OBJECTIVE: The aim of this study was to determine whether a 12-week course of low-frequency vibrating board therapy is a feasible therapy for non-specific chronic low back pain, and whether it improves the main outcome measures.
DESIGN: Randomized controlled trial.
Patients: A total of 50 patients with non-specific low back pain were included. They were randomly assigned to either a vibrating plate via reciprocation therapy group (n = 25) or a control group (n = 25).
METHODS: The 12-week vibration therapy programme consisted of a total of 24 training sessions (2 times/week, with 1 day of rest between sessions). Assessments of the main outcome measures for non-specific low back pain were performed at baseline and at 12 weeks.
RESULTS: In the vibration therapy group there was a statistically significant improvement, of 20.37% (p = 0.031) in the Postural Stability Index (anterior–posterior); 25.15% (p = 0.013) in the Oswestry Index; 9.31% in the Roland Morris Index (p = 0.001); 8.57% (p = 0.042) in EuroQol 5D-3L; 20.29% (p = 0.002) in the Sens test; 24.13% (p = 0.006) in visual analogue scale back; and 16.58% (p = 0.008) in the Progressive Isoinertial Lifting Evaluation test.
CONCLUSION: A 12-week course of low-frequency vibrating board therapy is feasible and may represent a novel physical therapy for patients with non-specific low back pain.
Key words: rehabilitation; postural balance; back pain; disability; proprioceptive feedback.
Journal Rehabil Med 2011; 00:00–00
Correspondence address: Narcis Gusi Fuertes, Faculty of Sports Sciences, University of Extremadura, Avenida de la Universidad s/n, 10003 Caceres, Spain. E-mail: ngusi@unex.es
Submitted December 6, 2010; accepted April 28, 2011
INTRODUCTION
Approximately 80% of the world’s population will develop low back pain (LBP) during adulthood (1). In 80% of cases of LBP it is difficult to identify the cause (2). Non-specific low back pain (NLBP) is one of the most frequent presentations in primary care. Between 7% and 9% of all individuals from the general population with a disorder of the lumbar spine will consult their primary care physician (3). Most episodes of low back pain (LBP) resolve rapidly and are not incapacitating (4). However, non-specific chronic low back pain (NCLBP) is a highly incapacitating disorder (5), which is associated with substantial use of healthcare resources as a result of medical consultations, investigations, and prescriptions. The disorder also has a negative impact on social and employment resources, mainly as a consequence of lost working days (6). Long-term incapacity substantially increases the risk that the disorder will become chronic, and reduces the likelihood of an early return to work (7).
Although research suggests that exercise decreases pain and improves function in patients with NCLBP (8), there is no consensus regarding the most appropriate form of exercise (9). The popularity of whole body vibration (WBV) has increased over the last decade, and studies of WBV in healthy subjects have concluded that this form of training is useful in improving the strength of the lower extremities (10), balance (11), neuromuscular performance (12), and health-related quality of life (HRQoL) (13). A recent review concluded that WBV is useful in a range of medical disorders (14). WBV has also been shown to be a feasible therapy for use in frail individuals who were previously physically untrained (15).
WBV involves the use of oscillatory muscle stimulation. The foot is placed on a platform that vibrates at a predetermined frequency and amplitude. The vibrations are then transmitted throughout the body, eliciting muscle stimulation through vibratory tonic reflex when the short and fast changes in muscle length are detected by different proprioceptive organs, which enhance the frequency of motor evoked potentials (14). However, the feasibility and application of WBV in specific populations has not yet been investigated (14).
Research has shown that most patients with NCLBP are physically unfit and report low HRQoL. In addition, they display proprioceptive deficits, which may be secondary to pain (16). Exposure to vibrations has traditionally been considered harmful (17). However, the results of several studies suggest that WBV relieves chronic back pain (18) through a genuine analgesic effect, and that vibration per se suppresses pain (19). Furthermore, studies in the general population have shown that WBV improves muscle strength (12) and may contribute to preserving those aspects of physical fitness that are affected in NCLBP. The vibration perception threshold is considered to be an index of proprioceptive ability (20). Deficits in proprioceptive ability have been demonstrated in patients with NCLBP (21). Given that the proprioceptive system is responsible for maintaining balance, the threshold of sensitivity to vibration can be considered an important parameter in the NCLBP population (21). Patients with LBP often experience problems secondary to falls (22). WBV had been reported to improve balance (23) and gait speed (24), both of which are independent predictors of the risk of falling (14).
Few studies have investigated the use of WBV in NCLBP using tilt devices. Iwamoto et al. (25) reported that 4 min of 20 Hz tilt WBV per week for 12 months reduced the severity of NCLBP in post-menopausal women. Rittweger et al. (18) followed up a cohort of WBV patients for 6 months, and suggested that well-controlled vibration may be a cure for, rather than the cause of, LBP. Nevertheless, no previous study has investigated the effects of tilting low-frequency WBV on the main outcome measures for NCLBP.
The aim of the present study was to test the hypotheses that a 12-week course of low-frequency vibrating board therapy would be feasible and improve the main disability index and HRQoL outcome measures for NCLBP. The study also investigated whether this form of therapy would improve postural stability, physical function, and the foot vibration perception threshold in the NCLBP population.
METHODS
Participants
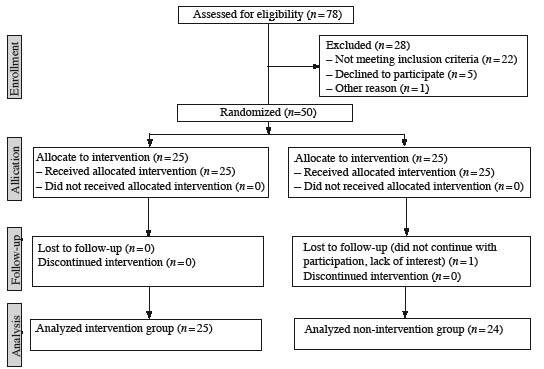
Fifty patients with NCLBP were recruited from a public health service pain unit in Extremadura. All study participants provided written informed consent. One patient subsequently dropped out of the study, and only the data of the 49 participants who completed the study were included in the analyses (Fig. 1). The study inclusion criteria were: aged 40–70 years; diagnosis of NCLBP according to the International Classification of Diseases, Ninth Revision (ICD-9) in the absence of any major neurological deficit; and a minimum of 6 months of NCLBP symptoms.
Fig. 1. Study participants.
The study exclusion criteria were: NCLBP of known aetiology; any other major disease; regular physical activity (i.e. more than once a week) during the previous 5 years; use of any medication that may significantly affect balance; diabetes; use of any medication with potential neurotoxic effects (e.g. pharmacological treatments for cancer or human immunodeficiency virus). All participants were receiving standardized medical care via the public health system (primary care; hospital and outpatient clinic).
All participants were randomly assigned to one of the two study groups using a table of random numbers: (i) a vibrating plate via reciprocation group (n = 25; WBV group); or (ii) a control group (n = 25). The 12-week vibration therapy programme consisted of a total of 24 training sessions. Training was performed twice a week, with at least 1 day of rest between any 2 consecutive sessions. All participants were assessed at baseline and at 12 weeks.
The study was conducted in accordance with the recommendations of the Declaration of Helsinki, and was approved by the Bioethics Committee of the university. The study was registered as a randomized controlled trial (ISRCTN31946666).
Whole body vibration group
A commercially available vibration device was used (Galileo 2000; Novotec GmbH, Pforzheim, Germany). The vibration exercise was performed in a standing position. The participant was asked to remove their shoes in order to eradicate any damping of the vibrations. The participant stood on the platform with their feet side by side. The angle of the knee was set at 120º in order to avoid any reduction in the transmission of the vibrations to the upper body (spine and head) and to increase the effort of the leg muscles. The platform generated side-alternating oscillations of the whole body. The training protocol is shown in Table I.
| Table I. Characteristics of whole body vibration (WBV) therapy |
| Weeks | Sessions n | Time series s | Repetitions n | Frequency Hz | Interval rest s | WBV total time s |
| 1–2 | 1–4 | 60 | 6 | 20 | 30 | 360 |
| 3–4 | 5–8 | 120 | 3 | 20 | 30 | 360 |
| 5–6 | 9–12 | 180 | 2 | 20 | 30 | 360 |
| 7–8 | 13–16 | 240 | 2 | 20 | 30 | 480 |
| 9–10 | 17–20 | 360 | 1 | 20 | – | 360 |
All participants in the control group were asked to continue with their normal pattern of daily activity for the 12-week duration of the study
Instruments
All participants were evaluated at baseline and at 12 weeks. The questionnaires were administered by a trained interviewer. The physical tests were administered by an experienced physical fitness tester. All testers were blinded to the group allocation of the participants.
Instrument for assessing peripheral sensory function
The Vibratron II device (Sensortech, Inc., Clifton, NJ, USA) was used to assess peripheral sensory function. The instrument consists of a controller and two identical “slave” transducers. A 15 cm diameter plastic post protrudes from each transducer. The transducer and the post generate a 120 Hz vibrating stimulus. The amplitude of vibration is determined by the applied voltage, which is adjusted manually via the controller unit. The amplitude of vibration is quantified in “vibration units”, which are displayed digitally on the controller unit.
The method-of-limits (MOL) yes-no procedure was used. The term “method-of-limits” refers to the determination of the delivered stimulus intensity, and the term “yes-no” refers to the participant’s response to the stimulus. The procedure commenced with the delivery of supra-threshold stimulation that could be detected easily by the participant. The intensity of the stimulation was reduced gradually at a constant rate. The participant was asked to indicate verbally the earliest point in time at which they could no longer perceive the vibration. This setting was recorded, and the participant was asked to lift their great toe from the stimulator post. The intensity of stimulation was then reduced to a level well below the threshold of the previous trial, and the participant was asked to place their great toe on the stimulator post.
Studies of vibration thresholds in normal subjects have reported average intra-subject coefficients of variation of as low as 7–10%, whereas values in the order of 10–20% have been found in patients with diabetes (26). The reliability of the test used in the present study was measured in a laboratory at the University of Extremadura using 10 of the NCLBP participants and a 7-day test-retest protocol. The intra-class correlation coefficient (ICC) was 0.97 (95% confidence interval (CI) 0.85–0.99), and the standard error of measurements (SEM) was 13.6%.
Six-min walk test
The six-min walk test (6MWT) is a measure of aerobic endurance. It is an inexpensive, relatively quick, safe, and well-tolerated method of assessing functional exercise capacity in a range of diseases (27). The participant was asked to walk as far as possible along a pre-selected course for 6 min. The distance walked was then recorded. This test has excellent reliability (r = 0.91). It is also sensitive to post-exercise change in distance walked (+78 m), and maximum volume of oxygen consumed (VO2) (+1.8 ml/kg/min) in other painful diseases such as fibromyalgia.
Progressive Isoinertial Lifting Evaluation
Progressive Isoinertial Lifting Evaluation (PILE) assesses the ability to perform repetitive lifting as quickly as possible. Each participant performed the maximum number of series as they were able to perform of lifting. In each series, the participant was asked to lift a weighted box from the table to the floor and back again 4 times within a time of 20 s. A new series of lifting was commenced following 20 s of rest. Weight increments of 4.5 kg for men and 2.25 kg for women were used per series until a criterion for maximum performance was reached. The measured outcome was the sum of the weight (in kg) from all series of lifting. The test was terminated when acceptable maximum effort was reached; lifting became unsafe; the heart rate of the participant reached 85% of the maximal rate for their age; the weight limit was reached (40.5 kg); or the speed of lifting was not maintained. The materials required for the test are a plastic box (36 × 26 × 18 cm); a table (height 71 cm); 2.25 kg weights; a Polar heart rate monitor; and a visual analogue pain scale (VAS) for exertion ranging from 0 to 100 (20 cm). A previous study of the reliability of the PILE test reported an ICC of 0.91 (28). The reliability of the test used in the present study was measured in the university laboratory in 10 of the NCLBP participants using a 7-day test-retest protocol. The ICC was 0.88 (95% CI 0.74–0.94) and the SEM was 16.6%.
Biodex balance system
In the postural stability test (PS), the platform remains static in the anterior-posterior and medial-lateral axes, which allows measurement of the following two variables: (i) the anterior-posterior stability index (APSI); and (ii) the medial-lateral stability index (MLSI) (further information concerning explaining the measures of this device can be found in the article by Arnold & Schmitz (29)). Each participant performed 3 trials of the test. The duration of each trial was 20 s, and the participant was allowed a 1 min rest between each trial. Previous studies have reported similar results for the dominant and non-dominant legs. Thus, in view of cost-considerations, only one leg was tested. To determine the dominant leg, the participant was asked which leg they would use to kick a ball (30). In each trial, the participant was asked to adopt a single dominant-limb stance while maintaining slight flexion of the knees (15º). The posture of the arms was not regulated. For both APSI and MLSI, the mean value of the 3 trials was calculated.
To our knowledge, there are no data concerning the reliability of the APSI and MLSI indices in NCLBP. The reliability of the test used in the present study was measured in the university laboratory using 10 of the NCLBP participants and a 7-day test-retest protocol. For the APSI index, the ICC was 0.96 and the SEM was 14.4%. For the MLSI index, the ICC was 0.97 and the SEM was 13.5%.
Questionnaires
The Roland Morris Questionnaire (RM) and the Oswestry Disability Index (Oswestry) (31) were used to assess the level of NCLBP-associated disability. In the RM, the respondent is asked to put a mark next to each appropriate statement. The total score is obtained by adding up the total number of marked statements. The possible total score ranges from 0 (minimal disability) to 24 (maximum disability). In the Oswestry, the ODI index is calculated according to the following formula: (total score/50)× 100. This indicates the percentage of disability that is attributable to back pain. This ranges from 0% (no disability) to 100% (maximum disability). To assess HRQoL, the EuroQol 5D-3L (EQ-5D-3L) (32) was used. The EQ-5D-3L has 5 dimensions, and each dimension is scored from 1 (best possible health state) to 3 (worst possible health state). The time trade-off tariff (tto) from a previous study in the Spanish population was used. Each participant was asked to indicate their current level of pain using a 20 cm VAS that ranged from 0 (no pain) to 100 (highest level of pain). The VAS has been reported to be a reliable and valuable method of assessing pain (33).
Statistical analysis
All variables were compared at baseline using Student’s t-test for independent samples. The Kolmogorov-Smirnov test with Lilliefors correction was used to examine the distribution of the data. After confirming that the distribution of all variables was parametric, a two-way analysis of variance (ANOVA) for repeated measures was used to compare the two study groups. The significance level was set at p < 0.05.
In addition to p-values, the statistical analyses included consideration of the mean values and 95% CIs. This provided a more detailed depiction of both the change within each intervention group between baseline and 12 weeks, and the treatment effect. If the null value of the comparative measure (mean) lies within the CI, then the result is not statistically significant. This approach is recommended for publications in biomedical journals to help other authors and readers determine the size of the reported differences and to compare the intervention within the context of other studies. This is particularly useful for the intervention used in the present study, as it allows comparisons to be made with other groups (e.g. sedentary groups or groups that underwent different forms of training). The difference between post- and pre-test outcomes was used to describe the changes from baseline to 12 weeks. Treatment effect was estimated by comparing the differences in each individual outcome measured over the 12-week study period between the two study groups. The mean and 95% CI of each change were calculated using Student’s t-test for independent samples.
A 7 day step-test reliability study was conducted on the outcomes of our study with 10 study participants. The relative reliability was determined from two sessions according to the ICC3,1. The ICC was used to check the concordance between both, test and retest measures in numeric variables, rather than the kappa test, which normally is used in categorical data, although both kappa and ICC give similar results in some conditions. The absolute reliability was determined according to the SEM (SEM = SD√(1–ICC)), where SD is the mean SD of day 1 and day 2.
Effect size was calculated to determine the magnitude of change. The difference between means was divided by the mean SD of either group. Cohen’s coefficient was used to assess the magnitude of the change. A change of 0–0.2 was considered very small; 0.2–0.6 small; 0.6–1.2 moderate; 1.2–2.0 large; and > 2.0 very large. All analyses were performed using the statistical package SPSS 19.0.
RESULTS
The socio-demographic characteristics of the study participants are shown in Table II. At baseline, no statistically significant differences were observed in any of the key measures between the two groups.
| Table II. Socio-demographic characteristics of study participants (n = 49) |
| Group | Control group (n = 24) | WBV group (n = 25) | p-valuea |
| Sex, male/female, % | 28/72 | 25.9/74.1) | |
| Age, years, mean (SD) | 59.53 (5.47) | 58.71 (4.59) | 0.54 |
| Weight, kg, mean (SD) | 78.91 (6.53) | 72.65 (10.61) | 0.11 |
| Height, cm, mean (SD) | 158.51 (8.84) | 156.11 (9.44) | 0.35 |
| BMI, kg/m2, mean (SD) | 31.47 (6.41) | 2.86 (3.84) | 0.27 |
| ap-values from Student’s t-test. WBV group; whole body vibration group; SD: standard deviation. |
Safety, feasibility and compliance
The WBV programme was a feasible and safe form of therapy in patients with NCLBP, and was associated with a high level of treatment compliance. None of the study participants reported any study-related adverse effects. None of the participants from the WBV group reported any negative effects on health during treatment. In the WBV group, 100% of the 25 participants completed the 12-week programme. One participant from the control group dropped out due to lack of interest. Thus, 96% (24 of 25) of the control group completed the 12-week study.
Effects of intervention
Table III shows the effects of the 12-week programme on postural stability, physical function, HRQoL, disability, and foot vibration perception threshold. In the WBV group, there was a statistically significant improvement of 20.37% (p = 0.031) in the APSI test; 25.15% (p = 0.013) in the Oswestry Index; 9.31% in the Roland Morris Index (p = 0.001); 8.57% (p = 0.042) in HRQoL, as measured by the EQ-5D-3L; 20.29% (p = 0.002) in the Sens test; 24.13% (p = 0.006) in VAS back and 16.58% (p = 0.008) in the PILE test.
| Table III. Effects of a 12-week course of whole body vibration (WBV) training in patients with chronic non-specific low back pain (n = 49) |
| Outcome measure | Baseline | | Post-treatment | Treatment effect Mean (95% CI) | pa | Effect size |
| Control group (n = 24) Mean (SD) | WBV group (n = 25) Mean (SD) | | Control group (n = 24) Mean (SD) | WBV group (n = 25) Mean (SD) |
| Primary outcomes |
| RM (points) | 12.44 (4.46) | 11.63 (8.35) | | 12.40 (4.50) | 10. 47 (8.68) | –1.12 (–2.42 to 0.96) | 0.001 | –1.01 |
| Oswestry (%) | 29.16 (15.78) | 26.50 (17.00) | | 29. 24 (15.64) | 20.28 (10.89) | –6.3 (–13.74 to –1.70) | 0.013 | –0.72 |
| HRQoL (tto) | 0.69 (0.03) | 0.71 (0.05) | | 0.68 (0.18) | 0.76 (0.23) | 0.06 (–0.10 to 0.09) | 0.042 | 0.53 |
| VAS back (0–100 points) | 39.54 (13.26) | 38.36 (15.85) | | 39.68 (14.77) | 29.00 (13.02) | –9.40 (2.94 to 16.05) | 0.006 | –0.85 |
| Secondary outcomes |
| PSTAntPost (º) | 0.57 (0.40) | 0.52 (0.22) | | 0.57 (0.40) | 0.41 (0.95) | –0.11 (–0.22 to 0.00) | 0.031 | –3.74 |
| PSTMedLat (º) | 0.47 (0.36) | 0.33 (0.17) | | 0.47 (0.37) | 0.30 (0.21) | –0.03 (–0.13 to –0.05) | 0.422 | –0.20 |
| T6MWT (m) | 419.52 (153.56) | 433.14 (87.39) | | 424.52 (144.56) | 458.62 (87.10) | 20.48 (12.61 to 53.57) | 0.221 | 0.34 |
| PILE test (kg) | 9.45 (9.41) | 12.25 (9.89) | | 9.50 (9.11) | 14.10 (9.55) | 1.80 (0.49 to 3.11) | 0.008 | 0.77 |
| Sens (vu) | 4.37 (3.52) | 5.68 (2.82) | | 4.50 (3.44) | 4.79 (2.51) | –1.02 (–1.71 to 0.42) | 0.002 | –2.20 |
| ap-values of analysis of variance (ANOVA) for repeated measures to compare differences between groups after 12-week vibration training. RM: Roland Morris questionnaire; Oswestry: Oswestry questionnaire; HRQoL: health-related quality of life measured with EQ-5D-3L questionnaire; VAS back: visual analogue scale for back pain (20 cm); PSTAntPost: anterior posterior score from postural stability test; PSTMedLat: medial lateral score from postural stability test; 6MWT: six-minute walk test; Sens: peripheral vibration sensibility; vu: vibration units about the vibration II manual; WBV group: whole body vibration group; tto: time trade-off tariff; PILE: Progressive Isoinertial Lifting Evaluation. |
DISCUSSION
To our knowledge, the present study is the first to have analysed the effects of WBV on specific LBP outcomes (Roland Morris and Oswestry questionnaire), vibratory threshold perception, HRQoL, and balance.
The main finding is that a 12-week course of low-frequency tilt WBV alleviated functional disability, decreased back pain and improved HRQoL in patients with NCLBP.
The Oswestry and RM questionnaires were used to measure the degree of NCLBP-associated disability, since these are the most widely used scales in assessing disability secondary to back pain (34). In the present study, the Oswestry indicated a 25% decrease in disability at 12 weeks in the WBV group. This change may be considered clinically relevant (31). A 1.12 point change in RM scores was observed in the WBV group, which may be considered to exceed the minimal threshold of clinically relevant change (35).
The improvements in the functional disability indices, balance, and vibration threshold sensibility were consistent with the observed decrease in pain. Previous studies have found correlations between pain and balance (36), pain and functional disability (37), and pain and vibration perception thresholds (38). On the basis of these data, it could be hypothesized that a reduction in pain may partly explain the increased level of functional capacity, balance, and sensitivity to vibration.
In accordance with the above data, the present study identified improvements in HRQoL in the WBV group (8.57%) compared with the control group. A change of 0.06 was observed in the WBV group, as measured with the EQ-5D-3L. This change did not exceed the minimal threshold of clinical change reported for this generic instrument (39). The EQ-5D-3L is widely used in the measurement of HRQoL and the analysis of the cost-effectiveness of targeted interventions in patients with LBP (32). However, some authors have reported that it underestimates HRQoL in LBP patients in the Spanish population, which has discouraged its use (40). Despite the acknowledged deficiencies of currently available tools, no specific instrument has yet been developed to assess HRQoL in patients with NCLBP in the Spanish population.
This study has several limitations. The small sample size may have limited the detection of other effects of WBV on some secondary outcomes. However, the study identified positive effects on the primary outcomes (functional disability). The study design precluded the detection of gender-effects, and further research is warranted to explore this issue. The study did not consider psychosocial factors, which are known to be important in determining the level of back pain (7). Finally, in this study there was no placebo group, thus the placebo effect was not controlled for, and this could affect some psychological parameters, such as VAS pain estimation and the motivation factor in the 6MWT and PILE test.
Future research
NCLBP has a high prevalence among the adult population and accounts for a substantial use of economic resources. Identifying effective therapies for NCLBP will therefore have a substantial impact on health and health economics. Further research is required to determine the effect of gender on the measures examined in the present study. Follow-up studies are also required to evaluate long-term outcomes. Finally, a cost-utility study is urgently needed to determine the suitability of the implementation of this type of therapy in routine clinical practice.
In conclusion, the hypotheses tested in the present study were verified. A 12-week course of low-frequency vibrating platform therapy was feasible and may represent a novel physical therapy for NCLBP. This therapy is applicable at low frequencies in individuals who are frail and previously physically untrained (15). The findings of the present study have implications for clinical practice, in terms of decreasing problems related to functional disability, and for public health policy, in terms of reducing healthcare costs.
ACKNOWLEDGEMENTS
The present study was supported by grants from the European Social Fund and the Junta of Extremadura Regional Call for Research (PRI07B093). The Red Cross, the Extremadura Department of Social Affairs and Dependence, and the Alejo Leal Clinic provided human and infrastructure resources. Miguel Hernandez Mocholí was awarded a pre-doctoral fellowship by the Spanish Ministry of Education (FPU3839).
The authors declare no conflicts of interest.
REFERENCES