Ann-Sofi Lamberg, RPT, MSc1 and Jan Fridén, MD, PhD2
From the Departments of 1Physical Therapy and 2Hand Surgery, Institute of Clinical Sciences, The Sahlgrenska
Academy at Göteborg University, Göteborg, Sweden
Ann-Sofi Lamberg, RPT, MSc1 and Jan Fridén, MD, PhD2
From the Departments of 1Physical Therapy and 2Hand Surgery, Institute of Clinical Sciences, The Sahlgrenska
Academy at Göteborg University, Göteborg, Sweden
OBJECTIVE: The aim of this study was to document prospectively the changes in function that can affect the skills required to use a manual wheelchair after reconstructive hand and arm surgery in individuals with tetraplegia.
DESIGN: Case series. The tests were conducted preoperatively and 12 months postoperatively.
Patients: Sixteen individuals who underwent a total of 23 grip/elbow extension reconstructions and who used a manual wheelchair as their main form of transport were included.
METHODS: Functional tests of wheelchair control were performed. The tests addressed 8 aspects of manoeuvring a wheelchair.
RESULTS: Sixty-eight percent of the individuals improved their manoeuvring skills after hand surgery. Improvements were also observed in the ability successfully to perform tests that were impossible to perform before surgery. The type of reconstruction and level of injury affected the outcome.
CONCLUSION: The improvement in wheelchair propulsion ability after reconstructive hand and arm surgery in individuals with tetraplegic spinal cord injury implies increased mobility, which can help individuals to live a more active life.
Key words: spinal cord injuries; tetraplegia; hand surgery, wheelchair manoeuvrability.
J Rehabil Med 2011; 43: 714–719
Correspondence address: Jan Fridén, Department of Hand Surgery, Sahlgrenska University Hospital, SE-413 45 Göteborg, Sweden. E-mail: jan.friden@orthop.gu.se
Submitted January 7, 2011; accepted May 18, 2011
INTRODUCTION
The return of arm and hand function is by far the most important priority to improve quality of life among individuals with tetraplegia (1). This is the case both during the early stages of spinal cord injury and later (> 3 years post-injury). Physical function and independence have been demonstrated to affect quality of life of persons with tetraplegia to a greater extent than those with paraplegia (2). Limited hand function, such as impaired function in mobility, activities in daily life and writing, have been identified as decreasing physical function.
Surgical reconstruction of arm and hand function has developed tremendously over the last decade, and several studies have documented the beneficial effects of reconstructive hand surgery in individuals with tetraplegia. Functional improvements after surgery and rehabilitation usually include better control and strength of elbow extensors, lateral pinch, grip function and opening of the hand (3–6). Improvements in activities of daily living and independence have also been documented, with increased ability to perform more activities and less need for adaptive equipment after hand surgery (7, 8).
Regained ability of individuals in daily life to increase their voluntary control of transfers to and from a wheelchair, as well as improved propulsion capacity of a manual wheelchair are listed as main goals before reconstructive surgery (9). It has been shown that the level of spinal cord injury affects the velocity and cycle distance. Persons with tetraplegia were slower and travelled shorter distances per cycle than those with paraplegia. There was also a difference between the C6 tetraplegia group and the C7 group, where the C6 group had a significantly shorter cycle distance than the C7 group (10). The current study was initiated to document prospectively the changes in function that can affect the skills required to use a manual wheelchair after reconstructive hand and arm surgery in individuals with complete spinal cord injury and tetraplegia (11). The study was designed to address various skills required to use and manoeuvre a manual wheelchair in daily life, i.e. sprint, driving along courses with turns, static forward push of the wheelchair driving wheel, unloading of the buttocks, driving uphill on a ramp and driving over rim. It was also of interest to determine whether the reconstructive surgery had any effect on the angle between grip and release of the rim during the propulsion cycle.
METHODS
Participants
Persons who used a manual wheelchair as their main form of transport and who used the same wheelchair during the whole test period were included in the study. The test included persons who underwent reconstructive surgery during 2003–2006. The study included 14 men and 2 women, with a mean age at surgery of 33.9 years (age range 19–62 years). Mean age at injury was 26.9 years (age range 17–60 years) (Table I). None of the participants included in the study were trained before or after surgery in any of the activities included in the functional test for manual wheelchairs. This study was approved by the ethics committee of the University of Gothenburg.
Surgical procedures
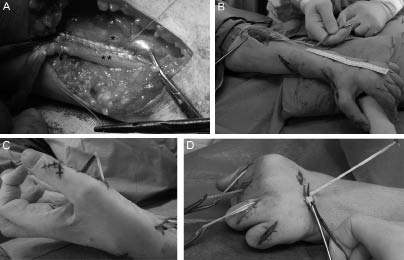
Reconstruction of elbow extension. Triceps function was reconstructed according to established international standards using transfer of posterior deltoid to triceps (12). Briefly, the posterior deltoid border was mobilized and the interval between middle and posterior deltoid identified. A tibialis anterior tendon graft was removed from the lower leg and the distal deltoid tendon was attached to the tendon graft with an overlap of 5 cm and sutured together (Fig. 1A). The distal tendon graft insertion was sutured to the flat triceps tendon. The muscle-tendon unit passive tension was set to a moderate level when the arm was positioned along the body and the elbow extended. After skin closure and wound draping, a circumferential plaster cast was applied, with the elbow flexed 10–15º from full extension.
Reconstruction of grip. This reconstruction typically included muscle-tendon transfers of brachioradialis (Fig 1B) to flexor pollicis longus (FPL) and extensor carpi radialis longus to flexor digitorum profundus, together with split FPL to extensor pollicis longus tenodesis, fusion of the basis of the thumb or transfer of extensor digiti minimi to abductor pollicis brevis (Fig 1C), as well as reconstruction of interossei (Fig. 1D) (for details see 13).
Fig. 1. Surgical procedures commonly used in reconstructive hand surgery in tetraplegia. (A) After attaching the tibialis anterior tendon graft to the posterior deltoid, it is tunnelled subcutaneously and inserted into the original triceps tendon proximal to the elbow joint. A meticulous suture technique is applied to secure the mechanical integrity of the attachment site. The figure shows the TA tendon graft sutured to the triceps tendon with a 5 cm overlap while the elbow joint is kept in full extension. *Triceps tendon, **TA tendon graft. (B) The brachioradialis (BR) muscle is a major donor for replacing, for example, wrist extension and thumb flexion. BR requires extensive mobilization to guarantee maximal excursion during activation. A ruler is used during procedure to measure muscle amplitude. (C) In many C6 injuries, some little finger extension is retained. This remaining function can be utilized by transferring extensor digiti minimi (EDM) muscle as a donor to abductor pollicis brevis (APB) and thus providing palmar abduction of the thumb to increase the opening of hand. The figure shows the EDM tendon brought subcutaneously to insert into the distal tendon of APB. (D) Reconstruction of interossei function is crucial for positioning of the fingers relative to the thumb (key pinch) and also for securing proximal interphalangeal (PIP) joint extension to enable improved opening of the hand. The figure shows tendon grafts brought through the lumbrical canal, thus mimicking the original intrinsic function of metacarpophalangeal joint flexion and PIP extension.
Potential risks
Potential risks during and after reconstructive upper limb surgery in tetraplegia do not differ from soft tissue extremity surgery in other patient groups. In other words, bleeding and infections may occur in rare cases. Two more likely complications are adhesions in the tendon-to-tendon attachment regions that may occur because of inappropriate or insufficient postoperative training, and pressure sores due to non-optimal fitting of the splints. Awareness of these potential complications is necessary among all personnel treating and training the patients after surgery.
Postoperative rehabilitation
Those patients who underwent a transfer of posterior deltoid to triceps, were supplied with a powered wheelchair, which had a special armrest attached, for the first 3 months. The arm was immobilized in a cast for one month and thereafter an adjustable angle orthosis was applied for gradually increasing the flexion of the elbow. These precautions were made to prevent tendon elongation (12). The patients were released from hospital 3 days after surgery. One month later they returned for 5 days to try out the adjustable orthosis and to start to activate their reconstructed elbow extension function and to gradually increase elbow flexion. After 3 months the patients were allowed to begin to propel their manual wheelchairs and after 4 months they were allowed to start with strengthening exercises. Follow-ups were performed 3, 6 and 12 months postoperatively.
Patients who underwent reconstruction of active finger flexion and/or thumb flexion (13) started postoperative training of the reconstructed functions the day after surgery. The goal of this training was to initiate early motor relearning via unloaded activation of the muscles in their new positions. This part of the training required extensive assistance and guidance by an experienced physiotherapist during 4 training sessions per day for 4 weeks. For the first month the hand was immobilized with splints between the training sessions. The patients were allowed to manoeuvre their manual wheelchair indoors with the splints attached to the hand. The patients were released from hospital 3 days after surgery. After one month the patients returned for 5 days of activity and functional training of the hand and they were allowed to start using their hand in daily activities under guidance and surveillance. After 3 months they were allowed to start with strengthening exercises. Follow-ups were performed 2, 3, 6 and 12 months postoperatively.
Measuring procedures
All individuals were examined by the reconstructive hand surgery team, which included surgeon, physiotherapists and occupational therapists before surgery and during the postoperative follow-ups.
Functional tests of wheelchair control
The functional test for manual wheelchair control included 8 different tasks (Test 1–8):
• Test 1. A 25-m wheelchair sprint.
• Test 2. Manoeuvre the wheelchair around a figure-of-eight (6 m).
• Test 3. Propel a wheelchair up a 3 m 1:12 gradient.
• Test 4. Manoeuvre the wheelchair over a 2.5 cm high and 2.5 cm wide rim.
• Test 5. Manoeuvre the wheelchair over a 5 cm high and 5 cm wide rim.
• Test 6. A static forward push of the wheelchair.
• Test 7. A 3-s buttock lift from the wheelchair.
• Test 8. The position of the hand on the rim during wheelchair propulsion.
All tests were performed twice and the best result was recorded. Tests 1–5 were measured using a timekeeper in seconds and with a standing start. Test 6 was measured with a scale attached to the wheelchair via an inelastic webbing strap and then attached to a stationary fixture. The greatest static forward push was recorded in kilograms. Test 7 was measured with a scale placed in the wheelchair and the percentage of seated body weight lifted from the wheelchair was recorded. In test 8, the hand strike position on the wheel was videotaped. The arc between the position of the hand at initial strike of the push and the position at which the hand left the rim was measured in degrees.
The ability to manoeuvre the wheelchair was tested in 16 individuals before surgery and 12 months after reconstructive hand and arm surgery. The patients underwent 23 reconstructive operations, 10 elbow extensor reconstructions and 13 grip reconstructions (Table I).
| Table I. Demographics | |||||||
| Sex | Age at surgery Years | Age at injury Years | Type of injury | International Classification Right/left | Level of injury | ASIA | Triceps grade 0–5 Right/left |
| F | 34 | 30 | Sport | OCu/O | C5–C6 | A | 0/0 |
| M | 19 | 17 | Sport | O/O | C5–C6 | A | 0 |
| M | 50 | 22 | Abuse | OCu/OCu | C6–C7 | A | 5 |
| M | 62 | 60 | Bicycle | OCu/OCu | C5–C6 | B | 2 |
| M | 28 | 25 | Diving | O/OCu | C5–C6 | A | 2 |
| M | 32 | 20 | Diving | OCu/OCu | C6–C7 | B | 5 |
| M | 31 | 21 | Car | O/O | C5–C6 | A | 0/0 |
| M | 29 | 18 | Diving | OCu/OCu | C5 | A | 0 |
| M | 22 | 20 | Diving | OCu/OCu | C7 | A | 5 |
| M | 32 | 26 | Diving | OCu/OCu | C6–C7 | A | 0/4 |
| M | 28 | 28 | Sport | OCu/OCu | C6–C7 | A | 4 |
| M | 30 | 15 | Bicycle | OCu/OCu | C5–C6 | A | 1 |
| M | 55 | 51 | Sport | O/O | C6–C7 | A | 4 |
| M | 31 | 23 | Bicycle | OCu/OCu | C5–C6 | A | 0 |
| M | 21 | 18 | Diving | OCu/OCu | C5–C6 | A | 0 |
| F | 39 | 37 | Car | OCu/OCu | C7 | A | 5 |
| Mean | 33.9 | 26.9 | |||||
| ASIA: American Spinal Injury Association; O: ocular (visual feedback); Cu: cutaneous sensory feedback. | |||||||
Statistical analysis
Statistical analyses were performed using Excel and SPSS (SPSS Inc., Chicago, IL, USA). To analyse the results after each procedure, a paired t-test was performed to compare preoperative results and the 12-months post-operative checkpoint. A p-value of 0.05 was considered significant. Wilcoxon’s signed-rank test was used to compare each individual’s preoperative results with data one year after completed reconstruction, as paired variables. Individuals who did not succeed with the test preoperatively were excluded from the statistical analysis.
RESULTS
Changes in performance after reconstructive surgery
Twenty-three reconstructive surgeries were performed. After 12 months, performance in the 25 m sprint, figure-of-eight, uphill, 2.5 cm rim and static push improved significantly (Table II). Those individuals who did not succeed with the test preoperatively were excluded from the statistical analysis. Out of the 23 individuals tested, 7 succeeded in propelling over a 5 cm rim before the operation (1 elbow and 6 grip reconstructions), although 3 more succeeded after reconstruction (1 elbow and 2 grip reconstructions). Thirteen individuals succeeded in manoeuvring uphill before the operation (4 elbow reconstructions and 9 grip reconstructions) and 2 more succeeded in the test after surgery (1 grip reconstruction and 1 elbow reconstruction).
| Table II. Results of functional test for manual wheelchair after reconstructive surgery | ||||||||
| Test | Total number of tests | Succeeded with the test n | Measurements | Mean | Min–max | Paired sample t-test (95% CI) | ||
| Upper | Lower | Significance 2-tailed | ||||||
| 25-m sprint | ||||||||
| Preoperative | 23 | 23 | Seconds | 19.739 | 10–38 | |||
| 12 months | 23 | 23 | Seconds | 18.152 | 9–30 | 0.46 | 2.72 | 0.007 |
| Figure-of-eight | ||||||||
| Preoperative | 23 | 23 | Seconds | 19.065 | 10–35 | |||
| 12 months | 23 | 23 | Seconds | 16.761 | 9–29 | 1.17 | 3.44 | 0.0004 |
| Uphill | ||||||||
| Preoperative | 23 | 13 | Seconds | 4.9762 | 3–17 | |||
| 12 months | 23 | 13 | Seconds | 4.1429 | 2–13 | 0.03 | 1.64 | 0.043 |
| 2.5 cm rim | ||||||||
| Preoperative | 23 | 18 | Seconds | 1.8261 | 1–11 | |||
| 12 months | 23 | 18 | Seconds | 1.0435 | 0.5–3 | 0.05 | 1.51 | 0.036 |
| 5 cm rim | ||||||||
| Preoperative | 23 | 7 | Seconds | 1.1842 | 1–7 | |||
| 12 months | 23 | 7 | Seconds | 0.8158 | 0.5–6 | –0.14 | 0.88 | 0.149 |
| Static push | ||||||||
| Preoperative | 23 | 23 | Kilogram | 15.826 | 3–37 | |||
| 12 months | 23 | 23 | Kilogram | 19.174 | 4–45 | –5.1 | –1.59 | 0.0007 |
| Buttock lift, 3 s | ||||||||
| Preoperative | 20 | 20 | % of weight | 42.55 | 3–100 | |||
| 12 months | 20 | 20 | % of weight | 46.55 | 9–100 | –8.91 | 0.81 | 0.097 |
| Hand strike | ||||||||
| Preoperative | 17 | 17 | Degrees | 100.53 | 75–125 | |||
| 12 months | 17 | 17 | Degrees | 102.82 | 82–122 | –8.29 | 3.71 | 0.43 |
| Paired t-test between preoperative results and 12 months postoperatively. Individuals who did not succeed with the test preoperatively were excluded from the statistical analysis. CI: confidence interval. | ||||||||
Individual improvements after completed reconstructive surgery
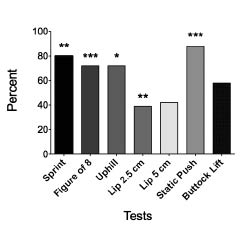
Overall, major improvements were recorded for most of the tests one year after completed surgery for each patient (n = 16). Eighty-nine percent of the 16 participants improved in static push, 81% in 25-m sprint, 69% in figure-of-eight, and 57% in buttock lift. Sixty-nine percent of the individuals improved in manoeuvring uphill, 2 persons succeeded after reconstruction and 3 persons remained unable to manoeuvre uphill after surgery. Forty-four percent of the participants improved in manoeuvring over a 5 cm rim. Paired comparisons of “sprint”, “figure-of-eight”,”uphill”,”2.5 cm rim” and “static push” demonstrated significant improvements (Fig. 2).
Fig. 2. Percentage of individuals who improved after completed reconstructive surgery. Statistical analyses of the individual improvements are based on paired variables. *p < 0.05, **p < 0.01, ***p < 0.001.
Comparing individuals with different levels of injury
Level of injury and triceps function differed between the individuals who only underwent grip reconstruction (n = 8) compared with those who only had elbow reconstruction or a combination of elbow and grip reconstructions (n = 8). The greatest difference between the groups was observed in the buttock lift. The individuals without preserved triceps function significantly improved (p = 0.02) after reconstruction of the elbow and hand. The group without triceps function was generally slower than those with preserved triceps for all speed tests and was weaker in static push forward (Table III). Only one person in the group with triceps function less than grade one succeeded to manoeuvre over the 5 cm rim before operation but two more succeeded after completed surgeries.
| Table III. Comparison of the results from wheelchair manoeuvring tests between individuals with different levels of injury. Group A and B represent individuals with triceps grade < 1 (n = 8) and grade > 1 (n = 8), respectively | ||||||||
| Wheelchair manoeuvring test | Group A | Group B | ||||||
| n | Pre Mean | Post Mean | p-value | n | Pre Mean | Post Mean | p-value | |
| 25 m sprint, s | 8 | 22.3 | 19.4 | 0.027 | 8 | 14.9 | 12.5 | 0.017 |
| Figure-of-eight, s | 8 | 21.4 | 16.8 | 0.028 | 8 | 12.8 | 11.6 | 0.056 |
| Uphill, s | 4 | 8.8 | 7.5 | 0.102 | 7 | 8.6 | 6.6 | 0.023 |
| 2.5 cm rim, s | 6 | 3.3 | 1.7 | 0.180 | 8 | 1.6 | 1.1 | 0.046 |
| 5 cm rim, s | 1 | 3 | 2 | – | 6 | 3.5 | 2.2 | 0.109 |
| Static push, kg | 8 | 12.3 | 16.5 | 0.018 | 8 | 24.1 | 29 | 0.017 |
| Buttock lift, % | 7 | 15.4 | 26.9 | 0.018 | 7 | 80.4 | 80 | 0.674 |
| Hand strike, degrees | 6 | 97.8 | 101.2 | 0.917 | 5 | 106.6 | 99.4 | 0.345 |
| Wilcoxon’s signed-rank test was used to compare preoperative and postoperative results. Individuals who did not succeed with the test preoperatively were excluded from statistical analysis. | ||||||||
Missing values were due to persons who did not bring their manual wheelchair or could not attend for follow-up, medical problems or technical issues. Five persons were excluded from the statistical analysis because they did not succeed with the test preoperatively, but succeeded postoperatively; 2 persons manoeuvring uphill and 3 persons over a 5 cm rim (Table II).
Complications
There were no serious adverse events in this group of patients. However, one patient had a skin ulcer caused by elbow plaster after triceps reconstruction and another patient had a haematoma in the palmar aspect of the forearm. Extra padding under the plaster combined with oral penicillin treatment, and compression over the haematoma, respectively, promptly treated both complications.
DISCUSSION
This study demonstrated that significant and clinically relevant improvements in wheelchair manoeuvrability skills could be detected after hand or arm reconstruction surgery. Donnelly et al. (14) identified functional mobility, including wheelchair use and transfers, as 1 of the top 3 problems listed by individuals with spinal cord injury. After hand and grip reconstruction the individuals are able to grip the rim and they can use the elbow extension when pushing forwards or regaining balance and this affects the patterns and abilities to manoeuvre the wheelchair. Interestingly, some individuals succeeded in performing the 5 cm lip test and manoeuvring uphill after surgery, but not preoperatively. The ability to use the new functions after tendon transfer is affected by several factors, such as muscle re-education, muscle strengthening, technique and motivation, and the improvements in using the arm/hand are likely to be due to a combination of these factors. Although patients included in this study did not have any specific manoeuvring skill training, their skills did improve. Specific wheelchair manoeuvring skill training may therefore advance the outcome even more.
Several studies have pointed out that physical activity is one factor that affects physical health of the SCI population (15–17). Better manoeuvring skills, improvements and, in some cases, regained ability in manoeuvring over a rim or up a slope, increase the independency level, which may have a positive effect on physical activity level.
Lack of grip function and loss of triceps function have been pointed out as factors that can affect the propulsion ability of the manual wheelchair. Individuals with tetraplegia have lower propulsion velocity than those with paraplegia and those with C6 injury propel slower than those with C7 injury (10, 18, 19). The ability to push with greater strength and propel faster significantly increases after reconstruction, although the angle between grip and release does not change. This indicates that the ability to develop force during wheelchair propulsion increases after reconstruction. Increased ability to develop force may have a positive effect on propulsion, as the ability to travel a longer distance per cycle increases. Subjects with tetraplegia devote more time to each metre travelled, and therefore subject their shoulders to a longer period of force (10). By increasing propulsion velocity and with a stronger forward push after reconstructive surgery the duration of force to the shoulder during propulsion may decrease. This may have a positive effect on preventing shoulder pain. Preoperative differences in propulsion velocity and strength to push forward were detected between those with preserved triceps and those with lack of triceps function; the former group being both stronger and faster preoperatively. However, both groups increased in their ability to manoeuvre the manual wheelchair postoperatively. Further studies are needed to investigate how reconstructive hand surgery specifically affects the shoulder and arm during different phases of wheelchair propulsion.
The skill of lifting the buttocks improved significantly in patients who underwent elbow reconstruction. The ability to unload the buttocks while seated in the manual wheelchair is important to prevent pressure sores. Studies have shown that a forward-leaning position and leaning side to side are more effective than pressure relief lift (20–21). With regained triceps function, persons with high level of injury can easily perform side-to-side leaning with better pressure relief and they can push themselves from a forward-leaning position up to sitting position. These are important factors in preventing pressure sores, even if they cannot perform a total pressure relief lift. The ability to lift the buttocks is also important during transfers, although other factors, such as balance, technique etc., play an important role.
Improvements after surgery are the results of the combined effects of surgical reconstruction and rigorous post-surgery training (22). Prior to surgery, the patient is carefully informed about the need to adhere to the ambitious rehabilitation programme. Therapists give details of the exercises and activities to perform, as well as restrictions to consider while the healing and relearning processes proceed. The improvements after surgery are also dependent on the level of injury and the type of surgery. Those with a lower level of injury and preserved triceps function have significant improvements in more advanced skills, such as driving up a slope, where the grip function is important. Persons with a higher level of injury that lacks triceps function, on the other hand, improve in skills that require improvements in the whole upper extremity. Both groups, however, improved significantly in forward push strength and speed. To test improvements after surgery and to set up reasonable goals it is important to take the type of surgery and the level of injury into account. Elbow extension reconstruction per se can provide important improvements for those individuals who lack triceps function, and further improvements can be made with a grip reconstruction.
The advancement of surgical techniques, together with progressively increasing complexity of the rehabilitation protocols in this field, make the necessity of a highly specialized team even more evident than before. The best way of building up and maintaining a high standard of service is to secure a high level of education of all personnel involved, provide functional infrastructure, carry out a sufficient number of surgeries per year, provide access to rehabilitation facilities, carry out continuous outcome measurements and enable development. This is usually possible in only a very few centres.
In conclusion, the results of this study demonstrate that the improvement in manoeuvring skills after reconstructive hand and arm surgery in individuals with tetraplegia implies increased mobility. Hand and arm function are highly prioritized goals in these groups of persons, and increased mobility is a crucial factor in living a more active life. Future studies are needed to demonstrate not only the long-term effects of reconstructive hand surgery and rehabilitation, but also the incorporation of new skills in order to increase other aspects of independence.
ACKNOWLEDGEMENTS
The Swedish Research Council Grant 11200, University of Gothenburg, Sahlgrenska University Hospital, and Promobilia Foundation provided funding for this project. The authors are indebted to Alastair Rothwell and Jennifer Dunn for planning the details of the study and for valuable suggestions during the course of the study. The authors are also indebted to Maria Knall for skilful technical assistance.
REFERENCES
