OBJECTIVE: The aim of this pilot study was to describe problems in functioning and associated rehabilitation needs in persons with spinal cord injury after the 2010 earthquake in Haiti by applying a newly developed tool based on the International Classification of Functioning, Disability and Health (ICF).
DESIGN: Pilot study.
SUBJECTS: Eighteen persons with spinal cord injury (11 women, 7 men) participated in the needs assessment. Eleven patients had complete lesions (American Spinal Injury Association Impairment Scale; AIS A), one patient had tetraplegia.
METHODS: Data collection included information from the International Spinal Cord Injury Core Data Set and a newly developed needs assessment tool based on ICF Core Sets. This tool assesses the level of functioning, the corresponding rehabilitation need, and required health professional. Data were summarized using descriptive statistics.
RESULTS: In body functions and body structures, patients showed typical problems following spinal cord injury. Nearly all patients showed limitations and restrictions in their activities and participation related to mobility, self-care and aspects of social integration. Several environmental factors presented barriers to these limitations and restrictions. However, the availability of products and social support were identified as facilitators. Rehabilitation needs were identified in nearly all aspects of functioning. To address these needs, a multidisciplinary approach would be needed.
CONCLUSION: This ICF-based needs assessment provided useful information for rehabilitation planning in the context of natural disaster. Future studies are required to test and, if necessary, adapt the assessment.
Key words: rehabilitation; needs assessment; spinal cord injuries; natural disaster; ICF.
J Rehabil Med 2011; 43: 969–975
Correspondence address: Alexandra Rauch, Swiss Paraplegic Research, CH-6207 Nottwil, Switzerland. E-mail: alexandra.rauch@paranet.ch
Submitted July 12, 2011; accepted September 26, 2011
Introduction
Natural disasters cause immediate physical and mental health problems in the affected area (1, 2). Immediately after a disaster, survival is the primary objective of medical response measures (3). In the aftermath, survivors are often confronted with a lack of medical care, water, food, housing and sufficient sanitary conditions. These critical living conditions entail new risks of early mortality, complications and incomplete or delayed recovery from acquired injuries, and acquiring additional health conditions, such as communicable diseases (3, 4). In survivors of the early phase of a disaster, interactions of acquired health conditions with the environment may have a major impact on levels of functioning. Health maintenance, reintegration into community, and quality of life present major challenges in the mid- and long-term following disasters, in particular in countries with limited health services (5).
Rehabilitation is an essential health strategy within disaster relief. In comparison with early-phase emergency treatments focusing on survival and prevention of complications and infectious disease (3), the target outcome of rehabilitation services is to achieve and maintain optimal functioning in the short- and long-term (6). The need for rehabilitative services increases rapidly after disasters as a consequence of the large number of persons with newly acquired disabilities and the breakdown of systems supporting those with pre-existing disabilities (4). In low-resource countries, in particular, rehabilitative services are frequently underdeveloped or not available (7). When available, they are often provided by international non-governmental organizations (NGOs).
One pre-condition for providing the appropriate amount and type of rehabilitation services is the assessment of the current needs of the affected population (3, 8). Assessment of rehabilitation needs should identify the following factors: (i) problems in functioning; (ii) environmental factors that contribute to these limitations in the particular population; and (iii) the interventions, as well as the human and other resources, required to address the existing needs. Such information is necessary to tailor rehabilitation services to the needs of the affected population and situation of the country. An adequate information base could help to achieve optimal functioning in individuals and populations in the aftermath of a natural disaster.
No instruments for the assessment of rehabilitation needs following natural disasters are currently available. Such an instrument should ideally be based on a common understanding of functioning and disability among all stakeholders and potential service providers. The International Classification of Functioning, Disability and Health (ICF) (9) provides a promising framework. To facilitate the use of the ICF in different areas, including rehabilitation, lists of domains of functioning, selected from the whole classification for specific health conditions, exist in the form of ICF Core Sets (10). Some of the existing ICF Core Sets cover health conditions frequently caused by disasters. These include traumatic brain injury and spinal cord injury (SCI). ICF Core Sets for amputations are currently being developed. Furthermore, ICF Core Sets for neurological and musculoskeletal condition groups are available for use in acute hospitals and early post-acute rehabilitation facilities. For rehabilitation management, documentation tools utilizing ICF Core Sets have already been developed (11). Thus, the development of specific instruments for assessment of rehabilitation needs can build on previous experience with implementing the ICF in rehabilitation management. The vast rehabilitation needs of persons who have sustained SCI from the 2010 earthquake in Haiti represent a specific context for the application of such an instrument.
The aim of this pilot study was to describe problems in functioning and the associated rehabilitation needs in persons with SCI after the 2010 earthquake in Haiti, using a newly developed ICF-based tool.
Methods
Setting and study population
One of the most severe earthquakes ever hit Haiti in January 2010, a developing country considered the poorest in the Western hemisphere. The earthquake immediately killed approximately 220,000 people and caused more than 300,000 acute injuries (12). As a consequence, a huge number of persons suffered from health conditions leading to physical disabilities. Estimations speak of 2,000–4,000 amputees and 100 persons with SCI (13). After emergency interventions, persons with newly acquired disabilities were admitted to several healthcare facilities across the country. In Haiti, there was no governmental rehabilitation facility and no health professionals trained in rehabilitation skills (13). Healing Hands for Haiti (14), a North American non-profit NGO with a local facility in Port-au-Prince, had been one of the few institutions providing rehabilitation services and a training programme for rehabilitation aides (15). With the rapidly increasing number of persons with disabilities from the earthquake the need for rehabilitation services overwhelmed the available capacity in Haiti by a long way (16–18). In order to care for this vulnerable population in the long term, Haiti was faced with the necessity to set up new rehabilitative services. The Action Plan for National Recovery and Development of Haiti (19) has addressed this issue and claims to improve service provision by promoting the creation of rehabilitation institutions.
One organization providing rehabilitative services as a consequence of the earthquake was Haiti Hospital Appeal (HHA) (20), a UK NGO active in Cap-Haïtien in the Northern district of Haiti. Several persons with acquired SCI had been transferred to HHA after receiving emergency treatment elsewhere. HHA staff comprised local nurses, 1 local medical doctor and 2 local physical therapy aides. The local nurses and physical therapist aides received regularly training in the special treatment of SCI by a British nurse employed by HHA and several expatriate volunteers working temporarily at the unit. In addition, a trained Haitian rehabilitation physician from Port-au-Prince supervised rehabilitation care 3 days each week. Five months after the earthquake (in June 2010), a team of the Swiss Paraplegics Group (SPG), with 4 rehabilitation professionals and 1 health scientist, spent 4 weeks at HHA. The SPG team aimed to provide rehabilitative services to the patients, to train the local staff members, and to develop and apply a newly developed instrument for the assessment of rehabilitation needs.
All persons admitted to HHA during the time of the stay of the SPG team for SCI rehabilitation were informed about the study and asked to participate. If they agreed, diagnosis specific information was collected using the International SCI Core Data Set (21) and their rehabilitation needs were assessed. At the time of arrival of the SPG team in June 2010, 18 persons (11 women, 7 men) with SCI were hospitalized at HHA (Table I). Eleven showed complete lesions (AIS A). Only one patient had tetraplegia.
| Table I. Characteristics of the study population (n = 18) according to Spinal Cord Injury (SCI) Core Data Set (21) |
| Characteristics | |
| Sex, female, n | 11 |
| Age, years, mean median (range) | 36.7 35.5 (26–55) |
| Cause for SCI, n Earthquake Traffic accident | 17 1 |
| Level of lesion, n Cervical Thoracal Lumbal | 1 15 2 |
| AIS, n A B C D Unknown | 11 1 3 1 2 |
| Spine surgery, n | 9 |
| AIS: American Spinal Injury Association (ASIA) Impairment Scale. |
Assessment of rehabilitation needs
To collect diagnosis specific information, the International SCI Core Data Set (21) was applied. To assess the rehabilitation needs, the ICF Core Sets for SCI (22, 23) served as the basis for data collection. For this purpose, all ICF categories included in the Brief ICF Core Set for SCI for the early post-acute and long-term context and 3 additional ICF categories from the respective Comprehensive ICF Core Sets were selected (Table II). These 3 ICF categories were selected based on expert opinion considering their importance in the actual context and for future community integration. The extent of a problem in each of the ICF categories was rated on a 3-point rating scale: 0 = no problem, 1 = some problem, 2 = complete problem. ICF categories referring to “Activities and Participation” were rated with the perspective of “capacity” (individual’s ability to execute a task without assistance and/or device) and of “performance” (individual’s actions in the actual environment including support and the use of devices) (9). The differences between capacity and performance ratings depict the impact of the environment on the levels of functioning. The impact of the selected environmental factors was rated either as “facilitator” (no, some, or complete facilitator) or “barrier” (no, some, or complete barrier). An ICF category was rated as “not specified” if too little information was available and as “not applicable” if rating would have been inappropriate. For each individual, the rehabilitation needs related to each ICF category were identified. If there was a need, the health professional who would be required to address the need was determined. To record this needs assessment, a documentation form was developed (Fig. 1).
| Activities and Participation | No difficulty | Some difficulty | Complete difficulty | Not specified | Not applicable |
| d465 | Moving around using equipment | P | 0 | 1 | 2 | 8 | 9 |
| C | 0 | 1 | 2 | 8 | 9 |
| | Description: Is able to move the wheelchair inside of the house but has severe difficulties outside of the building |
| Rehabilitation need: Yes No Type: Physical therapy (Wheelchair training) |
Fig. 1. Extract from the documentation form, example for one ICF category from Activities and Participation. P: Performance: individual’s actions in the actual environment including assistance and the use of devices; C: Capacity: individual’s ability to execute a task without assistance and/or device (10).
Procedure and analysis
The patients’ functional problems and the impact of the environmental factors were rated based on the information collected through patient interviews and the evaluation by the rehabilitation team. After rating the extent of a problem in each ICF category, it was decided whether this resulted in a need for a specific intervention and, if so, which specific intervention type would be required. Based on the individual needs assessments, the descriptives obtained were summarized to identify: (i) the prevalence of problems in functioning; (ii) the areas in which rehabilitation needs existed; and (iii) the type of professionals required to address these needs.
Results
Level of functioning
The level of functioning is presented for all 18 patients with SCI (Table II). In the “body functions” and “body structures” domain, patients showed problems that are typical following SCI, such as complete impairments in “b525 Defecation functions”, “b620 Bladder functions” and “b730 Muscle power functions” (below the level of lesion). Most of the patients presented additional problems in “b134 Sleep functions” and “b152 Emotional functions” potentially related to the traumatic experience from the earthquake. “b280 Pain” and, in particular, neuropathic pain, existed in almost all patients. Also, the number of persons having impairments in “s810 Structure of areas of skin” related to still-existing pressure ulcers was quite high. “s430 Structures of the respiratory system” and “s610 Structures of the urinary system” could not be assessed due to lack of technical equipment to perform more sophisticated investigations.
| Table II. Description of the extent of problems in functioning in the patients (n = 18) |
| | 0 No impairment | 1 Some impairment | 2 Complete impairment | 8 Not specified | 9 Not applicable |
| b134C | Sleep function | 7 | 10 | 1 | | |
| b152a,b | Emotional functions | 4 | 14 | | | |
| b280a,b | Sensation of pain | 1 | 17 | | | |
| b4401 | Respiration functions | 17 | 1 | | | |
| b525a,b | Defecation functions | 1 | | 17 | | |
| b620a,b | Urination functions | 1 | | 17 | | |
| b640b | Sexual functions | | | 16 | 2 | |
| b710b | Mobility of joint functions | 14 | 4 | | | |
| b730a,b | Muscle power functions | | 5 | 13 | | |
| b735a,b | Muscle tone functions | 14 | 4 | | | |
| b810a,b | Protective functions of the skin | 8 | 10 | | | |
| Body Structures | 0 No impairment | 1 Some impairment | 2 Complete impairment | 8 Not specified | 9 Not applicable |
| s120a,b | Spinal cord and related structures | | 5 | 13 | | |
| s430a,b | Structure of respiratory system | | | | 18 | |
| s610a,b | Structure of urinary system | | | | 18 | |
| s810b | Structure of areas of the skin | 8 | 10 | | | |
| Activities and Participation | 0 No difficulty | 1 Some difficulty | 2 Complete difficulty | 8 Not specified | 9 Not applicable |
| d230b | Carrying out daily routine | Performance | | 12 | 5 | 1 | |
| Capacity | | 12 | 5 | 1 | |
| d240b | Handling stress and other psychological demands | Performance | 5 | 12 | | 1 | |
| Capacity | 5 | 12 | | 1 | |
| d410a,b | Changing basic body positions | Performance | 8 | 9 | 1 | | |
| Capacity | 7 | 6 | 5 | | |
| d420a,b | Transferring oneself | Performance | 7 | 10 | 1 | | |
| Capacity | 7 | 6 | 5 | | |
| d445a,b | Hand and arm use | Performance | 17 | 1 | | | |
| Capacity | 17 | 1 | | | |
| d450a | Walking | Performance | | 3 | 15 | | |
| Capacity | | 2 | 16 | | |
| d455b | Moving around | Performance | | 1 | 17 | | |
| Capacity | | | 18 | | |
| d465b | Moving around using equipment | Performance | | 16 | | | 2 |
| Capacity | 1 | 15 | | | 2 |
| d470b | Using transportation | Performance | | 2 | 16 | | |
| Capacity | | 1 | 17 | | |
| d510a | Washing oneself | Performance | 9 | 8 | 1 | | |
| Capacity | 1 | 16 | 1 | | |
| d520b | Caring for body parts | Performance | 9 | 8 | 1 | | |
| Capacity | 1 | 16 | 1 | | |
| d530a,b | Toileting | Performance | 1 | 12 | 4 | 1 | |
| Capacity | 1 | 1 | 15 | 1 | |
| d540a | Dressing | Performance | 8 | 10 | | | |
| Capacity | 1 | 16 | 1 | | |
| d550a,b | Eating | Performance | 17 | 1 | | | |
| Capacity | 17 | 1 | | | |
| d560a | Drinking | Performance | 18 | | | | |
| Capacity | 17 | 1 | | | |
| d760c | Family relationships | Performance | 1 | 12 | 4 | 1 | |
| Capacity | 1 | 13 | 3 | 1 | |
| d850c | Remunerative employment | Performance | | | 18 | | |
| Capacity | | | 18 | | |
| Environmental factors | +2 Complete facilitator | +1 Some facilitator | 0 No facilitator/barrier | 1 Some barrier | 2 Complete barrier | 8 Not specified | 9 Not applicable |
| e110b | Products or substances for personal consumption | | 18 | | | | | |
| e115a,b | Products and technology for personal use in daily living | | 18 | | | | | |
| e120a,b | Products and technology for personal indoor and outdoor mobility and transportation | 1 | 17 | | | | | |
| e150b | Design, construction and building products and technology of buildings for public use | | | | 1 | 17 | | |
| e155b | Design, construction and building products and technology for private use | | | | 4 | 14 | | |
| e310a,b | Immediate family | 12 | 1 | | | 5 | | |
| e340a,b | Personal care providers and personal assistants | | | | | | | 18 |
| e355a,b | Health professionals | | 18 | | | | | |
| e580b | Health service, systems and policies | | | | | 18 | | |
| aICF categories contained in the Brief ICF Core Set for SCI in the early post-acute context (13). bICF categories contained in the Brief ICF Core Set for SCI in the long-term context (14). cICF categories selected from the Comprehensive ICF Core Sets for SCI (13, 14). ICF: International Classification of Functioning, Disability and Health; SCI: spinal cord injury; Performance: individual’s actions in the actual environment including assistance and the use of devices; Capacity: individual’s ability to execute a task without assistance and/or device (10). |
In the “Activities and Participation” domain, nearly all patients showed complete problems in “d450 Walking” and “d455 Moving around”. These limitations were closely related to the impairments in body functions. However, in the activities “d470 Using transportation” and “d465 Moving around using equipment” that are also related to mobility the environment had a major impact on these limitations, since the area around the hospital and existing transportation services were not wheelchair accessible. With “d530 Toileting”, the facilitating role of an environmental factor can be illustrated in terms of the difference between rating in capacity and performance: without assistive devices such as catheters, toileting would have presented a complete problem in most of the patients. During their hospital stay, patients received these products. Thus, the problem was rated only as “moderate” in terms of performance. “d850 Remunerative employment” was rated as a complete problem in all patients.
Environmental factors were identified as facilitators in the provision of products (e110, e115, e120) and availability of health professionals (e355). The immediate family (e310) supported most of the patients at least partially. Some patients, however, had no family member who survived the earthquake, or had family members were not able to stay at the hospital to support them. With respect to accessibility of public buildings (e150), the environment presented a complete barrier for all of the patients who became wheelchair users. In addition, most of the patients’ houses (e155) had been completely destroyed in the earthquake and, as a consequence, they had nowhere to stay after discharge from the facility. “e580 Health services, systems and policies” was rated as a complete barrier since the Haitian government had not provided rehabilitation services so far.
Rehabilitation needs
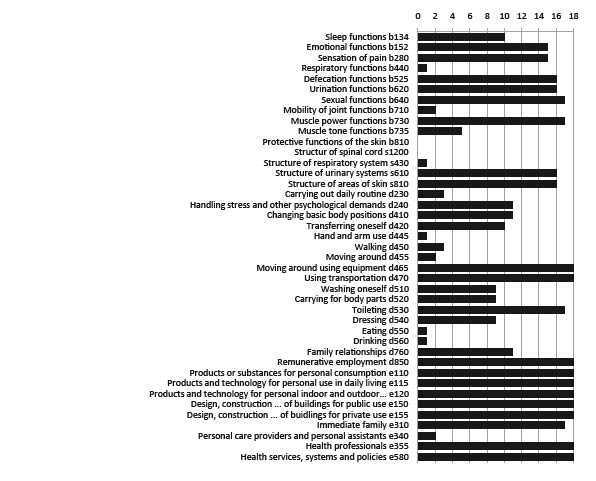
The distribution of rehabilitation needs in each aspect of functioning is presented in Fig. 2. This overview highlights the comprehensive needs of this population in nearly all aspects of functioning for acute and long-term rehabilitation interventions. Most importantly, it highlights the need to intervene not only at the level of the individual’s problems in functioning, but also at the level of environmental factors in order to improve functioning, and, in particular, community integration.
Fig. 2. Distribution of rehabilitation needs in aspects of functioning.
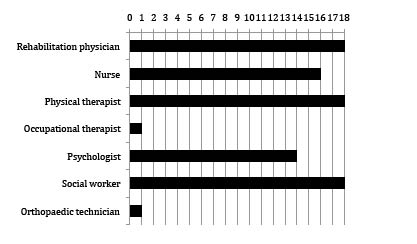
The demand for comprehensive rehabilitation was also reflected in the large spectrum of health professionals that would be needed (Fig. 3). All patients required a rehabilitation physician to address specific symptoms and to prescribe specific medication and therapies. Most of the patients required nursing care, in particular wound care, instruction for catheterization and, in some cases, support in self-care and mobility-related tasks. Physical therapy was necessary in all patients. Major areas included improvement of muscle power and mobility-related activities, in particular moving around with the wheelchair or walking in the patients with incomplete lesions. Interventions regarding self-care activities were performed by the nurses, physiotherapist and by family members. Only the patient with tetraplegia required specific interventions provided by the occupational therapist, such as the adaptation of the wheelchair and provision of splints for the hands and additional assistive devices. Psychological support was judged to be just as important in most patients, in particular to detect potential post-traumatic stress disorder. Moreover, social workers would be most important to all patients to clarify issues regarding future housing and employment. However, neither psychologists nor social workers were available.
Fig. 3. Needs for specific health professionals.
Discussion
This study addressed rehabilitation needs in persons with SCI caused by the 2010 earthquake in Haiti. The importance of rapid assessment tools to identify rehabilitation needs during the immediate phase after disasters had been recognized by previous studies (8, 24). For the provision of rehabilitative interventions, respective needs assessments tools were found to be still lacking. This pilot study illustrates a first attempt in the application of an ICF-based tool.
Utilization of the International Spinal Cord Injury Core Data Set and ICF Core Sets for Spinal Cord Injury
The diagnosis-specific information collected within the International Spinal Cord Injury Data Set provided information regarding the type of injury and sociodemographic characteristics. This information allows comparison between “regular SCI populations” and those from natural disasters. In this study population, only 1 of 17 persons had tetraplegia. In “regular SCI populations” this proportion is estimated as one-third (25). The question remains as to whether a smaller overall proportion of persons acquired tetraplegia or whether those with severe SCI did not survive the early phase after the earthquake. In addition, the distribution of men and women was the inverse of what is usually found (25). Gender-related information is important, since women still experience health disparities following disasters (26).
A comprehensive approach is essential to address the multidimensionality of disability when establishing a rehabilitation strategy (6). The utilization of the ICF Core Sets for SCI facilitated not only a comprehensive, but also an evidence-based, approach in the description of functioning (10). Using the Brief ICF Core Sets including 41 ICF categories facilitated a quick, but still multidimensional, assessment. The selection of 3 additional ICF categories from the Comprehensive ICF Core Set was deemed necessary to add specific aspects of functioning relevant to this particular SCI population. “b134 Sleep functions” are frequently impaired following traumatic events and were expected to be also impaired in this population. “d760 Family relationships” play an important role regarding care provision in developing countries and furthermore, were likely to be restricted due to displacement following the earthquake. Finally, “d850 Remunerative employment” plays an important role for community reintegration and, most importantly, for economic self-sufficiency and hence, was likely to require rehabilitative interventions. However, this selection was performed only on the basis of expert opinion and thus lacks scientific evidence. Some additional important life areas, such as “recreation and leisure” or “religion and spirituality”, were not covered. They were not included in the Brief ICF Core Sets, nor, for pragmatic reasons, did we decide to add them. Hence, relevant information may be missing in this assessment. The development of particular ICF Core Sets for assessment of rehabilitation needs following natural disasters either relating to specific health conditions or a generic set of ICF categories that is applicable across health conditions represents a potential task for future research.
Identification of problems and associated rehabilitation needs using the ICF
The use of the enlarged Brief ICF Core Sets for SCI facilitated the identification of rehabilitation needs in all components of functioning and environmental factors. The identified impairments in body functions and body structures and the limitations in the patients’ capacity to perform tasks would require therapeutic interventions. However, the identified restrictions in the patients’ performance would require additional adaptations in the environment. The impact of environmental factors on functioning in persons with SCI was immense, both positive and negative. While devices for toileting, walking and wheelchair mobility, provided by HHA and other NGOs, and the immediate family members presented important facilitators, the physical environment and the lack of a health and social security system presented barriers to current and future improvements in functioning. This finding stresses the need to act on environmental factors and, at the same time, depicts challenges that persons with disabilities face in low-resource countries, such as Haiti, regarding health service provision and accessibility in general (27).
Multidisciplinary approaches are required in order to address all of these needs. These should integrate medical professionals, such as physiatrists, nurses, physical and occupational therapists, and psychologists, as well as non-medical professionals, such as social workers, architects and city planners. Without such approaches, community integration is severely hampered, as is well-known from low-resource settings (28). This rehabilitation needs assessment contributed to the generation of data for multidisciplinary rehabilitation planning.
Usage of information
The information gathered with this approach will, however, contribute to the provision or development of rehabilitation services only if it is actually used by service providers and local or national health policy makers. In countries without established rehabilitation services (as it is the case in Haiti and many other low-resource countries), assessments are frequently performed by international NGOs who play an important role in service provision, in particular in the early aftermath of natural disasters (29). The application of instruments such as the one presented here may contribute to a more comprehensive understanding of disability across all levels and settings (30).
Limitations
In this pilot study, needs assessment was performed by an expatriate rehabilitation team with experience in SCI rehabilitation. In Haiti, as is the case in many other low-resource countries, a few trained rehabilitation doctors and nurses may be available, but physical or occupational therapists, psychologists and social workers are not. SCI specialists are crucially lacking. Hence, it is indispensible to enable local staff to perform assessments, education and training in rehabilitation management.
This needs assessment was performed in only 18 persons with SCI, who were admitted to the rehabilitation centre more or less randomly. Hence, the data may not be representative for all persons with from SCI after the earthquake. If data from larger samples became available in the future (e.g. from all persons with SCI following a specific disaster event), such needs assessments could provide more reliable information to service providers and thus better contribute to adequate resource allocation.
Conclusion
Natural disasters present immense challenges to the provision of adequate services. This pilot study represents a first attempt to develop a rehabilitation needs assessment tool based on the ICF to be used after natural disasters. Future studies are required to test and, if necessary, adapt this tool to other settings. In particular, its applicability by newly trained rehabilitation aides or professionals needs to be evaluated.
AcknowledgementS
The authors thank all participating patients and the local HHA staff members and leaders, in particular Fiona Stephenson (leading nurse), Lisa Carnie (physical therapist volunteer) and Jn Robert Joseph (translator) for their collaboration, as well as the organization Healing Hands for Haiti (HHH) under the lead of Colleen O’Connell for their organizational support. Furthermore, Sibille Bühlmann, Christa Schwager and Carine Steger from the team of Swiss Paraplegic Center are acknowledged for their valuable support during the work in Haiti.
REFERENCES