Kelvin W. K. Lau, MSc1 and Margaret K. Y. Mak, PhD2
From the 1Physiotherapy Department, Tung Wah East Hospital and 2Department of Rehabilitation Sciences, The Hong Kong Polytechnic University, Hong Kong
Kelvin W. K. Lau, MSc1 and Margaret K. Y. Mak, PhD2
From the 1Physiotherapy Department, Tung Wah East Hospital and 2Department of Rehabilitation Sciences, The Hong Kong Polytechnic University, Hong Kong
OBJECTIVE: To compare the effects of speed-dependent treadmill training on gait and balance performance in patients with sub-acute stroke.
DESIGN: Single-blinded randomized controlled trial.
SUBJECTS: A total of 26 patients with sub-acute stroke were randomly assigned to experimental (n = 13) and control (n = 13) groups.
METHODS: Subjects in the experimental group underwent short interval walking trials with stepwise increases in treadmill speed (speed-dependent treadmill training), following the principles of sprint training. Control subjects received gait training on the treadmill at a steady speed. Gait speed, stride length, cadence, and Berg’s Balance Score were recorded and analysed before and after the 10 training sessions.
RESULTS: Results of 2-way repeated measures analysis of variance showed significant group×time interactions for gait speed and stride length (p < 0.05). Within each subject group there were improvements in all gait parameters and Berg’s Balance Score after the training programme. In addition, the experimental group showed significantly larger increases in gait speed (mean 0.15 m/s, 95% confidence interval 0.04–0.26) and stride length (mean 0.16 m, 95% confidence interval 0.02–0.30) than the control subjects.
CONCLUSION: Speed-dependent treadmill training in patients with sub-acute stroke resulted in larger gains in gait speed and stride length compared with steady speed. The positive findings provide evidence for clinical practice of speed-dependent treadmill training in enhancing gait function after stroke.
Key words: gait; hemiplegia; treadmill; physiotherapy; rehabilitation.
J Rehabil Med 2011; 43: 709–713
Correspondence address: Margaret K. Y. Mak, Department of Rehabilitation Sciences, The Hong Kong Polytechnic University, Hong Kong. E-mail: rsmmak@inet.polyu.edu.hk
Submitted January 19, 2011; accepted May 5, 2011
INTRODUCTION
Stroke is the leading cause of morbidity and mortality in elderly people (1). According to Cheng et al. (2), approximately 30% of stroke survivors are permanently disabled and require assistance in their daily activities. Stroke survivors commonly have impaired motor control and balance that seriously affect their walking ability, leading to dependence and increasing burden to carers and society. Gait training is therefore a major goal in stroke rehabilitation. New modalities have been introduced for gait rehabilitation in patients with stroke. Previous studies have reported that body-weight supported gait training on a treadmill (BWSTT) improved walking performance in patients with stroke. The pioneer study of BWSTT in patients with chronic stroke was performed by Hesse et al. (3). These investigators demonstrated that BWSTT resulted in significantly more improvement in gait performance than Bobath training of patients with chronic stroke (3). Subsequent studies further reported that BWSTT had significantly higher gains in functional and gait outcome than conventional training in patients with sub-acute stroke (4, 5). BSWTT also significantly improved lower limb muscle strength (6) and balance performance (5, 7). BWSTT was further found to enhance cardiovascular and functional performance (8) and to reduce energy expenditure (9). These aforementioned studies instructed patients to walk at a tolerated and comfortable speed. Pohl et al. (10) examined the effect of speed-dependent treadmill training (SDT) on gait in patients with stroke. The training mode draws on the principles of sports physiology, which have demonstrated that training at subjects’ sub-maximal level does not provide optimal improvement in gait speed. In contrast, sprint training at maximum speed, while not intended to over-exert patients, results in optimal performance (11). After 2 weeks of training, subjects in the SDT group had significantly more improvement in gait performance than those with conventional treadmill training. Although the findings were encouraging, the effect of SDT was examined in patients with chronic stroke; hence its effect in patients with sub-acute stroke is not known. This study aimed to investigate the effects of SDT on gait and balance performance in patients with sub-acute stroke. Specifically, to explore whether 2 weeks of speed-dependent treadmill training is more effective at increasing walking speed, step length, cadence and improving balance than 2 weeks of speed-stable treadmill training in patients with subacute stroke.
METHODS
Subjects
Patients with stroke who were admitted to the rehabilitation unit of Tung Wah East Hospital were recruited. Inclusion criteria for the study were as follows: first episode of stroke; within one month of stroke onset; hemiparesis resulting from unilateral ischaemic stroke; Ashworth score of 0 or 1, indicating no spasticity or slight spasticity over the affected lower limb, respectively (12); mini-mental state examination score ≥ 23 (13); and the ability to walk on level ground without physical assistance and to walk on a treadmill with a minimum speed of 22.2 cm/s for 30 s. Subjects were excluded if they had neurological diseases other than stroke, active cardiovascular disease (i.e. American Heart Association class C or above), lower limb fractures, total hip replacement, or active rheumatoid arthritis that affected their gait performance. Patients who required assistance to ambulate before the stroke were also excluded. The study was approved by the university and hospital ethics committees. All subjects had to provide written informed consent in accordance with the Declaration of Helsinki. The trial was registered at www.clinicaltrials.gov (identifier: NCT01328301).
Treatment intervention
Subjects in both the experimental (SDT) and control groups received 30 minutes of locomotion training on a treadmill. Before the gait training, subjects were fitted with a harness for safety purposes; no body-weight support was given. The need to use the handrail for support was assessed before each session and minimal hand support was encouraged during training sessions. The initial belt speed of the treadmill was determined by the fastest over-ground gait speed obtained from the subject’s 10-m walk (10MW) test before each training session. For SDT training, subjects received short intervals of locomotion training with a treadmill. After walking for 30 s, the subjects had a 2-min rest. If they completed the first walking trial safely and without stumbling, the belt speed was increased by 10% on the next trial. However, if a subject failed to complete the first trial, the belt speed was decreased by 10% on the next trial. The speed of the treadmill was adjusted in each subsequent trial according to the same principle. In a single training session, subjects usually completed 7–8 walking trials in approximately 4 min. The belt speed was increased by a maximum of 5 increments within one training session.
Subjects in the control group walked on the treadmill with the belt speed adjusted according to their fastest over-ground gait speed. There was no adjustment of the belt speed throughout the 30-min steady-speed treadmill training (SST) session. During both SDT and SST, close supervision was provided by a physiotherapist to monitor subjects’ cardiac condition, discomfort level, and musculoskeletal problems during training, and to prevent loss of balance. In addition to locomotion training on the treadmill, subjects in both groups also received 90 min of rehabilitation, which included motor relearning, neuro-development techniques, integrated sensory stimulation, and conventional gait training.
Outcome measures
All outcome measures were collected by an investigator who was blind to the group assignment. Baseline demographic data including name, age, gender, date of stroke onset and medical history were collected. All subjects received an initial and a final assessment session. The initial assessment was performed before the first treatment session of the training programme and the final assessment was performed on the day after the last treatment session. Outcome measures included a 10MW test and Berg’s Balance Scale (BBS).
Gait performance was measured by a 10MW test. Subjects were instructed to walk at their fastest speed on a 10-m walkway (14), and were allowed to use their walking aids or assistive devices. Video-recording of the tests allowed off-line calculation of gait speed, cadence and stride length (15). One practice trial was given followed by 3 test trials, and the trial with the fastest speed was used for further analysis. The formulae for the calculation are as follows:
• gait speed (cm/s) = 1,000 cm/time (s) to walk the 10-m walkway
• cadence (steps/min) = number of steps to walk the 10-m walkway × 60/time (s) to walk the 10-m walkway
• stride length (cm) = 1,000 cm/number of steps to walk the 10-m walkway
Balance performance was determined by BBS. The scale consists of 14 items, including the ability to maintain sitting balance, static and dynamic standing balance, and stability during functional transfer tasks (16). Each item is scored from 0 (cannot perform the task) to 4 (the best performance), with a total score range of 0–56. BBS is a well-established balance assessment tool that has been found to have excellent inter- and intra-rater reliability (r > 0.98) (17). Before the main study, the test-retest reliability of the procedures for testing gait parameters and BBS was examined in 5 patients with chronic stroke. The results indicated excellent reliability, as shown by the intra-class correlation coefficients (gait speed = 0.97, cadence = 0.98, stride length = 0.89, BBS = 1.00) (18).
Statistical analysis
SPSS 16 software was used for data analysis (SPSS Inc., Chicago, IL, USA). Descriptive analysis was used to analyse the demographic data in each subject group. A 2-way repeated measures analysis of variance (ANOVA) was used to analyse gait and balance performance with time (week 0 and week 2) as the within-group factor and gait (experimental and control) as the between-group factor. When an interaction between group and time was found, post-hoc tests were used to determine the real within- and between-group differences. We further computed the changes in each outcome measure (gait speed, cadence, stride length, BBS score) between the pre- and post-treatment assessment sessions. The mean differences and 95% confidence intervals (95% CI) were calculated for the experimental and control groups. The level of significance was set at 0.05.
RESULTS
Fig. 1 shows that, of the 150 patients admitted with stroke, 30 met the inclusion and exclusion criteria. Subjects were allocated randomly to either the experimental group (n = 15) or the control group (n = 15). Subjects in the experimental group received SDT training, whilst control subjects received SST training. Four subjects withdrew from the study, 2 from each group. Twenty-six subjects completed 10 training sessions, with 13 in each group. Table I shows the demographic data for all subjects and for those who dropped out during the study, as well as the characteristics of the therapists who participated in the study. Table II illustrates the gait parameters and BBS score for both groups. Results of the 2-way repeated measure ANOVA showed significant interactions (group × time) for gait speed and stride length (p < 0.05). Within each subject group, there were improvements in gait speed, stride length, cadence and BBS score. Further between-group comparison of the pre- and post-treatment changes showed that subjects in the experimental group had significantly more increases in their gait speed (mean 0.15 m/s (m/s), 95% CI 0.04–0.26, p = 0.014) and stride length (mean 0.16 m, 95% CI 0.02–0.30, p = 0.027) than the control subjects. All subjects completed 10 training sessions. Throughout the training sessions, there were no falls, acute chest pain, or any incidence of a sudden drop in blood pressure in all subjects
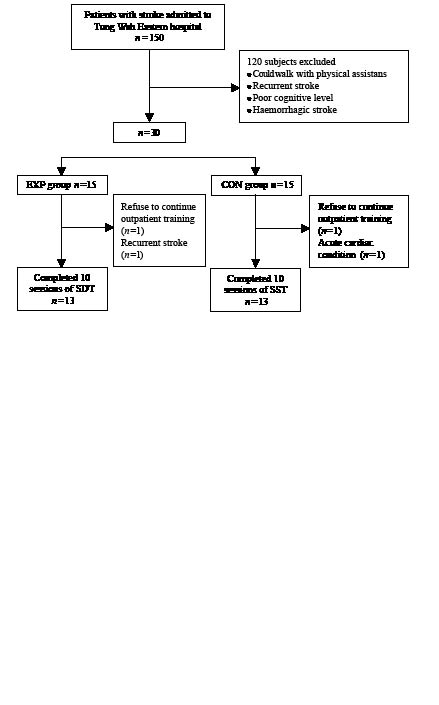
Fig. 1. Subject recruitment for the study. EXP: speed-dependent treadmill training group; CON: control group.
| Table I. Baseline characteristics of participants and therapists | ||||
| Characteristics | Participants | |||
| Randomized (n = 30) | Lost to follow-up (n = 4) | |||
| EXP (n = 15) | CON (n = 15) | EXP (n = 2) | CON (n = 2) | |
| Participants | ||||
| Age, years, mean (SD) | 69.5 (11.1) | 72.1 (9.2) | 72.5 (20.5) | 74.5 (3.5) |
| Gender, males, n (%) | 10 (66.7) | 11 (73.3) | 1 (50) | 2 (100) |
| Time since stroke, days, mean (SD) | 12.9 (5.3) | 12.7 (5.7) | 16.5 (7.8) | 17 (4.2) |
| Therapists | ||||
| Participants treated, n (%) | ||||
| 1 | 10 (66.7) | 11 (73.3) | 2 (100) | 1 (50) |
| 2 | 2 (13.3) | 2 (20.0) | 0 (0) | 1 (50) |
| 3 | 3 (20.0) | 1 (6.7) | 0 (0) | 0 (0) |
| SD: standard deviation; EXP: speed-dependent treadmill training group; CON: control group. | ||||
| Table II. Mean (standard deviation; SD) of groups, mean (SD) difference within group, and mean (95% confidence interval; CI) difference between groups | |||||||
| Outcome | Group | Difference within groups | Difference between groups | ||||
| Week 0 | Week 2 | Week 2 minus Week 0 | |||||
| EXP (n = 15) | CON (n = 15) | EXP (n = 13) | CON (n = 13) | EXP | CON | EXP minus CON | |
| Walking: speed, m/s | 0.28 (0.19) | 0.30 (0.19) | 0.64 (0.32) | 0.52 (0.21) | 0.34 (0.18) | 0.19 (0.09) | 0.15* (0.04 to 0.26) |
| Walking: step length, m | 0.65 (0.23) | 0.68 (0.24) | 1.04 (0.35) | 0.92 (0.31) | 0.35 (0.20) | 0.19 (0.15) | 0.16* (0.02 to 0.30) |
| Walking: cadence, steps/min | 36.9 (16.6) | 39.5 (15.0) | 58.5 (15.9) | 55.9 (12.0) | 18.6 (8.9) | 13.3 (10.6) | 5.4 (–2.6 to 13.2) |
| Balance: BBS, 0–56 | 37.7 (13.3) | 41.3 (13.0) | 50.3 (6.3) | 52.1 (2.3) | 9.9 (7.3) | 7.9 (9.7) | 2.0 (–5.0 to 9.0) |
| *p < 0.05. EXP: speed-dependent treadmill training group; CON: control group; BBS: Berg’s Balance Scale. | |||||||
DISCUSSION
The present study demonstrates that 10 sessions of SDT and SST training significantly increased gait and balance performance in patients with sub-acute stroke. In addition, this is the first study to show that SDT training can produce significantly larger gains in gait speed and stride length than SST. These findings provide evidence that SDT is more effective than SST in improving gait speed and stride length in patients with sub-acute stroke.
Effect of treadmill training on gait performance
The improvement in the gait speed of control subjects was 1.19 m/s, which was consistent with previous findings (4, 5). Our findings for SDT training agree with those reported by Pohl et al. (10). However, the increases in gait speed and stride length in our subjects after 2 weeks of training were 120% and 55%, respectively, which were larger than those reported by Pohl et al. (10). In their patients, gait speed increased significantly by 85% and stride length by 36%. This difference could be explained by differences in the sample, such as the time since stroke, baseline mobility and training protocol.
The subjects in our study were in the sub-acute stage, with a mean of 12.6 days since stroke onset, whereas those in the Pohl et al. (10) study were in the chronic stage (mean = 113.4 days after stroke onset). The natural course of stroke recovery has been shown to contribute to 50% of overall motor recovery within the first 2 weeks after stroke, and 80% of overall recovery after 1 month (19). Patients recruited in the present study were in the sub-acute stage, which might have led to more rapid gait recovery in response to the treadmill training compared with patients in the chronic stage. The baseline mobility level of patients in the present study was lower than those in the Pohl et al. (10) study, which may also help to explain the differences in the changes in gait speed and stride length.
Although our SDT training protocol was based on that of Pohl et al. (10), we made several changes because most of our patients had postural instability and low mobility. First, our patients were allowed to hold onto the handrails during gait training on the treadmill and this support was gradually decreased as patients progressed (4, 5). The hand support may have improved patients’ stability and confidence to walk with a longer stride and faster speed. Secondly, the duration of each walking trial was 30 s, which was longer than the 10 s used by Pohl et al. (10). This duration was based on the observation from our pilot trial that most patients with sub-acute stroke required 30 s to establish a more stable gait pattern. Thirdly, the rest time between walking trials was 2 min in the present study. SDT is a form of sprinting exercise, in which the rest period between walking trials allows patients to recover from muscle fatigue and to avoid overstressing the cardiopulmonary system. Pohl et al. (10) instructed patients to rest until they resumed their resting heart rate. We observed in our pilot trial that patients showed no signs of cardiopulmonary stress after each walk, and they required approximately 2 min to recover from their muscle fatigue. Some patients required up to 8 min to resume their resting heart rate even when they had no muscle fatigue. Such a long resting period might not be feasible in clinical practice, thus we chose to use a 2-min rest period between each walk. Fourthly, our training lasted for 10 sessions, while that of Pohl et al. (10) lasted for 6 sessions.
The finding that our patients showed a larger improvement in gait speed and stride length than those reported by Pohl et al. (10) could be attributed to the sub-acute phase of stroke, the availability of hand support, the longer duration of each walking trial, shorter resting time, and more training sessions.
Effects of treadmill training on balance performance
Control subjects showed significant increase in BBS score, which agreed with the previous findings of BWSTT (4, 7). The present study is the first to show that SDT can significantly improve balance performance in patients with sub-acute stroke. The non-significant interaction indicates that both SDT and SST training had a similar effect on balance performance in patients with stroke. Balance is a complicated issue and balance performance could be affected by multiple factors, including co-ordination, muscle strength, and vestibular, visual and sensory functions. Although locomotion training on a treadmill could affect some of these factors, it is difficult to isolate any particular aspect that might be responsible for the improvement in balance. In addition, because treadmill training is task-specific, the treatment outcome should be related to the task that is most directly affected by the training mode, which is gait performance (20).
Mechanisms underlying improvements in gait performance after treadmill training
The findings of the present and previous studies (7, 10, 21) show that treadmill training can improve gait performance in patients with stroke. The positive effect could stem from the activation of the central gait pattern generator (22). The walking pattern of patients with stroke is characterized by a short swing phase. When patients with stroke walk on the treadmill, the rapid extension of the paretic hip may facilitate a reflex hip flexion (23). Walking with greater hip flexion could lead to a larger swing, longer stride length, and a more symmetrical and efficient gait pattern (24). The improvement in over-ground gait performance shows that locomotion training on a treadmill can be transferred to level ground (4, 25). Treadmill walking is task-specific and repetitive, and these characteristics are shown to be more effective than strengthening exercises to enhance motor learning in patients with stroke (6, 26). These factors could account for the improvement in gait performance in both the SDT and the control group.
In addition to its task-orientated nature, SDT adopts a sprint training mode and distributed practice, whereas SST uses mass practice. Previous studies have shown that distributed practice with variable content produces better motor recovery than mass practice (27, 28). During SDT, subjects walked at their highest tolerated speed for a short interval of 30 s, and rests were given between walking trials. During the rest period, the therapist would give feedback on patients’ performance in form of knowledge of results, and suggest ways to improve on the next walking trial. Based on this feedback, patients were asked to rehearse their gait pattern mentally before the subsequent trial. Mental rehearsal involves high-level cognitive processing, which has been reported to enhance motor performance (29, 30). For SST, patients walked at a constant speed throughout 1 training session for 30 min. During the gait training on the treadmill patients were given feedback on their performance. At the end of the programme, the belt speed used in the SDT training was 1.31 m/s, which was much higher than the 0.62 m/s for SST. In addition, patients in the SDT group had made greater gains in gait speed and stride length. It appears that SDT with short intervals of walking at patients’ maximal level could be more effective than longer durations at a sub-maximal level. Feedback in the form of knowledge of results could have more effect on motor learning than knowledge of performance (31). The use of motor practice could also contribute to gait improvement in SDT subjects.
Subjects in the SDT group increased the gait speed by 0.34 m/s after 10 sessions of training. Furthermore, subjects in the SDT group showed a significantly larger gain in gait speed by 0.15 m/s than conventional SST training. This improvement is close to the minimum clinically importance difference (i.e. 0.16 m/s) found in patients with sub-acute stroke (32). This implies that SDT training is likely to produce more improvement in the disability level than control subjects (33). The results of this study provided evidence that the SDT training regime can be applied in clinical practice, especially in the acute stroke setting.
There are several limitations that should be addressed. First, the findings of this study could only be applied to patients with higher baseline mobility; that is, patients who are able to walk without physical assistance for 10 m. The effectiveness of SDT on more dependent groups of patients, or on those patients who require weight-support gait training, is not clear. Secondly, the effect of different parameters of SDT, such as treatment duration, intensity and training time, were not examined in the present study. Thirdly, the long-term effect of SDT was not examined in this research. A large-scale randomized controlled trial is needed to investigate the effect of SDT on patient groups with different mobility levels, the parameters and intensity of SDT, the carry-over effect of SDT, and the mechanisms underlying the improvement in gait and balance performance following SDT.
To conclude, 10 sessions of SDT and SST improved gait and balance performance in patients with sub-acute stroke. However, SDT showed larger gains in gait speed and stride length compared with SST. The results of this study show that SDT was more effective than SST for improving gait speed and stride length in patients with sub-acute stroke. SDT training is a simple, safe, feasible and tolerable exercise modality that is recommended for the rehabilitation of patients with sub-acute stroke.
REFERENCES
