Serdar Kesikburun, MD, Özlem Köroğlu Omaç, MD, Mehmet Ali Taşkaynatan, MD, Ahmet Özgül, MD and Arif Kenan Tan, MD
From the Department of Physical Medicine and Rehabilitation, Turkish Armed Forces Rehabilitation Center, Gülhane Military Medical Academy, Ankara, Turkey
OBJECTIVE: We report here a case of neoplastic brachial plexopathy detected by musculoskeletal ultrasonography in a patient with chronic cervicobrachialgia.
Methods/results: A 71-year-old man presented at Gülhane Military Medical Academy, Turkish Armed Forces Rehabilitation Center, Ankara, Turkey with a one-year history of cervicobrachial pain radiating to the left arm and numbness in the medial aspect of the left arm and hand. He could not tolerate magnetic resonance imaging because his pain was exacerbated by cervical extension. Radiographs of his chest and cervical spine were normal. Ultrasound examination of the left brachial plexus revealed segmental fusiform swelling, suggestive for a compressing lesion. Magnetic resonance imaging of the brachial plexus performed under general anaesthesia revealed a left apical lung tumour (Pancoast) infiltrating the brachial plexus.
CONCLUSION: Clinicians should consider neoplastic brachial plexopathy, which is an uncommon diagnosis, when evaluating patients with unrelenting and severe cervicobrachialgia. Musculoskeletal ultrasonography can be beneficial for examining brachial plexus lesions.
Key words: brachial plexopathy; cervicobrachialgia; musculoskeletal ultrasonography.
J Rehabil Med 2012; 00: 00–00
Correspondence address: Serdar Kesikburun, TSK Rehabilitasyon Merkezi 06530 Bilkent/Ankara, Turkey. E-mail: serdarkb@gmail.com
Submitted April 10, 2011; accepted October 10, 2011
Introduction
Neoplastic invasion of the brachial plexus, a rare cause of brachial plexopathy, can mimic symptoms of many common upper limb neuropathies. Therefore, its diagnosis can be missed easily. Neoplastic plexopathy is more common in patients with a previous history of malignant disease. The most common causes are lung (Pancoast tumour), breast carcinoma and lymphoma (1). We report here a case of neoplastic brachial plexopathy (NBP) that was detected by musculoskeletal ultrasonography. A patient with unrelenting cervicobrachialgia, who could not tolerate magnetic resonance imaging (MRI) due to cervical pain, was evaluated with ultrasonography. Abnormal ultrasonographic findings led to a decision to perform brachial plexus MRI under general anaesthesia, which revealed a Pancoast tumour compressing his brachial plexus. The aim of this report is to draw clinicians’ attention to the fact that NBP can be the underlying cause of cervicobrachialgia, and to focus on the benefits of ultrasound scanning of the brachial plexus.
Case Report
A 71-year-old man presented with a one-year history of cervical pain radiating to the left arm and numbness in the medial aspect of the left arm and hand. His cervical pain was exacerbated by looking up. Electrodiagnostic testing led the conclusion that his complaints were due to ulnar neuropathy. He was referred for a cervical MRI twice suspecting radiculopathy, but he could not tolerate the MRI procedure because his pain was exacerbated by extending his neck. Physical examination revealed that he had lost 20 kg of weight in one year. Clinical and neurological examination revealed atrophy of the left deltoid muscle, forearm muscles, intrinsic and extrinsic hand muscles, along with hypoaesthesia of C7-C8-T1 dermatomes and decreased triceps deep tendon reflexes. Routine blood tests were normal, except for an erythrocyte sedimentation rate (ESR) of 75 mm/h (normal < 20 mm/h). Radiographs of the chest and cervical spine were normal. Ultrasonography of the left brachial plexus revealed segmental fusiform swelling, suggestive for a compressing lesion (Figs 1 and 2). The abnormal ultrasonographic findings led us to perform brachial plexus MRI under general anaesthesia. MRI revealed a left apical lung tumour (Pancoast) compressing the brachial plexus and infiltrating C7-T2 vertebrae (Fig. 3). The patient was referred to the oncology department.
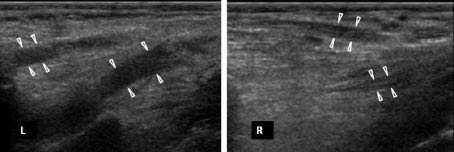
Fig. 1. Ultrasonographic longitudinal image of the left brachial plexus, showing significant segmental fusiform swelling of the trunks in comparison with the contralateral side. The probe is placed in a coronal oblique plane in the inferior interscalene region.
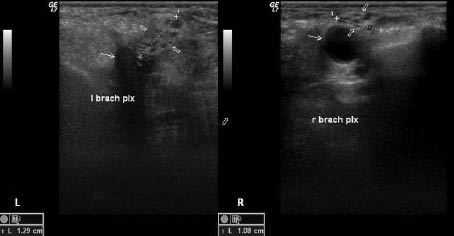
Fig. 2. Ultrasonographic transverse image of bilateral brachial plexuses (thick arrows) at the level of divisions dorsocranial to the subclavian arteries (thin arrows). Significant swelling of the left brachial plexus is visible. The probe is placed in a sagittal oblique plane in the supraclavicular region.
Fig. 3. Brachial plexus magnetic resonance image (MRI). Pancoast tumour (thick arrows) compressing the left brachial plexus (thin arrows) and infiltrating the C7-T2 vertebrae are seen at the apex of the left lung.
Discussion
The most common cause of brachial plexopathies is trauma (2). NBP is an uncommon cause of brachial plexopathy. NBP accounted for 16% of cases in a study of non-traumatic brachial plexopathies (1). It is diagnosed mostly in patients with a previous diagnosis of cancer. Lesions of the brachial plexus are often secondary to neoplasms that reach the plexus by direct extension (Pancoast syndrome) or by metastasis through the lymphatic system from the axilla. Pain in the neck and shoulder is the most frequent symptom of NBP (3). It may radiate down the limb. Pain and paraesthesia in the medial forearm and hand with lower trunk innervations (C8-T1 roots) may be observed. It mimics ulnar neuropathy or C8-T1 radiculopathy with these symptoms. Electrodiagnostic studies most often show axonal loss in the inferior trunk of the brachial plexus (2).
In the present case, the patient had consistent cervical pain, which was intended to be evaluated with MRI, but the patient could not tolerate the MRI procedure as the pain was aggravated by extending his neck. Musculoskeletal ultrasonography was therefore utilized, which had the advantage of being well-tolerated. The patient was evaluated in a comfortable position using ultrasonography. The findings were consistent with compression of the plexus. The swelling in the ultrasonographic images indicated something obstructing nerve fibres. The compression possibly lay in the infero-posterior side of the plexus. The nature of the compressing pathology could not be predicted as a malignancy with only these images. However, the weight loss and the constitutional symptoms alerted us to this pathology; and we therefore performed MRI under general anaesthesia.
Successful attempts have recently been made to use musculoskeletal ultrasonography for imaging the brachial plexus and peripheral nerves. The appearance of peripheral nerves, or the plexus, depends on its echogenicity, shape and echotexture of the surrounding tissues (4). The direction of the nerves or trunks determines the image obtained. Ultrasound scanning of the brachial plexus should be systematic and based on detection of some anatomical landmarks (5). The roots neighbouring the tubercles of the transverse processes of the cervical vertebrae can be visualized as hypoechoic rounded structures on the short and long axis, 5–7 cm apart from the vertebral foramina, the roots form the trunks in the inferior interscalene area. The trunks following the roots are visualized between anterior and middle scalene muscles. The divisions can be discerned in close proximity to the subclavian artery in an axial cross-section in the supraclavicular region. Crossing down the clavicle, 3 cords and terminal branches run next to the axillary artery. Limitations of brachial plexus ultrasonography can be regarded as the inability to image inside the spinal canal and costaclavicular space. To observe the plexus, the transducer is placed in an oblique anteroposterior plane. The position of the probe can be changed to sagittal and coronal planes. The examination in our case concentrated on the interscalene and supraclavicular regions.
With ultrasonography it is possible to recognize lesions in the brachial plexus region, characterize their nature, assess their extension and relationship to adjacent anatomical structures. It is reported that hypoechoic focal mass or masses and segmental fusiform swelling (diffuse hypoechoic swelling of roots or trunks) are the most common sonographic findings in secondary tumours of the brachial plexus (6). The ultrasonographic images in our case showed swelling of the brachial plexus at the level of trunks and divisions, indicating a mass compressing and obstructing the nerve fibres. However, the mass was not visualized. In addition, there was no Doppler signal obtained.
Conclusion
When evaluating patients with unrelenting and severe cervicobrachialgia, clinicians should consider neoplastic brachial plexopathy, which is an uncommon diagnosis. Musculoskeletal ultrasonography can be beneficial for examining brachial plexus lesions, especially when MRI is not tolerated by the patients.
References