previously reported for physically active persons with TTA (2.4–2.7 Nm/kg) (17). Again, it is not known whether the training group’s hip extensor strength would have continued to increase had they continued to train after the 10-week period, but their asymmetry results indicate their extensor strength increased more on their residual than intact limb. This was seen as a decrease after training from over 45% to just over 30%. It is still high compared with the 14% asymmetry reported by Nolan (17), where the residual limb was stronger than the intact limb. Moirenfeld et al. (3) stated that, from a metabolic point of view, the muscles in the residual limb function properly and one may expect to gain as significant reaction from training those muscles as one would from training the intact limb muscles. As it is expected that athletes with a lower limb amputation competing in sport at the highest level have stronger limbs than those in the present study, it is suggested that continued training would further increase hip strength. However, it is not yet known whether further training would reduce or increase limb strength asymmetry, and further study is warranted.
Interestingly, intact limb hip extensor was the only strength variable that significantly changed for the control group, reducing strength over the 10-week period and consequently increasing the hip flexor/extensor ratio. This variable was also significantly different between the two groups at post-testing. Other reductions in hip strength were exhibited by the control group, but were not significant. The results of the present study therefore show that it is important also to target the intact limb in any strength training programme and is in agreement with a previous study that showed that strength deteriorates following lower limb amputation (19). However, in another study where no strength differences were found between those who were amputated several years ago compared with those who were amputated more recently (2), it was not clear how active the participants had been. In the present study, several participants in the control group regularly exercised in terms of walking, Nordic walking, swimming, aerobics or undergoing weekly physiotherapy. Thus it may be possible that these types of healthy activities alone are insufficient to retain limb strength in persons with a lower limb amputation. It should therefore be recommended that a strength improving programme be undertaken in addition to these types of activities for persons with a lower limb amputation to avoid further loss of limb strength.
On looking at the strength results of the individual with a bilateral amputation, it is interesting to note that, initially, her hip flexors were stronger in her transtibial than transfemoral limb, while her hip extensors were strongest in her transtibial limb. Post-training, it was mainly her hip flexors that increased in strength, resulting in increased asymmetry between the limbs. As this was the only bilateral amputee in the training group, conclusions cannot be drawn as to the effect of the 10-week training programme and whether it is beneficial or needs to be modified for bilateral amputees. Further research is needed specifically on the effect of limb strengthening programmes on persons with bilateral amputations.
Although the aim of this training programme was not specifically to improve oxygen consumption, it significantly reduced in the training group, but no significant differences were seen between groups at post-testing. It is not known whether further training with this type of training programme not specifically aimed at improving oxygen consumption would result in group differences. The differences seen within the training group could have been caused by the fact that most of the participants in the training group lost weight, rather than by any improvement in cardiovascular function. However, on re-running the statistical analysis with non-normalised values, the same significant results were noted.
Possible reasons for this reduction in oxygen consumption could have been the 20 min of warm-up low intensity cycling twice a week, the strength training itself, or that the increase in muscle strength altered gait mechanics, making gait more efficient. However, studies have reported no change in sub-maximal VO2 while walking at 1.0 m/s after 12 weeks’ cycling and walking training in persons with TFA (10), or while walking at 0.9 m/s after 16 weeks’ whole body strength training in older females (20).
Whilst gait data were collected pre- and post-testing, these results will be presented elsewhere. It is interesting though to note a comment made by all 3 transfemoral amputees in the training group after they attempted running, that they felt able to “tense” their residual limb muscles and “grip” the inside of the socket, making it easier to walk, particularly during the swing phase. Further research is needed to determine whether the strength training can cause a change in amputee gait mechanics.
It is not known if or how the balance part of the training programme affected ability to run. While studies have looked at the effects of rehabilitation on standing balance in lower limb amputees and found that balance can be improved somewhat (21, 22), none have looked at the effect of balance on the ability of persons with lower limb amputations to run. Further research in this area is thus warranted. On another note, the significant increase in residual limb hip flexor and extensor strength at 120º/s in the training group, which was found to be significantly greater than for the control group at post-testing, may have contributed to the ability to run. Thus it is advisable that not only slow strength training repetitions, but also fast repetitions are undertaken if the goal is to run.
The limitations of the study include group size and matching. Matching the two groups in terms of gender, amputation level and years as an amputee as far as possible resulted in the control group having a greater activity level than the training group prior to testing. However, the control group tended to reduce strength over the 10 weeks, thus it does not appear that their “usual” exercise of walking, swimming and physiotherapy affected the results. On the contrary, had the control group not exercised at all during the 10-week period, group differences at post-testing may have been greater.
As the training programme included not only strength training, but also balance and co-ordination exercises, it is not known whether strength training alone achieved the results reported in the present study, or if balance exercises are also necessary. Studies have shown that balance is compromised following lower limb amputation, and while it can be improved with training, has not been shown to improve to levels comparable with non-amputees (21, 22). More research is needed on the effect of the type of training undertaken in the present study on balance.
In conclusion, the results of this study show that training twice a week for 10 weeks is sufficient to significantly improve hip strength in lower limb amputees. For those that did not follow the training programme but continued with their everyday activities, 10 weeks was sufficient time to significantly reduce hip extensor strength. It is recommended that a limb strengthening programme that targets both the residual and intact limbs be followed by lower limb amputees regularly in order to avoid losing limb strength following amputation. In addition, several participants in the training group were able to run for the first time following completion of the training programme. It is not known whether the strength exercises alone helped them achieve that, or whether the balance exercises were also necessary. Therefore it is recommended that further research investigate the role of balance on running ability in persons with a lower limb amputation.
Acknowledgements
The author would like to thank Oscar Gidewall for help with the training sessions and Alexander Ovendahl and Mårten Fredriksson for help with data collection. The study received financial support from Allmäna arvsfonden, CIF (Centre for Sport Research, Stockholm) and GIH, Stockholm.
References