OBJECTIVE: To examine changes in mobility longitudinally following single-event multilevel surgery in ambulant children with cerebral palsy, focusing on those using assistive devices for functional mobility because they are most at risk of declining gross motor function.
PARTICIPANTS: A consecutive sample of 156 ambulant children with cerebral palsy (99 males), 96 without devices (Gross Motor Function Classification System (GMFCS) I/II), 60 with devices (GMFCS III) who had single-event multilevel surgery at mean age 11 years 1 month.
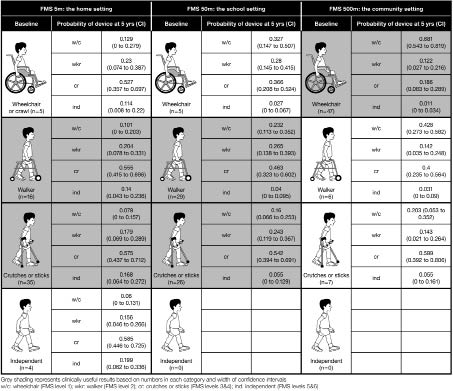
METHODS: GMFCS and Functional Mobility Scale (FMS) ratings were recorded pre-operatively and at 2 and 5 years post-operatively. A proportional odds logistic regression model was used for the GMFCS III group to predict the probability of assistive device requirements post-operatively conditional on baseline FMS.
RESULTS: Children in GMFCS III showed more change than those in I/II at home and school. Those in GMFCS III using crutches pre-operatively at home and school were more likely to continue using them at 5 years, whereas those using walkers were more likely to change to crutches or wheelchairs. Wheelchairs were most commonly used in the community before and after single-event multilevel surgery.
CONCLUSION: Mobility was generally stable or improved at 5 years after single-event multilevel surgery; however, a small number of children used more assistance to facilitate mobility.
Key words: cerebral palsy; mobility; outcomes assessment; activity; multilevel surgery.
J Rehabil Med 2012; 44: 137–143
Correspondence address: Adrienne Harvey, 35/17 Yarra Street Hawthorn 3122, Victoria, Australia. E-mail: harvey.adrienne@gmail.com
Submitted March 21, 2011; accepted October 10, 2011
Introduction
Single-event multilevel surgery (SEMLS) is considered to be the standard of care to improve gait and functioning in ambulant children with cerebral palsy (CP) and refers to the correction of all musculoskeletal deformities producing gait deviations in one session (1). SEMLS is a complex orthopaedic surgical intervention using a combination of muscle tendon lengthenings, tendon transfers, rotational osteotomies and joint stabilization procedures (2). It is usually based on detailed biomechanical assessment and is typically performed during childhood in ambulant children, primarily those in Gross Motor Function Classification System (GMFCS) (3) levels I–III. For optimum benefits, SEMLS must be combined with an intensive post-operative rehabilitation programme, and outcomes are usually assessed with a combination of instrumented gait analysis, functional scales and patient-reported outcomes (4).
Interventions such as SEMLS for children with CP aim to produce changes in body functions and structures, with the expectation that this will result in positive effects on activity and participation, as described by the International Classification of Functioning, Disability and Health (ICF) (5). There is also an expectation that corrections obtained in childhood are maintained throughout adolescence and into adulthood. However, the longer term impact of SEMLS on activity and participation has not been examined adequately.
Longitudinal data describing changes in gross motor function as children with CP enter adulthood, illustrated by motor growth curves, show maintenance of functional levels for those who ambulate without assistive devices (GMFCS levels I and II), but a functional decline for those who require assistance to ambulate or are non-ambulant (GMFCS III–V) as they become young adults (6). Moreover, gait parameters of children with CP have been shown to deteriorate over time without interventions (7, 8). Many adults with CP report declining mobility and gait function, often related to pain, fatigue, weakness and balance issues (9–12). Shorter-term surgical studies have shown stabilization of gait patterns following SEMLS, with deterioration of control groups of children with CP (13, 14). These studies show a general deterioration of mobility over time without interventions; thus maintenance of mobility levels might be an appropriate long-term goal of SEMLS and one that needs to be explored.
Optimal mobility allows adolescents to maximize their participation in daily life, particularly as they enter adulthood. For this reason it is important to examine functional mobility in a longitudinal fashion following such major interventions as SEMLS, which are typically performed in the younger child. There are no studies published to date reporting functional mobility longitudinally following SEMLS. Many studies report outcomes up to two years post-surgery, usually focusing on body functions and structure using gait analysis and measures derived from physical examination (13–16). Longer follow-up studies also focus on body functions and structure (17–19). Until recently, most studies evaluating SEMLS were retrospective or prospective cohort studies, with few controlled trials. A recent randomized controlled trial of 19 children with CP, GMFCS levels II–III, randomized into SEMLS or progressive resistance strength training, showed a 57% improvement in a global gait summary statistic (Gillette Gait Index) for the surgical group at 12 months post-operatively, whereas a small deterioration was observed in the control group (4). Functional improvements (mobility and gross motor function) were seen at two years post-operatively. Limitations of this trial include the small number of children recruited and the follow-up restricted to two years.
There remains a deficit of evidence of long-term effects of SEMLS on functional mobility. The mobility of children with CP was found to deteriorate in the first 6 months following SEMLS, with subsequent improvement to pre-operative levels at 12 months, and further improvement in the second post-operative year (20). Mobility status beyond this time is largely unknown.
This purpose of this study is to report the effects of SEMLS on functional mobility in a large group of children and adolescents with CP, in a prospective longitudinal manner with a mean post-intervention follow-up of 5 years. The study focuses on children in GMFCS level III because they are more at risk of declining gross motor function and have more diverse mobility methods.
The research questions were:
• What changes in mobility are seen in children in GMFCS levels I–III at 5 years post-SEMLS; and
• For children in GMFCS level III, what is the probability of change in assistive device requirements for mobility at 5 years post-operatively based on pre-operative status?
We hypothesized that children in GMFCS levels I/II at baseline would show less change in assistance, while the probabilities of change for those in level III would vary depending on their pre-operative mobility requirements.
Methods
This longitudinal study involved retrospective analysis of prospectively collected clinical data on a consecutive sample of children with CP at the Hugh Williamson Gait Laboratory of the Royal Children’s Hospital, Melbourne, Australia. Experienced senior physiotherapists prospectively gathered standardized physical examination parameters, gait and functional data. Parents had given informed consent and the study was approved by the Ethics in Human Research Department of the tertiary care centre from where the children were recruited.
Participants
The participants were all children and adolescents with spastic CP who underwent SEMLS at a single tertiary children’s hospital between 1998 and 2006. The individual child’s precise surgical prescription was determined by a full biomechanical evaluation, including a standardized physical examination, measurements of muscle tone, strength and muscle selectivity and instrumented gait analysis (21). Multilevel surgery prescription included soft tissue procedures, such as tendon lengthenings, tendon transfers and muscle recessions. Bony procedures included rotational osteotomies and stabilization of the hip and/or midfoot when indicated, following previously published guidelines (1). Surgery was performed by two staff surgeons, plus two senior assistants operating as a team. Our approach to selection of surgical procedures and postoperative rehabilitation has been reported in a number of publications (1, 4) and is not the focus of this study, which is concerned with longitudinal assessments of functional mobility. Children were excluded from this study if clinical monitoring and follow-up had not been done with return visits to the Gait Laboratory, or if follow-up was shorter than two years from surgery.
Procedure
The first author, an experienced clinical researcher, collected the data from the gait laboratory files. Baseline information included: child’s motor disorder type and topographical pattern, age at surgery, GMFCS level (3) and mobility rating using the Functional Mobility Scale (FMS) (22). At a mean of 2 and 5 years post-operatively, the information retrieved was the child’s age, GMFCS level and FMS rating.
Instruments
The GMFCS is a 5-level ordinal grading system for children with CP based on the assessment of self-initiated movement, with emphasis on function in sitting and walking (3). The GMFCS is reliable, valid and stable over time (3, 23) and is used widely to describe and classify children based on activity.
The FMS is a 6-point ordinal scale that rates the mobility of children with CP based on the need for assistive devices at 3 specific distances: 5, 50 and 500 m. These represent home, school and community environments, respectively (22). The FMS is administered by asking a few questions of the child and/or parent. It has been shown to be reliable, valid and able to detect change after SEMLS (20, 22, 24).
Together the GMFCS and FMS provide clear and complementary descriptions of a child’s mobility status: GMFCS classifies and FMS measures change over time (25).
Statistics
Descriptive statistics were calculated for the group at each time point, including mean age, GMFCS level distribution and FMS scores. Stability of GMFCS levels from baseline (pre-operatively) to each time point was analysed using quadratic weighted kappas (26).
Children in GMFCS levels I and II were combined because both groups walk independently without assistive devices. Children in level III use a range of assistive devices, including sticks, crutches and walkers. The percentage of children who changed 1, 2 or 3 FMS categories in either direction was calculated for those in GMFCS I/II compared with those in level III for each FMS distance.
For children in GMFCS level III at baseline a proportional odds logistic regression model was used to predict the probability of FMS-reported assistive device requirements at 2 and 5 years post-operatively. In this model, the probability of various FMS level thresholds at each time point was conditioned on FMS levels at the previous time point through a logit function. FMS scores 3 and 4 were combined (walk with crutches or sticks) as were 5 and 6 (walk without devices). FMS categories 1 (wheelchair) and 2 (walker) remained as separate scores. The model was developed in Mplus 5.2 using the maximum likelihood estimator, and Monte Carlo method of integration (27). The estimated coefficients of the model were used to calculate estimated probabilities for each FMS category, conditional on the category at the previous time.
Results
There were 156 children (99 males) in the study; 96 in GMFCS level I/II combined and 60 in level III. Mean age at surgery overall was 11.1 years (standard deviation (SD) 2.47, range 6–19 years). The mean number of surgical procedures per SEMLS intervention was 7.6 (SD 2.1). The majority of children had both bony and soft tissue procedures (144), with only 12 children having soft tissue surgery with no bony procedures.
Substantial agreement was found for GMFCS levels at different time points (kw 0.70–0.76, percentage agreement 96–97%) providing evidence of stability over time. There were 96 children in GMFCS level I/II preoperatively (62%), and 60 (38%) in level III. At 5 years 68 children (58%) were in I/II, 45 (38%) in III and 4 children (3%) in level IV. On closer inspection, the children who were later classified in level IV were on the margins between III and IV pre-operatively; that is, they had more severe motor impairments, and during adolescence chose wheelchair use for energy conservation and independence.
Table I displays the percentages of children in GMFCS level I/II at baseline who changed FMS levels compared with those in III. Change upwards represents less assistance required and change downwards represents more assistance required. More change was seen for children in III compared with those originally in I/II for FMS 5 and 50 m. For 500 m both groups showed equal change. The majority of change reflected less assistance required. Descriptive data for children who were 12 years or younger at the time of surgery were compared with those who were older than 12 at the time of surgery. The only striking differences found were at the 5 m and 500 m distances, where a greater number of children in the older group required less assistance at 5 years compared with pre-operatively.
| Table I. Changed Functional Mobility Scale (FMS) scores (1 or more levels) at 5 years post-single-event multilevel surgery: comparison of children in Gross Motor Function Classification System (GMFCS) level III with those in level I/II pre-operatively |
| | GMFCS I/II n (%) | GMFCS III n (%) |
| FMS 5 m | No change | 56 (74) | 11 (33) |
| | Change up | 14 (18) | 22 (51) |
| | Change down | 6 (8) | 5 (16) |
| FMS 50 m | No change | 50 (66) | 19 (51) |
| | Change up | 15 (20) | 13 (34) |
| | Change down | 11 (14) | 6 (15) |
| FMS 500 m | No change | 45 (60) | 23 (60) |
| | Change up | 18 (24) | 11 (30) |
| | Change down | 12 (16) | 4 (10) |
| Change-up: requires less assistance; -down: requires more assistance. |
Results of the longitudinal modelling for those in GMFCS III at baseline are shown in Fig. 1 for each FMS distance. No children walked independently of assistive devices at 50 and 500 metres pre-operatively; hence, there are no data for these categories.
Pre-operatively in the home setting the majority of children in GMFCS III used crutches or sticks (58%) followed by walkers (27%). In the school setting, a walker was the most common method pre-operatively (48%) followed by crutches or sticks (43%). In the community, wheelchair use was most common (78%).
Fig. 1. Probability of change in assistive device at 5 years post-operatively conditioned on baseline requirements for Functional Mobility Scale (FMS) 5, 50 and 500 m. (Shaded areas denote the most clinically significant results based on the numbers in each category and the width of the confidence intervals (CI)). w/c:wheelchair (FMS level 1); wkr: walker (FMS level 2); cr: crutches or sticks (FMS levels 3 & 4); Independent (FMS levels 5 & 6); yrs: years.
In the home setting, those in GMFCS level III who used crutches pre-operatively (the majority) have a 75% chance of remaining on crutches or becoming independent (walking without devices) at 5 years. Those who used a walker pre-operatively have a 70% chance of requiring less assistance (crutches or independent). In the school setting, those who used a walker before surgery have a 50% chance of requiring less assistance and 23% chance of using a wheelchair. Those on crutches at school before surgery have a 54% chance of staying on them at 5 years, but also a 40% chance of requiring more assistance (walker or wheelchair). For the community setting high numbers required wheelchairs pre-operatively and this remained high at 5 years (68%); however, there was also a 32% chance of progressing to a walker or crutches. As distances became greater there was increased probability of requiring more assistance at 5 years post-operatively. Overall, for the home and school settings those on crutches at baseline were more likely to remain on them at 5 years, whereas those using a walker at baseline were more likely to change to either less assistance (crutches) or to using a wheelchair.
There were no striking differences in probabilities of assistive device requirements between 2 and 5 years post-operatively in relation to baseline. This suggests stability of assistive device requirements and no remarkable change in mobility status between 2 and 5 years.
Discussion
This study reports longitudinal changes in functional mobility following SEMLS for children and adolescents with CP, GMFCS levels I–III. The majority of children showed either stability of mobility or change to less assistance required, as reported by the FMS. The study findings have implications for considering the effects of surgery on mobility as compared with natural history, the stability of the GMFCS, and the impact of the environment on mobility methods.
The expanded and revised GMFCS (28) demonstrates how assistance required for mobility can change with natural history as children enter late adolescence with the effects of growth and development and progressive musculoskeletal pathology. Those in level II generally walk without assistance up to the age of 12 years, but may choose to use assistance for longer distances when they become adolescent and prepare to enter adulthood. In addition, those in levels III and IV may increasingly rely on wheeled mobility in adolescence and adulthood, as compared with when they are younger.
The motor growth curves provide evidence of that risk of decline in gross motor function for adolescents in level III–V as they enter adulthood (6). In addition, Day et al. (10) estimated the probabilities of losing or gaining ambulatory ability through adolescence and young adulthood using a large database of children and young adults in GMFCS levels I–IV (10). Like the curves demonstrated in the study by Hanna et al. (10), those who walked without difficulty at a younger age have a much higher chance of maintaining that later in life. Those equivalent to GMFCS III who used a wheelchair at age 10 years had a 34% chance of losing ambulatory ability by age 25, whereas those who did not use a wheelchair had only a small chance of declining mobility skills.
The evidence from the current study goes against the suggestion that the natural history is of declining function for adolescents with CP in the second decade of life, by showing that mobility of those in GMFCS level III was mostly stable or improved. This can be explained by the characteristics of the study samples. Despite the studies by Day et al. (10) and Hanna et al. (6) involving large databases of children, neither provides information on surgical or therapeutic interventions the children may have had, which was likely to have been quite varied. The current study reports a select group of children who all had SEMLS followed by a well-defined and comprehensive post-operative rehabilitation programme. The results therefore provide further evidence for the stabilizing effect of SEMLS on mobility in this group.
A key result from the current study was that children within GMFCS level III who were using a walker pre-operatively in the home and at school have a very good chance of progressing to requiring less assistance following SEMLS. This change can be crucial during the adolescent years to improve independence and enhance access to classrooms and offices, etc., as crutches are less cumbersome than a walker. To illustrate this point a case example is described below.
A 7-year-old boy, GMFCS level III, uses quad sticks at home, a posterior walker at school and wheelchair for longer distances in the community (FMS 4, 2, 1). Fig. 2 shows pictures of his standing pre-operatively, where it is clear that he has severe contractures and requires considerable support to stand. His surgery consisted of bilateral: femoral derotation osteotomies, tibial derotation osteotomoies, foot stabilization surgery, distal hamstring lengthening and gastrocnemius recession. At 5 years post-operatively (Fig. 3) his deformities have been corrected and he is able to walk around the home for short distances independently, uses crutches at school and a wheelchair for longer distances (FMS 5, 3, 1). His GMFCS has remained stable at III. He reports increased independence and ease of mobility now that he has progressed from a walker to crutches at school.
Fig. 2. Coronal and lateral views of the lower limbs in a 7-year-old boy with bilateral spastic cerebral palsy, Gross Motor Function Classification System III, Functional Mobility Scale (FMS) 4 2 1 prior to single-event multilevel surgery. Note the flexed, adducted internally rotated hips, the flexed knees, equinus at the ankle and pes valgus deformities. For the purposes of these photographs the subject required the standing support of two adults, one holding each hand.
Fig. 3. At 5 years post-single-event multilevel surgery he remains within Gross Motor Function Classification System III, but his Functional Mobility Scale has improved to 5 3 1. As can be seen in the photographs, he is able to stand comfortably with the aid of two Canadian crutches. The lower limbs have been realigned to improve extension at the hip and knee and the feet are now plantar grade.
The GMFCS is stable over time (23, 29) and this was confirmed in this surgical cohort study with follow-up to more than 5 years after SEMLS. In sharp contrast, a recent study reported change in GMFCS level in most children following various types of orthopaedic surgery across all GMFCS levels (30). Both the frequency and magnitude of improvement (2–3 GMFCS levels) in that study are in contrast to those of the current study and most of the literature, but may be explained by the retrospective assignment of GMFCS levels, despite the reported high agreement between raters. In the current study experienced gait laboratory staff assigned GMFCS levels prospectively. GMFCS level has been shown to change following SEMLS within the rehabilitation phase of the first post-operative year, but not more than one level, with subsequent stabilization by the second post-operative year (20).
Because of the risk of declining gross motor function in people classified within GMFCS III at baseline, this study focused on this group. There were some differences between those in III and those in I/II combined. The latter group functions at a high level with less room to improve on the FMS. This was demonstrated by a higher percentage of those in I/II in the home setting showing no change at 5 years than those in III, who tend to move up FMS levels. In the school setting, although there were still more children in I/II who showed no change than those in III, there was a higher percentage of those in III who showed no change compared with the home setting. In the community setting equal numbers at 5 years showed no change, but slightly more in I/II required more assistance. The finding that gait parameters, but not functional mobility, improves in GMFCS level I/II after SEMLS is highly relevant to goal setting and counselling for this group in comparison with those in III.
Previous to this study, evidence on outcome after SEMLS has been short term or has focused on the body functions and structure domains of the ICF using measures such as 3-dimensional gait analysis and physical examination. Two studies have shown positive changes in some kinematic gait parameters and range of movement with overall stabilization of gait patterns at 14 months (13) and 2 years post-surgery (14) with deterioration in kinematics of control groups. This provides important evidence that deterioration may occur in the absence of surgery. These studies do not, however, provide any information on the functional status of the children, which is more meaningful to the children and families.
Studies that have incorporated functional measures have been short term. A small pilot randomized controlled trial showed clinically significant improvements in gross motor function and improvements in functional mobility at 2 years post-SEMLS (4). Another study assessed change in mobility using the FMS after SEMLS in 66 children with spastic diplegia and showed significant deterioration (need for more assistance) at 3 and 6 months, a return to baseline at 12 months and significant improvement at 2 years post-operatively for all 3 FMS distances (20). Matched pairs of children in GMFCS levels I–III were used to examine outcome at 1 year post-surgery, with significant differences in gait parameters, the Pediatric Outcomes Data Collection Instrument (PODCI) expectation subscore and Pediatric Quality of Life Inventory (PedsQL) Physical Functioning subscore, but not for other functional subscores (15). Significant improvements were found on gait parameters and oxygen cost, but only modest improvements (less than one level) on the Functional Assessment Questionnaire for 135 children at a range of 8–24 months post-surgery (16).
Long-term outcome studies show improved kinematic and temporospatial gait parameters at a range of 4–6 years post-operatively and variable improvements in physical examination measures (18, 19). Overall, there has been limited evidence on short-term functional changes after surgery and none on long-term functional changes. The current study provides some evidence of longer term functional changes, with a focus on mobility and assistance required. It found that, for children in GMFCS level III pre-operatively, mobility status is generally stable or improved (require less assistance) at 5 years post-operatively, with a small number of children requiring (or at least using) more assistance. The concept of surgery having a maintenance effect as a desired outcome is supported by studies comparing surgical and control groups (13, 14) as well as studies on the natural progression of gait, which show deterioration in gait parameters in growing children who have not had surgery (7, 8).
This study emphasizes the impact of the environment on the assistance required for mobility. Mobility in daily life is influenced by environmental factors and age (31), and environmental setting influences methods of mobility used by children with CP (32, 33). As distances increased and the environment was less familiar, more assistance was used as shown by the most common methods used pre-operatively (crutches or sticks at home, walker at school and wheelchair in the community). At 5 years after surgery those in GMFCS III were still most likely to use crutches at home and for school. Wheelchairs remained the most likely in the community, but there were higher chances of requiring less assistance. Following SEMLS it may be easier for children to walk longer distances with less assistance. Crutch use was more stable, i.e. there were higher probabilities of remaining on them, whereas those on walkers have more chance of choosing to use crutches or wheelchairs. This is not surprising considering that as children become adolescents and young adults and are aiming for self-sufficiency, walkers are cumbersome and difficult to manage.
The FMS is ordinal, and changing up levels might be considered improvement and down as deterioration. However, requiring more assistance does not necessarily translate to loss of function. In the initial post-operative period, change to less assistance can be considered as improvement. In the longer term, however, personal choice becomes an important factor in functional status; an adolescent may choose to use a wheelchair rather than a walker at school to optimize independence, speed and safety, and this should not automatically be considered evidence of deterioration. This aspect of personal choice and the different demands that come into play during adolescence may help to explain why some children required more assistance in different environments in the longer term.
Limitations of this study include the relatively small subgroup of children in GMFCS III analysed separately, despite the large overall sample size. Because SEMLS is individualized for each child with CP, there were variations in surgical procedures. Although there was no control group in this study to compare with, the longitudinal modelling of the data allowed for examination of changes in mobility over time within the group, which was the primary goal of the study. Randomized controlled trials have practical and ethical limitations when long-term follow-up is being examined. The sample reflected the research question and focused on children in GMFCS levels I–III who had SEMLS for gait correction, therefore the results can only be generalized to this population.
In conclusion, this study provides some evidence of expectations for assistance required for mobility several years following SEMLS. GMFCS levels remained stable, but more change was seen in assistance required by those in level III compared with those in I/II. Children in level III are more at risk of declining gross motor function as they enter adulthood. SEMLS aims to maintain gross motor function to prevent that decline. This study showed that mobility is generally stable or improved at a mean of 5 years post-surgery; however, a small number of children required more assistance to facilitate mobility.
Acknowledgement
This study was supported by the Victorian Government’s Operational Infrastructure Support Program.
References