OBJECTIVE: The aim of this study was to investigate: (i) the feasibility of delivering a multi-modal knowledge translation intervention specific to the management of acute post-stroke unilateral spatial neglect; and (ii) the impact of the knowledge translation intervention on occupational therapists’ knowledge of evidence-based unilateral spatial neglect problem identification, assessment and treatment, and self-efficacy related to evidence-based practice implementation.
DESIGN: A 3-period (pre-post) repeated measures design.
SUBJECTS: Acute care occupational therapists treating patients with post-stroke unilateral spatial neglect were recruited from two major Canadian cities.
METHODS: Participants completed two pre-intervention assessments, took part in a day-long interactive multi-modal knowledge translation intervention and a subsequent 8-week follow-up, and completed a post-intervention assessment. Knowledge of evidence-based problem identification, assessment and treatment of unilateral spatial neglect, and self-efficacy to perform evidence-based practice activities were measured using standard scales.
RESULTS: The intervention was tested on 20 occupational therapists. Results indicate a significant improvement in knowledge of best practice unilateral spatial neglect management (p < 0.000) and evidence-based practice self-efficacy in carrying out evidence-based practice activities (p < 0.045) post-intervention.
CONCLUSION: Use of a multi-modal knowledge translation intervention is feasible and can significantly improve occupational therapists’ knowledge of unilateral spatial neglect best practices and self-efficacy. The findings should help advance best practices specific to the management of post-stroke unilateral spatial neglect as well as informing knowledge translation studies in other areas of practice.
Key words: knowledge translation; evidence-based practice; stroke rehabilitation; occupational therapy; unilateral spatial neglect.
J Rehabil Med 2012; 00: 00–00
Correspondence address: Anita Petzold, School of Physical and Occupational Therapy, McGill University, 3630 Promenade Sir William Osler, Montreal, Quebec, H3G 1Y5, Canada. E-mail: anita.petzold@mail.mcgill.ca
Submitted June 8, 2011; accepted September 22, 2011
INTRODUCTION
Fifteen million people are affected by stroke annually (1). More than 40% will experience post-stroke unilateral spatial neglect (USN) (2), an impairment characterized by the inability to orient or respond to stimuli appearing on the contralateral side of the brain lesion (3). USN can affect how an individual perceives their personal, near extrapersonal, and far extrapersonal space (3, 4), and is associated with falls, extended inpatient stays and poor functional recovery (2).
Occupational therapists commonly assess and treat USN, given their training and expertise in the management of visual perception disorders (5). Despite an abundance of standardized assessments (4) and some effective interventions (5, 6), there is evidence that many clinicians fail to use evidence-based practice (EBP) in the management of USN. Indeed, a Canadian survey (7), which elicted information from occupational therapists on the assessments and interventions they would use when treating a patient with USN, as depicted in a case vignette, suggests poor management. Less than 30% of therapists would have used a standardized USN assessment, although the vignette clearly raised concern about the possibility of USN, and only 58% would have offered a USN treatment (7). Similarly, in a multi-centred chart audit investigating acute care management of USN post-stroke, only 13% of charts included the results of any standardized visual perception assessment (8). These results highlight a substantial gap between actual and current USN practice. Most university programmes in Canada have as their mission to graduate generalist occupational therapists rather than specialists. As stroke is a complex condition to treat, it is difficult, without specified postgraduate specialty certificates, to create stroke specialists. This has been recognized by the Canadian Stroke Network, the Canadian Stroke Strategy and the Heart and Stroke Foundation of Canada as being a problem that must be addressed through capacity-building activities aimed at enhancing best practices.
Knowledge translation (KT) is a process proposed to bridge the gap between best practices and actual practices (9). A review of the effectiveness of KT interventions for rehabilitation professionals documents the paucity of research specific to KT interventions (10). It suggests that multi-modal active educational methods (11–13) are likely to be more effective for increasing knowledge and use of best practices, compared with single or passive methods. Given that no study has explored the benefit of a multi-modal KT intervention specific to occupational therapists treating patients with post-stroke USN, it was deemed valuable to investigate the use of a multi-modal strategy aimed at closing the gap between best and actual USN practice.
Thus, the primary objectives were: (i) to create and test the feasibility of delivering a multi-modal KT intervention specific to the management of acute post-stroke USN, and (ii) to evaluate the impact of a multi-modal KT intervention on occupational therapists’ knowledge of evidence-based USN problem identification, assessment and treatment as well as self-efficacy related to EBP implementation. A secondary objective was preliminarily to determine the association between clinician/work environment variables and change in evidence-based USN knowledge acquisition.
METHODS
Research design
A 3-period (pre-post) repeated measures design was used with 2 pre-intervention assessments conducted 1 week apart, a KT intervention consisting of a 7-h in-person interactive session based on Graham et al.’s (14) Knowledge to Action Process model, a KT reinforcement period lasting 8 weeks and, finally, a post-intervention assessment. Occupational therapists working in acute care hospitals were recruited from two Canadian cities and surrounding regions. The primary outcomes were: (i) knowledge of evidence-based USN problem identification, assessment and treatment of a patient with stroke as determined by a standardized 20-item Knowledge Questionnaire; and (ii) clinician self-efficacy to implement the steps of EBP using the EBP Self-Efficacy Scale (15). Ethics approval was obtained from McGill University’s Faculty of Medicine Institutional Review Board, Montreal, Canada. Informed consent was obtained electronically during the first pre-intervention assessment and in-person on the day of the interactive session.
Participant eligibility
Occupational therapists were eligible if they: were registered with their provincial licensing body; had at least 3 months of full-time experience with a stroke clientele in acute care; treated a minimum of two adults with stroke per month; and spoke English.
Sample size
Sample size calculations were performed using PC-Size software (Dallal GE, Version 1.0, Malden, MA, USA). The goal was to determine the preliminary effectiveness of the KT intervention and an effect size around the primary outcome, USN knowledge acquisition, as measured using the Knowledge Questionnaire. A sample of 17 would detect an actual improvement (effect size) in knowledge of a minimum of 15 points from the mean pre-intervention assessment to post-intervention, with power of 80% and an alpha of 0.05 using a 2-tailed test. Given that the questionnaire contains 20 questions each worth 3–8 points, it was deemed that a 15-point difference out of 100 would represent a clinically important change in knowledge above that expected by chance. To account for potential withdrawals, 21 clinicians were recruited.
Recruitment procedures
Occupational therapists were recruited from the provincial professional orders of Quebec and Ontario, Canada. Random sampling was performed using computer-generated numbers. Potential participants were contacted by telephone by a trained assistant who described the study using Dillman’s Total Design Method (16) to maximize recruitment. Eligibility was verified and eligible clinicians were invited to participate.
Data collection
Participating clinicians completed the Knowledge Questionnaire two weeks, and one week, prior to the 7-h in-person interactive session. The questionnaire was completed again 8 weeks later after completion of the KT intervention. Each time the clinician had 30 min within two days to read a vignette depicting a patient with post-stroke USN and complete the questionnaire in relation to how they would manage the patient. If the clinician did not complete the questionnaire within the allotted time, a reminder was sent. A different patient case vignette was used with each administration of the questionnaire, but the questions remained the same.
On the day of the 7-h interactive session, prior to beginning the intervention, the clinician/work environment variables were collected using a structured self-administered measure (15) after which the EBP Self-Efficacy Scale (15) was completed: the Self-Efficacy Scale was re-administered immediately following the session.
Outcome measures
Knowledge Questionnaire. Knowledge of USN best practice management was assessed using the 20-item Knowledge Questionnaire (see abbreviated version in Table I) developed for this study based on the levels of learning from Bloom’s Taxonomy: knowledge, comprehension, application, analysis and synthesis, and, evaluation (17). It includes elements adapted with permission from Menon et al. (18). The questionnaire was created with guidance from experts in questionnaire design and then pilot tested on 4 clinicians in stroke rehabilitation. After feedback and revision, it was further validated on 3 experts in KT. The final version contains 4 sections that elicit information on: (i) USN problem identification, (ii) USN assessment use, (iii) USN intervention use, and (iv) general knowledge of USN and best practice recommendations. The questionnaire is scored out of 100 with a higher score indicating greater knowledge.
| Table I. Pre- to post- change on the Knowledge Questionnaire per question |
| Level of question category Learninga | Pre- to post-change in item score | p-valueb |
| Problem identification | | |
| Q1 - S | Which concern(s), if any, do you have regarding potential problems related to visual perception for Mrs P? | 8 | 0.010 |
| Q2 - C | Which type(s) of USN, if any, do you think Mrs P should be assessed for? | 14 | 0.005 |
| Assessment | | |
| Q4 - AP | How soon post-stroke (if at all) do you typically perform your initial evaluation to identify USN? | 6.5 | 0.017 |
| Q5 | If you do not perform an initial evaluation for USN, skip to question #9. | | |
| Q6 - AP | How do you go about evaluating a patient for USN at the initial evaluation? | 5 | 0.046 |
| Q7 - C | In an ideal world, how soon post-stroke would you perform your initial evaluation to identify USN? | 2 | 0.281 |
| Q8 - AP | Which USN screening tool(s) would you typically use to evaluate a patient like Mrs P? | 16 | 0.000 |
| Q9 - AN | In an ideal world, which specific screening tool(s) would you use to evaluate Mrs P given the type of USN she has? | 19 | 0.000 |
| Q10 - AP | Are there any USN assessment tool(s) that you typically use to assess a patient like Mrs P? | 13 | 0.001 |
| Q11 - AP | If you have performed an initial evaluation that identifies USN, do you typically evaluate the patient again? | 6.5 | 0.038 |
| Q12 - AN | In an ideal world, which specific assessment tool(s) would you use to evaluate Mrs P given the type of USN she has? | 18 | 0.001 |
| Treatment | | |
| Q13 - AP | Do you provide treatment to patients who exhibit USN symptoms? | 1 | 0.317 |
| Q14 - AP | If yes, specify which treatment(s) you typically use. | 9 | 0.026 |
| Q15 - AN | In an ideal world, which intervention(s) would you choose to use with Mrs P given the type of USN she has? | 17 | 0.001 |
| Knowledge of USN and best practices | | |
| Q3 - K | Name at least 1 area of the brain which when affected by stroke can result in USN. | 11 | 0.011 |
| Q16 - K | List the USN interventions you believe are effective. | 12 | 0.000 |
| Q17 - K | According to best practices, how soon after the occurrence of a stroke should screening for USN take place? | 15 | 0.005 |
| Q18 - K | List any online resources for clinicians that you are aware of that contain best practices for stroke rehabilitation. | 10 | 0.002 |
| Q19 - K | Were you aware that Canadian Best Practice Stroke Guidelines exist for stroke? | 3 | 0.083 |
| Q20 - K | If you answered “yes” to question 19 – have you seen these Guidelines? | 4 | 0.059 |
| Significance set at p ≤ 0.01. aLevel of learning: S = synthesis, C = comprehension, AP = application, AN = analysis, K = knowledge. bAnalysed using Wilcoxon signed-rank test; Wilcoxon signed-rank value: W+ = 190. USN: unilateral special neglect. |
Evidence-based practice self-efficacy scale. Self-efficacy was evaluated using the EBP Self-Efficacy Scale, a 12-item scale (15) scored out of 100%. Clinicians rate confidence from 0% (cannot do at all) to 100% (certain can do) to perform EBP activities, such as formulating a question. The scale has been assessed for clarity (15).
Clinician/work environment variables. The 47-item measure used to collect clinician- and work-related variables (15) is adapted from Jette et al. (19). It is self-administered and elicits information on: (i) opinions on EBP; (ii) EBP education; (iii) availability of resources at work; and (iv) clinician and work characteristics. The questions have been tested for validity (19) and used previously (7, 15, 20, 21).
Patient case vignettes. The use of vignettes has been found to be a valid means to determine actual practices (22). Three vignettes were created by experts in stroke rehabilitation and were modelled after vignettes previously used for a cross-Canada study on 1800 stroke clinicians (8, 20–21). Each describes a typical patient in the acute phase and gives cues as to the type(s) of USN the patient is experiencing. For example, this vignette gives cues to a possible USN of the near extrapersonal space:
Vignette 1: “Mrs. P is 68 year-old … admitted with a right hemisphere stroke. On initial assessment …Mrs. P is sitting in a regular chair. You enter the room on Mrs. P’s left and observe that she does not notice your entry. At that point the phone rings and Mrs. P has difficulty locating the phone to her left.”
Knowledge translation intervention development
The KT intervention was created based on a series of steps. First, we conducted a focus group composed of occupational therapists treating patients experiencing USN to explore their perceptions on effective educational strategies and on barriers and facilitators to the use of best practices when managing patients in the acute phase. This step is thought to be essential (14) as it maximizes the potential effectiveness of a KT intervention by tailoring it to the specific learning needs of the target audience.
Next, we reviewed learning theories (17, 22) to determine those that would be optimal. The learner-centred model (22) places the responsibility of learning on the student, and requires the instructor to serve as a facilitator, in contrast to didactic lectures where the responsibility of transmitting knowledge falls on the instructor. Bloom’s Taxonomy (17) categorizes levels of learning including: knowledge, comprehension, application, analysis, synthesis and evaluation. A combination was used in building the intervention.
Knowledge translation intervention procedures
The 7-h interactive session was provided by 4 occupational therapists, 2 with doctoral level training, all with expertise in USN. The day was divided into didactic lectures, hands-on sessions, use of e-learning resources, and dissemination of summary information.
The didactic component included a refresher on neuroanatomy of USN, best practice assessment and effective interventions, as well as the latest research on lesion location. Because a sense of self-efficacy is linked to engagement in EBP activities (15, 23), a didactic lecture was given on searching the literature using the Physiotherapy Evidence Database (PEDro) Scale (24) to appraise randomized trials, and, detailing levels of evidence of intervention effectiveness (25). The Professional Evaluation and Reflection on Change Tool (PERFECT) (18) was also used to help clinicians explore change clinical practice over the past year related to problem identification, assessment, intervention and referral practices for USN; reasons for change, as well as facilitators and barriers to actual and desired change. After completion of the PERFECT there was discussion on self-efficacy in using EBP to incite change in daily practice. During the practical hands-on sessions clinicians administered assessment tools and interventions.
Clinicians were introduced to e-learning resources, StrokEngine and StrokEngine-Assess (25) (www.strokengine.ca) (4) that include a USN module with information on assessment tools and interventions, best practice recommendations, and an interactive e-learning component (26) with “clinician how-to” guidelines for USN management (27). Clinicians were also given a USN pocket card (created for this study) that summarizes USN best practices specific to assessment and treatment.
For the 8-week reinforcement period, each clinician was given password-protected access to Web-CT, an online classroom where they had access to USN-related learning materials and could participate in discussion forums. Clinicians were also requested to browse the USN modules of StrokEngine (4) and StrokEngine-Assess (25) and were sent reminder e-mails every 2 weeks to encourage their use of these resources. Clinicians were instructed to keep a log of the time spent and activities completed on Web-CT and StrokEngine (4), and to submit this log by e-mail on a bi-weekly basis. A tracker option monitored time spent on Web-CT but not specific activities.
Data analysis
Recruitment and intervention feasibility was explored by examining the percentage of those who were contacted, eligible, and received employer permission to participate as well as participation intensity. Descriptive statistics were used to characterize the clinician/work environment variables. As a preliminary analysis of effectiveness, and to gain an estimate of effect size, a pre-post comparison of mean scores on the Knowledge Questionnaire was performed using repeated measures analysis of variance (ANOVA) (28).
To explore associations between clinician/work environment characteristics and knowledge acquired, Spearman’s rank correlation analyses were performed (28). Only 7 variables (age, degree obtained, years of experience, supervision of students, number of patients with stroke seen per day, stroke research conducted in setting, and, presence of a stroke team) were adequately distributed when dichotomized or trichotomized to allow analyses. In addition, change on the Knowledge Questionnaire from pre- to post-intervention for each question was analysed using the Wilcoxon signed-rank test (28).
A paired t-test was used to compare pre- and post-self-efficacy scores (15). To determine the correlation between change in self-efficacy and change on the Knowledge Questionnaire, a Pearson product-moment correlation was performed (28). Spearman’s rank correlation analyses (28) were used to correlate clinician participation in the 8-week reinforcement period (yes/no) and change on the Knowledge Questionnaire; as well as participation (yes/no) and change on the Self-Efficacy Scale (15).
RESULTS
Participants
From 44 clinicians randomly selected from the professional lists, 35 were contacted by telephone using vigorous strategies. Two were ineligible and 12 (36%) refused to participate.
Of 21 clinicians who agreed to participate, 20 completed the study (1 withdrew for medical reasons). Ninety-five percent were female aged 23–51, 70% held a bachelor’s degree and 95% worked in a teaching institution. Fifty percent had between 4 and 10 years of clinical experience in stroke and 50% treated on average 2–5 patients with stroke per day. While most supervised students (n = 16), only half worked on a stroke team or had stroke research conducted in their setting.
Feasibility of providing a multi-modal knowledge translation intervention
Of the 12 occupational therapists who refused to participate, 5 did not receive employer permission. Four indicated personal reasons and 3 were not interested.
During the 8-week reinforcement period, 50% (n = 10) of participants submitted bi-weekly logs documenting their activities and time spent on Web-CT/StrokEngine (4). Web-CT tracking confirmed that 10 clinicians (50%) never logged on. Activities carried out included reading posted materials as well as use of the discussion board.
Change in knowledge from pre- to post- intervention
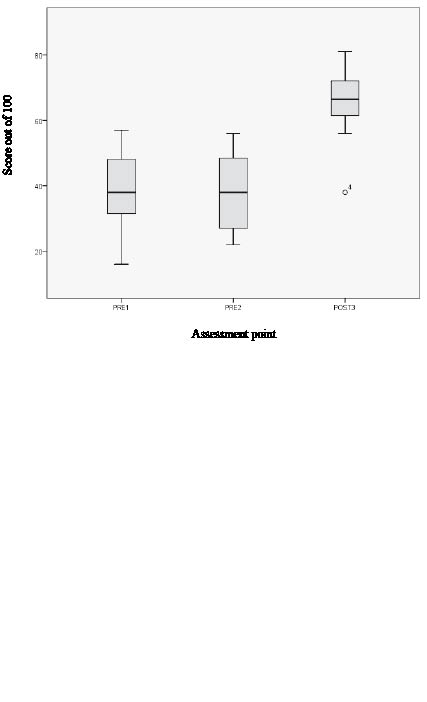
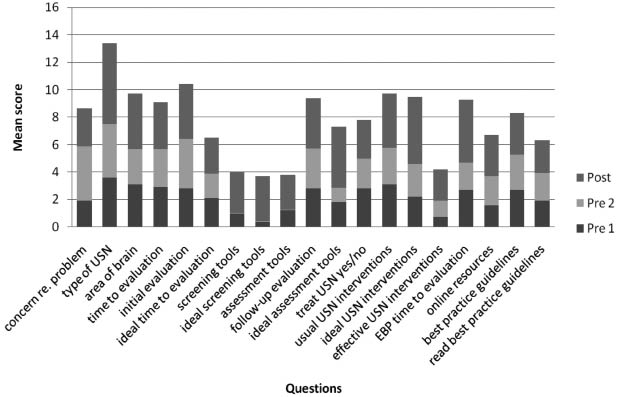
The 2 pre-intervention mean scores (and standard deviations (SD))on the Knowledge Questionnaire did not differ (39.65 (SD 11.25) and 38.05 (SD 11.17), respectively). The mean post-intervention score was significantly higher (65.06 (SD 9.62); F-test = 192.16; degree of freedom (DF) = 19; p < 0.000) ranging from 15 to 42.5 points (see Fig. 1). Fig. 2 shows the group score on each question at each assessment point. The mean change in knowledge from pre- to post-assessment on each question from the Knowledge Questionnaire is presented in Table I, with significance levels indicated at p ≤ 0.01. When analysed by sub-category (problem identification, assessment, intervention, and, knowledge of USN and best practice guidelines), there were more correct answers post-intervention vs pre-intervention in all categories. In terms of problem identification, 95% of clinicians could differentiate the 3 types of USN following the intervention, compared with 58% beforehand. Significantly more correct answers were seen in 4 out of 8 screening and assessment questions: pre-intervention, 15% of clinicians differentiated a screening tool such as the Line Bisection Test (29) from an assessment tool such as the Rivermead Behavioural Inattention Test (30), compared with 95% post-intervention. In terms of intervention, significantly greater knowledge of effective interventions was seen post-intervention; 90% compared with 15% pre-intervention. Significant improvement was also found in 4 out of 6 questions related to general knowledge of USN and best practices. One-hundred percent could identify online learning resources specific to USN post-intervention vs 40% pre-intervention (Table I).
Fig 1. Change in mean Knowledge Questionnaire total score by assessment point (n = 20). Box-plot: lowest score, lower quartile, median quartile, upper quartile, highest score; °4=outlier
Three of the 7 potential explanatory variables were significantly correlated with greater mean change in scores on the Knowledge Questionnaire: bachelor’s vs master’s degree (28.21 (SD 8.09) vs 23.3 (SD 9.69); supervising students vs not (29.33 (SD 7.64) vs 25.21 (SD 8.03)); and, being part of a stroke team vs not (29.55 (SD 9.26) vs 24.86 (SD 7.37)). The mean baseline Questionnaire scores according to these descriptors were: (bachelor’s/master’s: 37.43 (SD 11.92) vs 42.17 (SD 7.01); supervising students/not: 42.21 (SD 8.97) vs 25.37 (SD 4.92); stroke team/not: 30.37 (SD 9.02) vs 35.79 (SD 12.23)).
The 10 clinicians who logged on to Web-CT during the 8-week reinforcement period did so 1–5 times and reported reading about USN on Strokengine for anywhere from 15 min to 2 h (mean 45 min (SD 11.43)). Those who logged on had higher Knowledge Questionnaire scores both pre-intervention (p < 0.035) and post-intervention (p < 0.031) than those who did not log on (n = 10).
Self-efficacy
For the group as a whole, a significant change (paired t-test = –2.144, DF = 19, p = 0.045) in EBP self-efficacy was seen from pre- to post-intervention. There was a weak positive correlation between post-intervention self-efficacy and knowledge gain (r = 0.187). There was a weak negative correlation between post-intervention self-efficacy and having logged on to Web-CT and StrokEngine (yes/no) during the reinforcement period (Spearman’s correlation coefficient = –0.089), such that those with higher self-efficacy were less likely to ever log on.
DISCUSSION
To our knowledge this is the first study to test a multi-modal USN KT intervention aimed at increasing best practice knowledge in occupational therapists treating individuals with stroke. While this was a feasibility study with a small sample size, significant improvements in knowledge in all key components essential for best practice management of post-stroke USN were found. Encouragingly, these improvements were observed after the 8-week reinforcement period, suggesting that the knowledge was not simply retained short-term. While several studies have found an increase in knowledge immediately following a KT intervention (15, 31–34), our study design allowed for an estimate of actual knowledge acquired and sustained over time.
Important changes in knowledge of USN problem detection were seen. For example, most clinicians were unaware of the existence of 3 types of USN (5) prior to the KT intervention. This is an important gap in practice, given that each type of USN has different functional limitations associated with it, and each implies different decision-making regarding assessment and treatment (3).
Knowledge changes that are important to clinical practice were also seen in the area of assessment. For example, the ability to differentiate between a screening and assessment tool is critical to problem identification. Typically, screening tools are quick and highlight areas of concern that help guide the clinician in choosing a standardized assessment that has the capacity to detect impairment more accurately and that can often also monitor a patient’s change over time (35). Pre-intervention, clinician responses suggested that the majority were utilizing screening and assessment tools interchangeably. Furthermore, many clinicians could correctly choose the appropriate screening and assessment tools for the evaluation of near extrapersonal neglect, but were unable to choose tests that measure personal and far extrapersonal neglect (Fig. 2). One possible explanation is that few screening and assessment tools exist for personal neglect and only one standardized assessment tool exists for far extrapersonal neglect (35); the Catherine Bergego Scale (36). Another plausible reason is that, given that we found that many clinicians were unaware that there were 3 types of USN at pre-intervention, they would not have known to assess for all 3.
The best practice pocket cards were created as part of this KT intervention in line with the Knowledge to Action Process Model (14) recommending that clinicians have access to synthesized materials. This card can be accessed and reproduced from the “clinician how-to” section of the USN module on StrokEngine (27).
Our results show that those who had higher education and who supervise students had a higher baseline knowledge of stroke-specific EBP, which is in line with previous research (8, 21, 23). Our results also indicate that those who worked on a stroke team had greater mean change in Knowledge scores. The presence of a stroke team may be an indicator that the worksite is supportive of continuing education, and it could be postulated these clinicians took advantage of this learning opportunity. The presence of a stroke team has been shown to be associated with increased stroke rehabilitation EBP use (8, 15, 21, 23). Why clinicians on a stroke team did not have higher scores at baseline is an interesting query. It may be that USN assessment and treatment is very specific and, as we have found in previous studies (7, 8) not always well understood, even when a stroke team is present. Interestingly, 50% of participants were part of a stroke team, which is well above what is expected from a random sample of clinicians (37). It may be that managers of stroke teams were more open to granting clinicians a full day to attend training. EBP self-efficacy changed significantly. Interestingly, higher scores were negatively correlated with logging on to Web-CT (4) during the reinforcement period. This is perhaps because clinicians with higher self-efficacy did not feel the need to improve their knowledge and skills, whereas those with lower self-efficacy did.
Fig. 2. Mean question score on the Knowledge Questionnaire by assessment point (n = 20).
Half of participants did not log on during the reinforcement period. These findings are similar to those of McClusky et al. (12), who tested a KT intervention on occupational therapists working with varying clientele. Lack of time is often cited as a prominent barrier (12, 13). However, interestingly, in our study those who used Web-CT during the reinforcement period had higher mean scores on the Knowledge Questionnaire at both the pre- and post- intervention than those who did not use Web-CT. One explanation is that some clinicians are more likely to seek out new evidence than others, based on their personal learning style or trait. According to a 2007 study (38) on 243 stroke clinicians tested on a standardized questionnaire that discriminated 4 possible practice style traits (seeker, receptive, traditionalist, pragmatic), only 2% of occupational therapists were seekers. A seeker bases his or her practice on published evidence and frequently uses electronic resources. It is plausible that in our study clinicians who used the online resources were seekers. It is also possible that those agreeing to participate in the study were more likely to be seekers or receptives (open to new learning) rather than falling in the category of pragmatist or traditionalist (38). Seeing as this KT intervention has proven effective in a sample of 20 clinicians, this multi-modal method is likely to be useful at the very least in clinicians who fall in the category of seeker or receptive. In the future it would be useful to study the effect of various knowledge translation strategies that are tailored according to practice style traits as well as according to desired levels of learning.
We used validated cases of patients with stroke to elicit USN management. Some may argue that using vignettes overestimates or underestimates clinical practice vs direct observation. However, their use has been shown to be valid in estimating practice variations (39).
As there was no control group, a limitation of this study design was that change in knowledge may be explained by a Hawthorne Effect rather than the specific intervention provided. However, this is unlikely, given that clinicians exhibited no change in knowledge between the two baseline assessments of knowledge. The main outcome was knowledge change measured using a standard online questionnaire. A possible limitation of using an online test of knowledge includes clinicians looking to outside sources for answers. We attempted to reduce this potential by reducing the amount of time that the clinician had to complete the questionnaire. However, it could be argued that a clinician’s know-how regarding where to seek information in a timely fashion is one of the EBP behaviours that leads to improved practice. As such, if a clinician did use resources more efficiently at post-intervention testing to identify correct best practice responses, this in itself is an important part of becoming a more knowledgeable EBP practitioner.
Statistically it could be argued that we should not have summed the items on the Knowledge Questionnaire: we have presented item by item change in responses as well as the total change score, to allow readers to examine the data in both ways. Lastly, despite a small sample size significant differences were found in both the primary (knowledge) and secondary (self-efficacy) outcomes. What was not as plausible to fully answer with this sample size was the contribution of the various explanatory variables to knowledge change.
In conclusion, these findings suggest that the use of a multi-modal KT intervention in the context of continuing education and based on understanding context-specific barriers and facilitators to EBP use (14) can significantly improve occupational therapists’ knowledge of best practices in the management of post-stroke USN. This study is important in demonstrating that a multi-modal intervention is feasible and acceptable to rehabilitation clinicians.
The findings from this study are useful in a number of ways. First, they are directly useful in informing a randomized control study that will investigate the benefit of this form of KT intervention on important endpoints in USN management that have yet to be measured, including change in clinical practice and most importantly, change in patient outcomes. This study, both in its design and theoretical foundation, should also prove useful in a larger context. There are many areas of rehabilitation medicine where there are substantial gaps between best practices and actual practices (20, 21, 32). Encouragingly, the use of a multi-modal intervention targeted at the specific needs of clinicians is showing promise in changing practice knowledge.
ACKNOWLEDGEMENTS
Anita Petzold is funded by a fellowship award from the Fond de la Recherche en santé du Québec (FRSQ), and Nicol Korner-Bitensky by a senior career award from the FRSQ. Nancy M Salbach is funded by a Heart and Stroke Foundation of Ontario Clinician Scientist career award and, Sara Ahmed by a junior researcher salary award from the FRSQ. Anita Menon is funded by a doctoral award from the CIHR program (Innovations in Patient Safety and Knowledge Translation). This work was funded by an Edith Strauss Knowledge Translation Grant from the School of Physical and Occupational Therapy at McGill University. We would also like to acknowledge the Canadian Stroke Network/CIHR for their continued support, and Julie Lamoureux for her statistical support.
The authors report no conflicts of interest.
REFERENCES