OBJECTIVE: To determine upper limb function and associated factors in adults with Duchenne muscular dystrophy.
DESIGN: Cross-sectional study.
SUBJECTS: A sample of 70 men with Duchenne muscular dystrophy (age range 20–43 years).
METHODS: General motor function and, in particular, upper limb distal motor function, were assessed with the Motor Function Measure. Muscle strength and range of motion of the upper limb were evaluated using hand-held dynamometry, manual muscle-testing and goniometry. Associations were studied using Spearman’s correlation coefficients and multiple linear regression analysis.
RESULTS: General motor function was severely impaired. Wide variability was found in distal motor function, muscle strength and range of motion of the upper limb, especially in early adulthood. Muscle strength and range of motion explained 76% of the variance in upper limb distal motor function.
CONCLUSION: This study illustrates a large variability in upper limb function in adult patients with Duchenne muscular dystrophy, and identifies muscle strength and range of motion as factors strongly associated with upper limb function. These results suggest that preserving muscle strength and range of motion in Duchenne patients might be relevant for a better outcome of distal motor function of the upper limb when adult.
Key words: Duchenne muscular dystrophy; adults; upper limb function; Motor Function Measure; muscle strength; range of motion.
J Rehabil Med 2011; 00: 00–00
Guarantor: Robert Pangalila, Erasmus University Medical Center, Department of Rehabilitation Medicine and Physical Therapy, PO Box 2040, NL-3000 CA Rotterdam, The Netherlands. E-mail: r.pangalila@erasmusmc.nl
Submitted January 9, 2011; accepted May 18, 2011
Introduction
Duchenne muscular dystrophy (DMD ) is an X-linked recessive neuromuscular disease diagnosed in childhood, with an incidence of 1/3500 living male births (1). The absence of dystrophin causes progressive weakness of skeletal, respiratory and cardiac muscles, and leads to severe physical disability and a shortened life expectancy. Long-term survival has improved substantially in the last two decades, due to improvements in care and the introduction of home ventilation. Where the mean age of survival in 1980 was approximately 20 years, a recent study estimated median age of survival to be 30 years (2) and another study 35 years, with an estimated probability of survival to age 30 years of 85% (3). As a result, there is now a considerable group of adult patients with DMD living with severe physical impairments and a strong dependency on care (4).
As the distal muscle groups of the upper extremities are those best preserved in patients with advanced DMD, upper limb activities are especially meaningful in daily life (5). Studies have shown that adult patients with DMD are still able to perform important functional activities with limited distal motor function, but tend to lose this capacity if muscle strength diminishes only slightly (6, 7). Until now the level of distal motor function still present in the adult population has been unknown. We therefore conducted a cross-sectional study on adult patients with DMD to determine distal motor function of the upper limb. Further insight into upper limb function and associated motor impairments in adulthood may contribute to our knowledge of the functional prognosis of DMD.
PATIENTS AND METHODS
Recruitment
This study is part of a larger cross-sectional study on functioning, quality of life and healthcare needs for adults with DMD and their informal caregivers, performed over the period 2006–2010 in the Netherlands. Patients were recruited through the 4 Centers for Home Ventilation in the Netherlands, rehabilitation centres and the Dutch patient organization for neuromuscular diseases (VSN). Inclusion criteria were a diagnosis of DMD and an age of at least 20 years. As at this age almost all patients are ventilator-dependent and therefore known to the Centers for Home Ventilation, and since almost all patients with DMD in the Netherlands are referred to rehabilitation care, we believe we have identified virtually the entire population of adults with DMD in the Netherlands. A total of 151 people were invited to participate in the entire study and 80 agreed. Upper limb function of the first 72 patients who were included in the entire study was measured in terms of functioning, quality of life and healthcare needs for adults with DMD and their informal caregivers. Because of a large delay in inclusion of the last 8 patients they did not participate in this specific study on upper limb function. Patients had been diagnosed on clinical grounds before DNA analysis or Western blot were available. Where possible, we retrospectively applied the diagnostic criteria according to Emery for diagnosis (8). We eventually excluded two patients because, retrospectively, they did not meet the diagnostic criteria regarding age of ambulation loss. The majority of patients, but not all, had had DNA analysis at a later stage; in 18 patients there was no DNA confirmation of diagnosis. For these we accepted the clinical diagnosis.
Of the non-participants, 7 persons indicated that participation was too burdensome. The study sample and non-responders did not differ in terms of age and ventilation type; therefore, the study sample was assumed to be representative. The Erasmus University Medical Center Ethical Review Committee approved the study protocol. All the participants provided their informed consent to participate.
Characteristics
Seventy Dutch adults with DMD (mean age 27.6 years, standard deviation (SD) 6.1, range 20–42) participated in this study. Almost all the patients used home ventilation (97%) and 50% of these ventilated patients were tracheostomized. Most of the patients used a powered wheelchair (95%). Retrospectively, participants indicated a mean age for loss of ambulation of 9.1 years (SD 1.3, range 6–12), which corresponded with previous studies (3, 9). None of the participants had used steroids in the past or were using steroids at the time of the measurements.
Measurements
Measurements were performed at home, during 2 sessions on different days in order to reduce the burden on the participants to a minimum. To avoid bias caused by a further decline in motor function over the time period, measurements were planned with no more than a 30-day interval (10). In 94% of the participants, measurements were performed within the predetermined period of 30 days. The longest period in between measurements was 43 days, which was caused by sudden illness of the participant between planned measurements. One physical therapist (BB) with several years of experience assessing patients with DMD performed the measurements. He performed assessments of motor function, muscle strength and range of motion (ROM) of the upper limb in a fixed order.
Motor function. Motor function was assessed using the Motor Function Measure (MFM). The MFM provides a standardized assessment of the motor capacity of a subject with a neuromuscular disorder. It is validated for persons with DMD, among other neuromuscular diseases, and is adapted for both children and adults. The test includes 32 items and refers to 3 dimensions. D1: Standing and transfers (13 items); the patient is asked, for example, to stand up from a chair without support. D2: Axial and proximal motor function (12 items); the patient, for example, is placed in a supine position, and asked to raise and hold his head in flexion for 5 s. D3: Distal motor function (7 items of which 6 items refer to the upper limb); the patient is, for example, asked to draw loops with a pencil. Each item is scored on a 4-point scale (0–3); a higher score corresponds to a better performance. MFM total score was calculated as a percentage of the maximum possible score following standard scoring procedures, as described by Berard et al. (11).
In order to measure distal motor function of the upper limb specifically, we excluded Item 4 (movement of the ankle) from the MFM dimension 3, and further indicated this score as the MFM D3 Upper Limb score. Most of the participants were not able to select a dominant side as they were using both sides equally for different purposes, for example driving a powered wheelchair with 1 hand and managing an environmental control system with the other. Therefore we selected the best scoring side to calculate MFM D3 Upper limb score and further indicated this side as the “best side” in all analyses. MFM D3 Upper limb score was calculated as a percentage of the maximum possible score. MFM total score (%) and MFM D3 Upper limb score (%) were used for further analysis.
Muscle strength. We determined the strength of 8 selected muscle groups for both arms (flexion and abduction of the shoulder, flexion and extension of the elbow, flexion and extension of the wrist, adduction of the thumb, and flexion of the index finger) using the Medical Research Council (MRC) scale for manual muscle testing (12). MRC scores were dichotomized into “1” (MRC ≥ 3) and “0” (MRC < 3). An overall sum score was calculated for each side, addressing the number of non-impaired muscles (0–8 muscles), with a higher score indicating less impairment in muscle strength of the upper limb. The sum score of the dominant arm was used for further analysis. In addition, quantitative muscle tests of wrist extension and thumb adduction were performed in participants with MRC values ≥ 3. Patients below this criterion had a score of 0 Newton on both measurements. Wrist extension was measured with a hand-held dynamometer (type Microfet2, Biometrics Europe BV, Almere, The Netherlands) by using the break method with a 30-s interval (13). Measurement protocol was adjusted for this population: supine position, shoulder adducted, along with elbow in 90-degree flexion and wrist in neutral position. The dynamometer was positioned just distal from the third carpal-metacarpal joint. Thumb adduction was measured with the Rotterdam Intrinsic Hand Myometer (RIHM) (14). The measurement protocol was adjusted for this population: position seated in the wheelchair, lower arm resting on the table and in a 90º prone position, the wrist in neutral position, and the thumb adducted against the radial side of the index finger. The leather band of the RIHM was positioned just distal from the metacarpal-phalange joint and pulled towards abduction. A mean score calculated from 3 measurements of the predetermined best side was used for further analysis of both wrist extension and thumb adduction.
Range of motion. Passive ROM of 4 joints in 12 selected directions on both sides was assessed through goniometric measurements (Appendix I) (15). Placing the wrist joint in maximum flexion or extension eliminated the effects of extrinsic flexor and extensor tightness on the ROM of the thumb and index finger. Measured angles were converted into percentages of motion impairment of the corresponding joints and dichotomized into no ROM impairment “1” (< 10% motion unit impairment) and impaired ROM “0” (≥ 10% motion unit impairment). The cut-off point was chosen in accordance with the American Medical Association (AMA) guide (16). An overall sum score was calculated for each side, summarizing the number of non-impaired movements (0–12 movements). Higher scores indicated less impairment in the ROM of the upper limb. The overall sum score of the predetermined best side was used for further analysis.
Statistical analysis
Statistical analyses were performed using SPSS Version 16.0 (SPSS Inc., Chicago, IL, USA).
Results for distal motor function, muscle strength and ROM of the upper limb are presented as median and range. Differences in distal motor function, muscle strength and ROM between the best side and the other side were tested with the Wilcoxon’s signed-rank test. Interrelationships between motor function, muscle strength, ROM and age were estimated with Spearman’s correlation coefficient (rs). Multiple linear regression analysis was carried out for motor function of the upper limb, exploring muscle strength, ROM and age as independent variables. We present the standardized regression coefficients (β) and explained variance (R²) of the regression model. For all tests, the significance level was set at 0.05.
Results
General motor function (MFM total score) was severely impaired in all adult patients with DMD (Table I); 18% of the men obtained no positive score and only 11% of the men exceeded a score above 20% of maximum score. Differences in levels of general motor function were mainly caused by a large variability in distal motor function of the upper limb (Fig. 1). Twenty-one percent of the men obtained a MFM D3 upper limb score of 50% or higher, while 23% obtained no positive scores at all. Overall, the MFM D3 upper limb items demanding less proximal involvement of the upper limb were performed better (Fig. 2). Within participants, the difference in MFM D3 upper limb score between upper limb sides was significant, but relatively small (median difference of 6% in favour of the best side, p < 0.001), which might explain the difficulty the participants experienced in selecting a dominant hand.
All participants had severe muscle weakness of the upper limb; none of them was able to lift their arms against gravity (abduction and flexion of the shoulder: MRC < 3). However, the extent to which the muscles of the upper limb were affected varied greatly. Seven percent of the men could still raise their lower arms (overall strength 6), while 37% could only lift their hands against gravity (overall strength score 4). The ability to overcome any moment of gravity was lost in 27% of the men (strength score 0). Quantative muscle tests showed a large variability in muscle strength of the wrist extension (range = 0–79 N) and thumb adduction (range = 0–53 N). The participants showed severe muscle weakness of wrist extension in comparison to reference values (13) (Table I). In general, distal muscle groups were less affected than proximal muscle groups; flexion of the index finger and adduction of the thumb were the two best preserved functions (MRC ≥ 3 in 51% of the participants). Flexion and abduction of the shoulder were the most severely affected (MRC ≥ 3 in 0% of the participants). In all participants, passive ROM of the upper limb was impaired. The number of affected joints, however, varied largely. In 58% of the men ≥ 6 out of 12 selected joint directions were impaired.
| Table I. Descriptive results of motor function, muscle strength and range of motion | |||
| Median | Range | Reference values | |
| MFM total score (%)a | 5 | 0–32 | 100% |
| MFM D3 upper limb score (%)a | 17 | 0–88 | 100% |
| Overall muscle strength upper limbb | 2 | 0–6 | 8 |
| Wrist extension (Newton) | 0 | 0–79 | 170 |
| Thumb adduction (Newton) | 5 | 0–53 | – |
| Range of motion upper limbc | 6 | 2–12 | 12 |
| aScore expressed as a percentage of the maximal possible score. bNumber of muscle groups with Medical Research Council scale (MRC) ≥ 3 out of 8 selected muscle groups. cNumber of directions not impaired out of 12 selected joint motions. MFM: Motor Function Measure. | |||
In 10% of the men ≤ 2 selected joint directions were impaired. In this population, most of the men had loss of supination of the lower arm (83%) and extension of the wrist (77%). Relatively few men had loss of flexion (24%) and extension (31%) of the second metacarpal joint. The sum scores of muscle strength and ROM of the upper limb did not differ between sides.
Correlations with age and parameters of upper limb function
We found only a weak to moderate correlation between age and distal motor function of the upper limb (rs = 0.44); the large variability is found predominantly between 20 and 30 years of age. In the older group there are no individuals who have preserved a good distal motor function (Fig. 1). We observed a strong correlation between distal motor function and overall muscle strength of the upper limb (Fig. 3A). Distal motor function of the upper limb was moderately correlated to ROM of the upper limb (rs=0.64), thumb adduction strength (rs=0.73) and wrist extension strength (rs=0.63) (Fig. 3B). All correlations were significant. A regression model demonstrated that 76% of the variance in distal motor function of the upper limb was explained by overall muscle strength and ROM of the upper limb.
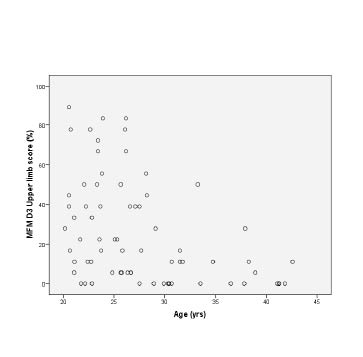
Fig. 1. Age and distal motor function of the upper limb (MFM D3 upper limb score) as a percentage of the maximal score.
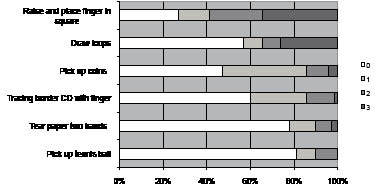
Fig. 2. Item scores MFM D3 upper limb score. Percentage of participants are shown. 0: cannot initiate task; 1: partially performs task; 2: performs task incompletely or completely but imperfectly; 3: performs task fully and normally.
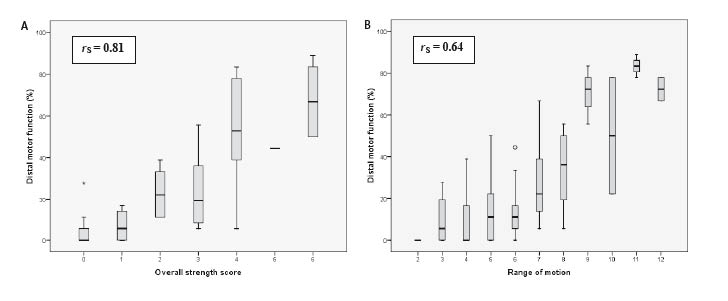
Fig. 3. Relationship between (A) overall muscle strength and distal motor function of the upper limb, (B) and overall range of motion and distal motor function of the upper limb box-plots depict median score (—), interquartile range (grey) and minimum and maximum values (whiskers); *show outlier. rS=Spearman’s correlation coefficient.
Distal motor function: motor function measure D3 upper limb score. Overall strength score: number of non-impaired muscles.
Discussion
This cross-sectional study demonstrates a large variability of upper limb function in adult patients with DMD in terms of distal motor function, muscle strength and ROM.
Brooke et al. (17) demonstrated a large variability in lower and upper limb function in 114 paediatric DMD patients. Along with loss of ambulation, variability in lower limb function is generally lost in adulthood. The present results, however, show that variability in upper limb function is maintained in adulthood, especially in earlier adulthood. In agreement with the results of Berard et al. (11), in some of the severely affected DMD patients we observed a high level of distal motor function of the upper limb, reflected in a good performance on “Dimension 3 upper limb” of the MFM. The difference between the least affected (best) side and the most affected side per individual was relatively small at the group level. This study also shows that at this advanced stage of the disease, the MFM D3 Upper Limb score is capable of differentiating between individuals with some residual distal upper limb function. For patients with very minimal upper limb function, however, this score does not identify the last residues of motor function, which are of great importance for the performance of patients. In these patients, remaining distal upper limb function generally consists of isolated finger movements, such as flexion of the index finger and adduction of the thumb. Given that these isolated finger movements can be essential for successfully manipulating assistive devices while performing activities of daily living, it might be more relevant to differentiate within this group of patients by evaluating distal motor function parameters, such as muscle strength and ROM of the hand. Since there are no reference values available for thumb adduction strength it was not possible to compare the adult patients with DMD with healthy controls. For abduction of the thumb, Schreuders et al. (18) demonstrated in patients with median or ulnar nerve injury that strength values of 20 N or lower correspond to a grade 3 or less on the MRC scale. The findings in thumb adduction (range 0–59 N, median 5 N) suggest that most of our participants have severe muscle weakness of the thumb adduction, but also that some participants still have moderate strength of the thumb adduction. In contrast to our results, Pelligrini et al. (7) found consistently low values of key pinch strength in adult patients with DMD. However, these patients were selected based on poor hand function (Brooke score ≥ 5) and should therefore not be compared with our participants.
Mattar & Sobreira (19) reported a significant correlation between hand strength and physical capacity of the upper limb in paediatric DMD patients older than 10 years, and Wagner et al. (20) demonstrated similar correlations between muscle strength of wrist extension and 6 items of the Jebsen Hand Function Test. Our study demonstrates similar correlations between muscle strength and motor function in the adult population, thus extending the knowledge about these correlations to older patients.
To assess motor impairments of the upper limb, we selected reference muscle groups and joint motions, dichotomized these values and created sum scores. In order to calculate a sum score of muscle strength, we dichotomized the MRC scores using the clinically relevant cut-off point at MRC Grade 3. Although muscle groups with an MRC Grade 2 may contribute to activity performance to a small extent, at Grade 3 muscles are just strong enough to provide a full ROM in the joints they cross. Grade 3 is easily and reliably assessed and has been defined as good motor outcome (21). By dichotomizing our data we were able to differentiate easily between minimum and medium levels of muscle strength and create a summary score (“overall strength upper limb” score) that reflects the general muscle strength of the upper limb in adults with DMD.
In addition, we performed quantitative muscle testing of wrist extension and thumb adduction to investigate the relationship between specific muscle groups with motor function
For ROM measurements a similar approach was used (22). On principle, ROM expressed in degrees is an interval scale and is therefore suitable for parametric statistics. However, given that the ROM of a particular joint is not linearly related to motor function we did not know the individual’s contribution of a specific joint direction to a particular movement of the upper limb. Therefore, by dichotomizing our data into no ROM impairment vs ROM impairment we were able to calculate a summary score that reflects the level of ROM impairment of the upper limb in adults with DMD. By dichotomizing the data on ROM we were no longer able to differentiate between moderately and severely impaired joints, but we could differentiate between individuals regarding the amount of impaired joints.
In the literature, until now, intervention programmes have focused mainly on improving and maintaining ambulation in children with DMD. With an ongoing improvement in life expectancy, however, upper limb function also deserves specific attention in rehabilitation programmes and research. By showing strong relationships between muscle strength, ROM and distal motor function of the upper limb, this study suggests the importance of maintaining adequate levels of muscle strength and ROM of the upper extremity, with the long-term goal of preserving distal motor function of the upper limb. The role of intervention programmes, such as resistance training, in the management of muscular dystrophy is still a matter of debate in the literature because of the possible adverse effects on the integrity of the muscles involved. However, several authors have shown that resistance and endurance training can be performed safely in other muscular dystrophies, such as Becker dystrophy and facioscapulohumeral muscular dystrophy (23, 24). Although these results cannot be automatically transferred to the DMD population because of differences in origin and severity of the pathology, they do show that damaged muscles can be trained to some extent without adverse effects. Considering the importance of upper limb function in the adult life of DMD patients, it is advisable to investigate the possible long-term effects of such training programmes on muscle strength and joint motion in DMD patients. Interventions should preferably begin in the ambulatory period when functional ability of the upper extremity has not yet been affected (20).
In conclusion, this study illustrates a large variability in upper limb function in adult patients with DMD, and identifies muscle strength and ROM as factors strongly associated with upper limb function. Our results suggest that preserving muscle strength and ROM in persons with DMD might be relevant for a better outcome of upper limb function in adulthood.
AcknowledgementS
This work was supported by grants from the Foundation Rotterdam Children’s Rehabilitation Fund Adriaan-Stichting (KFA Grant Number 2005/0143), Johanna Children’s Fund (JKF Grant Number 2005/0143) and The Nuts-Ohra Foundation (Grant Number SNO-T-0701-85).
The authors wish to thank the Home Ventilation Centers of the University Hospitals of Rotterdam (J. Rischen-Vos, MD), Utrecht (M. J. Kampelmacher, MD, PhD), Groningen (P. J. Wijkstra, MD, PhD) and Maastricht (N. A. M. Cobben, MD, PhD) for their support in recruiting the participants in this study.
References


