Linda Nordin, MSc1,2 and Ia Rorsman, PhD1
From the 1Department of Neurology, Skane University Hospital – Lund, Lund, Sweden and 2Rehabilitation and Research Centre for Torture Victims, Copenhagen K, Denmark
Linda Nordin, MSc1,2 and Ia Rorsman, PhD1
From the 1Department of Neurology, Skane University Hospital – Lund, Lund, Sweden and 2Rehabilitation and Research Centre for Torture Victims, Copenhagen K, Denmark
OBJECTIVE: The aim of this study was to design a trial that could evaluate the effect of acceptance and commitment therapy as a group-intervention for multiple sclerosis patients with psychological distress.
DESIGN: Randomized controlled trial with assessment at pretreatment, end of treatment, and at 3-month follow-up.
SUBJECTS: Multiple sclerosis outpatients with elevated symptoms of anxiety and/or depression (n = 21).
METHODS: Patients were randomly assigned to acceptance and commitment therapy or relaxation training. Both treatments consisted of 5 sessions over 15 weeks containing didactic sessions, group discussions, and exercises. Outcome was assessed by self-rated symptoms of anxiety, depression, and a measure of acceptance.
RESULTS: At 3-month follow-up, the relaxation training group had a significant decline in anxiety symptoms whereas the acceptance and commitment therapy group showed a maintained improvement in rated acceptance at follow-up.
CONCLUSION: The results reflect the different emphases of the therapies. Acceptance and commitment therapy is aimed at living an active, valued life and increasing acceptance, while relaxation training focuses directly on coping strategies to handle emotional symptoms. The results are preliminary, but supportive of further study of brief group interventions for reducing psychological distress in patients with multiple sclerosis.
Key words: multiple sclerosis; cognitive behaviour therapy; relaxation therapy; psychotherapy; group.
J Rehabil Med 2012; 44: 87–90
Correspondence address: Ia Rorsman, Department of Neurology, Skane University Hospital – Lund, SE-221 85 Lund, Sweden. E-mail: Ia.Rorsman@med.lu.se
Submitted April 27, 2011; accepted August 30, 2011
INTRODUCTION
Multiple sclerosis (MS), one of the most common neurological disorders, is a chronic inflammatory demyelinizing disease that affects the central nervous system. Symptoms vary widely and can affect visual, motor, sensory, coordination, balance, bowel, bladder and sexual functioning. Symptoms of anxiety and depression are common, and linked to social dysfunction, decreased adherence to treatment, somatic complaints and lower functional status (1). In a Cochrane review from 2007 it was concluded that the scope for using psychological interventions in MS is broad, while the evidence-base is still relatively small (2). However, there is reasonable evidence that cognitive behavioural therapy (CBT) is beneficial in the treatment of depression, and in helping people adjust to, and cope with, having MS (2).
Acceptance and commitment therapy (ACT) is a modern CBT approach, designed to improve functioning and quality of life by increasing a person’s ability to stay active and act in concordance with personally held values (3). The approach also includes practice in mindfulness and acceptance. Overall, the effects of ACT look promising (large effect size compared with waitlist conditions, and moderate effect size compared with treatment-as-usual or other active treatment) although further studies are needed in which ACT is compared with empirically supported treatments (4, 5). One uncontrolled study has shown encouraging results on ACT and MS (6).
The aim of this pilot trial was to design a study that, in a larger follow-up study, could evaluate the effect of ACT as a group-intervention for MS outpatients with anxiety and/or depression. ACT is a brief intervention (manuals with as little as 3 sessions), which gives cost benefits and enables implementation in outpatient settings (7). ACT was compared in a randomized controlled trial with relaxation training (RT), a behavioural intervention that previously has been successfully applied on patients with MS (8). RT is a commonly used component of CBT and, given the extensive data in support of its efficacy, is often compared with other psychological methods (9, 10).
METHODS
Subjects
Twenty-one adult patients with MS (Fig. 1), according to McDonald criteria, were included after obtaining informed consent. Patients with no to moderate functional disability (< 6.0 on the Expanded Disability Status Scale; EDSS) (11), who were referred by their doctor as having difficulties coping/adjusting to their disorder were recruited from the Department of Neurology, Lund University Hospital, Sweden, in March 2008. Invitation to participate was sent to patients with elevated symptoms of anxiety and/or depression (≥ 10 on the Beck Depression Inventory (BDI) (12), and/or >8 on one or both of the subscales of Hospital Anxiety and Depression Scale (HADS) (13)). Patients with a history of serious psychiatric illness or current alcohol or substance abuse were excluded.
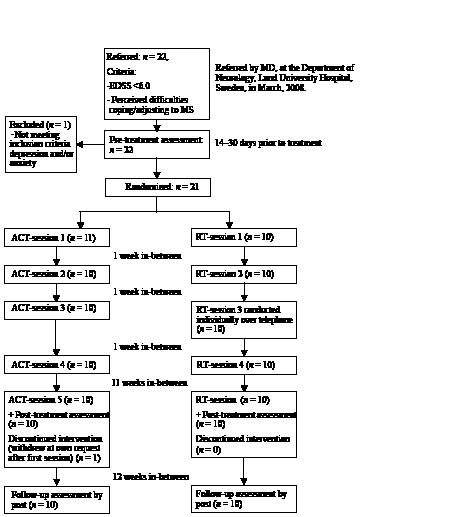
Fig. 1. Treatment flow. EDSS: Expanded Disability Status Scale; MS: multiple sclerosis; ACT: Acceptance and commitment therapy; RT: relaxation training.
Procedure
Patients were randomly assigned by an independent co-worker to one of two treatment groups following pairwise matching based on EDSS, anxiety, and depression scores. Both programmes, ACT and RT, were largely based on previously published manuals (3, 7, 14, 15). Treatments contained didactic sessions, group discussions, and exercises.
The ACT intervention is based on 6 core processes: defusion, acceptance, mindfulness, values, self as context and committed action (3). For the ACT group, the first session focused on didactic and experiential reflections of avoidance and control strategies and the long-term costs and consequences of these. Sessions 2 and 3 focused on mindfulness, acceptance, and cognitive defusion techniques as alternatives. In session 4, patients explored personally held values and how to live life in accordance with these. At the 3-month booster follow-up these strategies were rehearsed.
For the RT group, the rationale of RT was explained in session 1. In sessions 1–3, the relaxation training was presented and practiced in a step-wise fashion in accordance with the manual (14). Session 4 was an individual session over the telephone in which each participant received personal guidance on how to carry out the programme. At the 3-month booster follow-up, the programme was rehearsed. The protocols (in Swedish) are available on request.
RT is normally given as a 10-week session treatment. To match the benefits of the short-term ACT therapy, RT had to be shortened to a 5-session design (15). Both groups received home exercises and CDs containing audio versions of the relaxation techniques (RT group) and mindfulness exercises (ACT group).
Both interventions were given by the authors of this paper, who are psychologists working at the clinic. One author has extensive experience in RT and some ACT training (5 days). The other has extensive training in ACT and teaches ACT for licensed psychologists at the Swedish Psychological Association’s cooperation for continuing education.
Assessment
The following outcome measures were used: HADS; BDI; Acceptance and Action Questionnaire (AAQ-II) (16). AAQ-II assesses the ability to accept undesirable thoughts and feelings. Any changes in treatment plan or relapses were recorded from the patient’s journal. Patient’s expectations vs credibility of treatment was recorded after the first session and at the end of treatment, respectively (17).
All treatment effect analyses were by intention-to-treat. For participants who dropped out, scores from the previous assessment were carried forward. Scoring and data analyses were conducted blindly. Between-group comparisons on patient background characteristics were conducted with Mann-Whitney U tests and χ2 analyses. Group comparisons in changes on outcome variables were assessed using Mann-Whitney U analyses on difference scores. On each variable, two difference scores were calculated (pre-treatment to post treatment; pre-treatment to follow-up). Within-group comparisons to pre-treatment scores were calculated with a Wilcoxon signed-rank test for each treatment group. Two-tailed tests were used in all analyses.
RESULTS
A total of 20 patients (8 women in each group) completed the treatment. There were no significant differences at randomization between the 2 treatment groups with regard to age, length of illness, gender, marital status, occupational status, EDSS, or pre-treatment outcome data. Background information is presented in Table I.
| Table I. Baseline characteristics and outcome data on patients randomized to acceptance and commitment therapy (ACT) and relaxation training (RT) | ||
| Baseline characteristics and outcome data | ACT group (n = 11) | RT group (n = 10) |
| Age, years, median (IQR) | 43 (36–45) | 48.5 (38–55) |
| Marital status, married/cohabitant, n | 10 | 7 |
| EDSS, median (IQR) | 1 (1–2.5) | 2 (1–3) |
| Length of illness, years, median (IQR) | 5 (2–12) | 9 (5–16) |
| Reported frequency of homework practice, n | ||
| Daily | 2 | 7† |
| Few times a week | 7 | 3† |
| Rarely–never | 1 | 0 |
| HADS-A, median (IQR) | ||
| Pretreatment | 10 (7–15) | 9 (6–12) |
| End of treatment | 10 (5–14) | 7.5 (5–12) |
| 3 months follow-up | 10 (6–13) | 6 (2–12)* |
| HADS-D, median (IQR) | ||
| Pretreatment | 5 (3–9) | 7 (6–9) |
| End of treatment | 3 (3–11) | 4 (3–7)*† |
| 3 months follow-up | 5 (3–11) | 6.5 (2–10) |
| BDI, median (IQR) | ||
| Pretreatment | 13 (10–20) | 15 (10.5–23) |
| End of treatment | 12 (9–19)* | 13.5 (7.5–17) |
| 3 months follow-up | 10 (7–25) | 11 (5–22) |
| AAQ, median (IQR) | ||
| Pretreatment | 45 (38–49) | 44.5 (41.5–49) |
| End of treatment | 49 (41–53)* | 48.5 (37–62) |
| 3 months follow-up | 52 (41–60)* | 48 (41–58.5) |
| †Between-group difference at p < 0.05 (on outcome measures: based on difference scores from pretreatment). *Within-group difference at p < 0.05 compared with pre-treatment. Scores on HADS-A and HADS-D range from 0 to 21. BDI ranges from 0 to 63. AAQ-II ranges from 10 to 70, with higher scores representing more psychological acceptance. IQR: interquartile range; HADS-D: Hospital Anxiety and Depression Scale-Depression Scale; HADS-A: Hospital Anxiety and Depression Scale-Anxiety Scale; BDI: Beck Depression Inventory; AAQ: Acceptance and Action Questionnaire. | ||
The majority of patients had relapsing remitting MS, whereas 5 patients (2 in ACT and 3 in the RT group) were diagnosed with secondary progressive MS. All patients, except patients with secondary progressive MS, were receiving immunomodulary medication. None of the patients received natalizumab. Two patients (one from each group) had changes in immunomodulating treatment during follow-up. One patient from each group had ongoing psychotherapeutic contacts. Psychopharmacological medication included selective serotonin re-uptake inhibitors (3 patients in each group) and lamotrigine (one from ACT, two from the RT group). Two patients from the ACT group and 3 from the RT group were on full-time sick pay, the remaining patients were employed or in education.
One patient (RT group) had a MS relapse with complete recovery during treatment. Expectations of treatment after the first session did not differ between groups (8/11 patients in ACT and 7/10 in the RT group believed treatment would, or, was likely to, help). Credibility ratings were high at the end of treatment as 90% in both groups responded would recommend treatment.
All significant changes in outcome measures are presented in Table I. Between-group analyses on difference scores yielded a significant outcome on Hospital Anxiety and Depression Scale-Depression Scale (HADS-D) scores, with the RT group showing a larger decline than the ACT group between pre- and post-treatment (p < 0.05). Patients in the RT group reported a higher frequency of daily practice (χ2 = 5.9, p < 0.05) than the ACT group. Within-subject contrasts in the RT group showed significant decrease in HADS-D between pre- and post-treatment (Z = 2,4, p < 0.05) as well as a significant decline in Hospital Anxiety and Depression Scale-Anxiety Scale (HADS-A) from pre-treatment to follow-up (Z = 1,9, p < 0.05). Within-subject analyses in the ACT group yielded a significant decline in BDI scores from pre-treatment to post-treatment (Z = 2.2, p < 0.05), as well as an increase (improvement) in AAQ-II scores from pre- to post-treatment (Z = 2.2, p < 0.05) and from pre-treatment to follow-up (Z = 2.1, p < 0.05).
DISCUSSION
The aim of this study was to conduct a pilot trial that compared ACT, a brief intervention aimed at enhancing acceptance rather than control of negative experiences, with RT, an approach using coping strategies to handle negative psychological symptoms. Patients receiving RT showed a larger decline than the ACT group in depressive symptoms (HADS-D). However, this difference was not maintained at 3-month follow-up. Moreover, and consistent with previous research (10, 18), within-group analysis of RT patients showed a decline in anxiety symptoms (HADS-A) from pre-treatment to follow-up. Although between-group comparisons did not demonstrate any advantage to ACT over RT on any outcome variable, within-group analyses on the ACT group showed an effect on AAQ-II, assessing the ability to accept undesirable thoughts and feelings. Moreover, this result was maintained at follow-up, 3 months after the end of treatment.
These results mirror the different approaches of the two therapies. ACT is aimed at helping the patient accepting psychological pain and leading life in accordance with personally held values, despite irreversable symtoms. RT, on the other hand, focuses directly on coping strategies to handle dysfunctional psychological symptoms. Outcome variables assessing aspects in quality of life, such as social and physical participation and daily functioning may have been more appropriate than symptom scales given the breadth of difficulties associated with MS and the emphasis on behavioral change rather than symptom reduction in ACT.
Inclusion of a wait-list control group would have helped to answer whether any form of brief group intervention could have given the observed effects. In light of existing critisism of available research on ACT (4, 5), the importance of comparing ACT to previously empircally documented treatment was prioritized. Credibility ratings were high and did not differ between groups. The treatment groups differed, however, with regard to homework practice. The majority of RT patients reported practicing daily whereas the majority of ACT patients only practiced a few times a week. This is likely to be a reflection of intrinsic differences in the treatment programmes where the importance of systematic daily practice is emphasized in RT, but less so in ACT. The ACT group was encouraged to integrate the ACT techniques in daily life. Given that homework compliance can be a major obstacle for progress in RT, this can be considered an important advantage to ACT.
This study has several weaknesses, most importantly the limited follow-up period, the absence of an independent treatment evaluation to ensure treatment integrity, and the small number of participants. Given these limitations, the results should be considered preliminary but supportive of further study of short-term CBT treatments for reducing psychological distress in patients with MS. This pilot should be useful in designing such studies.
The importance of continued research in this field is illustrated by studies suggesting that depression and anxiety appear to be undertreated in MS outpatient settings (1). Moreover, whereas clinicians have been found to be more concerned about the physical manifestation of the disease, patients with MS consider mental health to be a critical determinant of overall burden (19). Further focus on empirically proven psychotherapeutic interventions may help bridge this gap and improve the overall quality of life for patients with MS.
Acknowledgements
The authors would like to thank the following co-workers for invaluable referrals of patients to the present investigation: Gun Jadbäck, Lena Asmoarp, Karin Lennartsson, Petra Nilsson, and My Bergkvist.
Conflicts of interest: None to declare.
Funding: Lindhaga Foundation, Sweden.
REFERENCES
