OBJECTIVE: To establish the prevalence and patterns of self-reported musculoskeletal symptoms in community-dwelling stroke survivors and their impact on common activities of daily living.
METHODS: Analysis of data from two consecutive postal surveys in northern England. Data on overall joint pain, swelling or stiffness and difficulties with daily living tasks were obtained from 16,222 individuals aged ≥ 55 years (a response rate of 86%). Information on stroke-specific impairments was obtained from the 415 individuals who reported a stroke.
RESULTS: Forty-seven percent of stroke survivors reported musculoskeletal symptoms. There was a greater prevalence of reported symptoms in the smaller peripheral joints: 23.4% of stroke survivors reported symptoms in the ankle joint compared with 12.3% in the general population aged ≥ 55 years. Although both stroke-specific impairments and musculoskeletal pain contributed to difficulty in functional tasks, the effect of both was more than additive (for example, left hip symptoms increased the risk of having difficulty with standing and walking by 10.3 times (95% confidence interval 1.0, 106.3); stroke affecting the right leg increased the odds by 4.8 times (95% confidence interval 2.5, 9.2). Having both impairments increased the odds by 49.1 times (95% confidence interval 10.7, 225.4)).
CONCLUSION: Musculoskeletal symptoms are common in people with stroke and can have a significant additional effect on disability.
Key words: stroke; joint symptoms; epidemiology; functional impairment.
J Rehabil Med 2011; 43: 197–203
Correspondence address: Chamila Hettiarachchi, Specialist Registrar in Rheumatology & Rehabilitation Medicine, Academic Department of Rehabilitation Medicine, Section of Musculoskeletal Disease, Leeds Institute of Molecular Medicine, University of Leeds, Level D, Martin Wing, Leeds General Infirmary, Great George Street, Leeds, LS1 3EX, UK. E-mail: chamila@doctors.org.uk
Submitted May 1, 2010; accepted October 7, 2010
Introduction
Musculoskeletal complaints are common in the general population. Estimates suggest that 15% of the adult population have joint pain, with 2 out of 3 people over the age of 50 years reporting recent musculoskeletal pain (1). These problems can have a significant impact on physical independence (2). Similarly, stroke is one of the most common causes of severe physical disability (2, 3). Both conditions represent considerable direct and indirect costs to healthcare. In addition to physical disability, people with either condition are also more likely to have greater levels of anxiety, depression (4–6) and unemployment (7, 8). There is, however, little published information on the epidemiology and impact of musculoskeletal problems arising in people who have also had a stroke. Previous research in this area has focused largely on shoulder pain following stroke (9–13). The organization of clinical services is also aimed almost exclusively at the individual conditions. A single study examining the impact of osteoarthritis in rehabilitation of stroke patients found that people with both conditions have poorer outcomes (14). This suggests that musculoskeletal pain can have an adverse effect on recovery after stroke. The aim of this study was to investigate the prevalence and pattern of musculoskeletal problems in people with stroke and their impact on function through a community-based population survey.
Materials and methods
Sampling frame and size
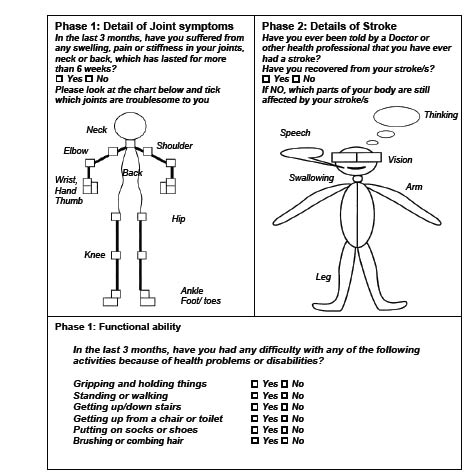
Data used in this study was collected from anonomized information obtained as part of a study of stroke prevalence in North Yorkshire, UK (15). This prevalence study involved a staged community-based postal survey. A series of questionnaires was sent to an age-stratified random sample of residents aged 55 years and over living within the North Yorkshire Health Authority catchment area. The survey consisted of 3 phases. In phase 1, a 4-page-screening questionnaire was used to identify a number of pathologies including community prevalence of stroke as well as the community prevalence of joint problems. The questionnaire asked, “Have you ever been told by a doctor or other health professional that you have had a stroke?” (Fig. 1). Other information collected included demographic data (age and gender), and physician-diagnosed co-morbidities. Data on musculoskeletal symptoms as well as difficulty with common activities of daily living were also collected. Patients were asked to indicate whether they had had any swelling, pain or stiffness in their joints, neck or back lasting more than 6 weeks in the previous 3 months. To identify the loci of joint symptoms, participants were asked to indicate the location of joint problems on a manikin, with major joints identified on the manikin as boxes. Participants were also asked to indicate if they experienced difficulties with activities of daily living, as described in Fig. 1.
Fig. 1. Questions and manikins included in the postal questionnaires.
In phase 2, those who reported that they had had a stroke were sent a further questionnaire designed to capture detailed information about the stroke as well as impact on function. This 12-page questionnaire included the question “Did these symptoms last for more than 24 hours?” aiming to distinguish “true” strokes from transient ischaemic attacks. Patients were also asked if they had completely recovered from a stroke. Participants were asked to indicate on a series of manikins (Fig. 1) the parts of the body that were affected by the stroke both at the time of the stroke and at the time of completing the questionnaire. Participants were encouraged to seek help in completing the questionnaire if necessary. Those who did so were asked to indicate the type of help needed (e.g. “writing”, “understanding the questions”). Phase 3, involved home visits by a research nurse, and consisted of a random sample of those identified from phase 2 as having had a stroke and was designed to validate the self-report diagnosis (15).
The data used in this study, which looks at the reporting of musculoskeletal disorders in people who had also had a stroke, has not been published previously.
Data analysis
In phase 1, following exploration for non-response bias, the data was adjusted for non-response by age and sex and for age, sex and dependency in phase 2. Weighted data was used to calculate prevalences and 95% confidence interval (CI) using methods described by Morris and Gardner (16). Unweighted data was used for all inferential statistics and modelling. Data was analysed using the Statistical Package for Social Sciences Version 14 (SPSS Chicago. IL, USA).
All patients with neurological symptoms lasting > 24 h (n = 415) have been included in the descriptive statistical analysis regardless of whether they reported recovery afterwards. For the purposes of calculating prevalence of self-reported symptoms in individual joints, joint symptoms in either the right, left or both joints were considered to be positive responses for that joint. The effect of central post-stroke pain on the self-reporting of joint symptoms was considered as a possible confounding factor. Post-stroke pain is reported in the area affected by stroke and often involves an entire limb or hemi-section of the body (17, 18). The published literature also suggests that 5–8% of all people with stroke will develop post-stroke pain, with approximately one-third experiencing a diminution of pain at 1 year post-stroke (17, 19–22). Based on clinical features of post-stroke pain, we created conservative surrogate markers for the likely presence of central post-stroke pain. A respondent was considered to be reporting post-stroke pain if all the loci on a particular limb within the manikin were “ticked”. We then examined the relationship between the presence of symptoms in all the loci on a particular limb and stroke affecting that limb. For example, those patients with stroke who did not report symptoms in all the joints areas of the paretic limb were designated as not having post-stroke pain.
The effect of self-reported musculoskeletal and neurological impairments on specific functional tasks was explored using logistic regression analysis. The neurological impairments used in the analysis were those that were experienced by the respondent at the time of completing the questionnaire. The likelihood of having difficulty with specific activities was expressed as odds ratios. Independent variables within the analysis included sex, age, time since stroke, all sites of joint symptoms and all stroke impairments. Aggregate variables were created to capture self-reported symptoms in the wrist and hand as well as the ankle and foot. In order to investigate the influence of laterality, combination variables were created to include stroke affecting either side of the body and symptoms affecting joints on the upper and lower limbs on either side of the body. Muti-collinearity of variables was assessed and variables with very low tolerance values were removed. All models were assessed for accuracy in classification and models that had an accuracy of more than 75% were retained. The Hosmer and Lemeshow Test of goodness of fit was calculated and all models that fulfilled the criteria were accepted. All models reported here have a predictive capacity (Nagelkerke R2) > 0.35. Summative odds ratios were calculated for combination of stroke and joint impairments based on that described in the literature (23, 24). The models used specific day-to-day activities as representative of arm and leg function (difficulty with gripping and holding, standing and walking, getting up and down stairs, getting up from a chair or toilet, putting on socks and shoes and brushing and combing hair).
Results
Response rate
Completed questionnaires were received from 16,222 individuals in phase 1 (86% response rate) and 745 individuals in phase 2 (76% response rate). A total of 330 respondents from phase 2 reported neurological symptoms lasting less than 24 h and were excluded from subsequent analysis. Thus, 415 (2.26% individuals from phase 1) reported having had a clinician-diagnosed stroke with symptoms lasting more than 24 hours (Table I).
| Table I. Basic characteristics in the study populations |
| | General population survey Phase 1: n = 16,222 n (%) | Stroke population survey Phase 2: n =415 n (%) |
| Age groups, years |
| 55–64 | 8,886 (54.8) | 120 (28.9) |
| 65–74 | 5,388 (33.2) | 169 (40.2) |
| ≥ 75 | 1,948 (12.0) | 128 (30.8) |
| Male | 7,151 (44.1) | 208 (50.1) |
| Physician-diagnosed co-morbidities |
| Hypertension | 4,214 (26.0) | 221 (53.3) |
| Diabetes | 728 (4.5) | 53 (12.8) |
| Arthritis | 6,457 (39.8) | 186 (44.4) |
| Stroke | 714a (4.4) | 415b (100) |
| Joint symptoms: pain, swelling or stiffness lasting > 6 weeks in the previous 3 months | 6,307 (38.9) | 196 (47.2) |
| aNumber represents all self-reported cerebrovascular events including stroke and transient ischaemic attacks. bNumber represents all self-reported strokes only. |
A total of 158 (38.1%) individuals were within 2 years post-stroke. A total of 99 (23.9%) individuals reported that they had recovered from the stroke impairments at the time of completing the questionnaire.
Prevalence of joint symptoms
The prevalence of stroke in the general population from this survey was 46.8 per 1000 (Table II) (15). The prevalence of joint problems in people with stroke was 22.0 per 1000. Thus 47% of individuals with stroke living in the community reported joint symptoms. Women with stroke had a higher prevalence of self-reported joint symptoms (55.5%) compared with men (40.8%), (c2 test: p < 0.001). The most common symptomatic joint reported by people with stroke was the knee (13.21 per 1000), followed by hand pain (11.73 per 1000) and the ankle (10.95 per 1000). For each joint, the prevalence of self-reported joint symptoms was highest in the group greater than 75 years of age.
| Table II. Prevalence estimates of joint pain, swelling, and/or stiffness over the last 3 months, lasting more than 6 weeks per 1000 patients with stroke |
| Joints/age, years | Rate per 1000 |
| Male | Female | Total |
| Neck total | 7.38 | 7.42 | 7.40 |
| 55–64 | 2.56 | 3.25 | 2.91 |
| 65–74 | 5.10 | 5.72 | 5.44 |
| ≥ 75 | 19.79 | 13.22 | 15.47 |
| Shoulder total | 8.92 | 10.83 | 10.00 |
| 55–64 | 4.14 | 3.00 | 3.56 |
| 65–74 | 6.15 | 7.83 | 7.07 |
| ≥ 75 | 22.01 | 21.53 | 21.70 |
| Back total | 6.87 | 8.49 | 7.78 |
| 55–64 | 2.24 | 3.00 | 2.63 |
| 65–74 | 5.13 | 6.92 | 6.11 |
| ≥ 75 | 18.05 | 15.48 | 16.36 |
| Elbow total | 3.56 | 7.65 | 5.87 |
| 55–64 | 2.22 | 2.01 | 2.11 |
| 65–74 | 3.07 | 5.60 | 4.45 |
| ≥ 75 | 6.76 | 15.25 | 12.34 |
| Hands total | 8.98 | 13.86 | 11.73 |
| 55–64 | 4.46 | 3.00 | 3.71 |
| 65–74 | 7.69 | 10.81 | 9.40 |
| ≥ 75 | 19.26 | 27.61 | 24.75 |
| Hip total | 6.07 | 9.59 | 8.06 |
| 55–64 | 3.51 | 3.25 | 3.38 |
| 65–74 | 7.16 | 6.92 | 7.03 |
| ≥ 75 | 9.03 | 18.52 | 15.27 |
| Knee total | 9.12 | 16.36 | 13.21 |
| 55–64 | 5.38 | 4.98 | 5.18 |
| 65–74 | 9.22 | 11.80 | 10.63 |
| ≥ 75 | 15.78 | 32.14 | 26.54 |
| Ankle total | 8.89 | 12.53 | 10.95 |
| 55–64 | 3.80 | 2.26 | 3.02 |
| 65–74 | 8.21 | 9.64 | 8.99 |
| ≥ 75 | 19.26 | 25.55 | 23.40 |
| Feet total | 9.45 | 10.35 | 9.96 |
| 55–64 | 3.22 | 3.00 | 3.11 |
| 65–74 | 8.70 | 9.31 | 9.03 |
| ≥ 75 | 22.01 | 18.64 | 19.80 |
| Total stroke population | 50.1 | 44.3 | 46.8 |
Patterns of reporting of joint symptoms
Joint symptoms across all joint categories were reported more frequently in those with stroke compared with those without stroke (Table III). A larger proportion of people with stroke reported symptoms in the smaller peripheral joints (wrists, elbows and ankles). Self-reported neck and back symptoms were not significantly increased in those with stroke.
| Table III. Comparison of the prevalence of self-reported joint symptoms in the different joints in the general population with the stroke population |
| | General population (%) (weighted sample size = 209,641) | Stroke population (%) (weighted sample size = 9814) | Ratio: Stroke population vs general population |
| Shoulders total | 16.2 | 21.4 | 1.3 |
| Elbows total | 6.9 | 12.5 | 1.8 |
| Wrists total | 9.2 | 17.4 | 1.9 |
| Hands total | 17.5 | 25.1 | 1.4 |
| Hips total | 12.6 | 17.2 | 1.4 |
| Knees total | 22.2 | 28.2 | 1.3 |
| Ankles total | 12.3 | 23.4 | 1.9 |
| Feet total | 13.6 | 21.3 | 1.6 |
| Upper and lower back | 16.4 | 16.6 | 1 |
| Neck | 15.3 | 15.8 | 1 |
Self-reported neurological impairments included: stroke affecting right arm (n = 102), stroke affecting left arm (n = 100), stroke affecting right leg (n = 110) and stroke affecting left leg (n = 121). Participants who reported upper limb stroke impairments were more likely to report joint symptoms in the joints on the side affected by stroke. Symptoms in the right shoulder (p = 0.023), right elbow (p < 0.001), right wrist (p < 0.001), right hand (p < 0.001), right thumb (p < 0.001), right ankle (p < 0.001), and right foot (p < 0.001) were more frequent in those with paresis of the right arm. Symptoms in the left shoulder (p = 0.004), left elbow (p = 0.018), left wrist (p = 0.047) left thumb (p = 0.027) and left hip (p = 0.027) was more frequent in those with left arm paresis. However, these associations were not identified in relation to laterality of leg paresis.
Just over half (55.4%) of those patients who were within 2 years of the stroke reported joint symptoms in comparison with just over two-fifths (43.5%) who were more than 2 years post-stroke at time of completing the questionnaire (c2 test: p < 0.05). However, there was little difference in the proportion of individuals with joint symptoms (46.1%) who reported that they had recovered from the stroke, compared with those with joint symptoms (48.1%) who did not report recovery from their stroke.
The influence of post-stroke pain on the pattern of self-reported joint symptoms was small. To examine the potential confounding effects of post-stroke pain, patients who reported symptoms in all the joint areas of a limb were considered to be reporting post-stroke pain. However, of those respondents who reported symptoms in all the joints of a limb, only a small percentage reported having stroke in that limb. For example, those reporting pain in all the right upper limb joint areas on the manikin, only 21 individual out of 271 reported stroke affecting that limb. The numbers were even lower in the other 3 limbs (6.8%, 7.1% and 5.8%, respectively, for the left arm, right and left leg). In addition, 90% of patients indicated that the onset of stroke was more than 1 year prior to completing the questionnaires, at which time one-third of people post-stroke might have expected to have a diminution in their pain (22).
Impact of self-reported joint symptoms on function
Participants reporting stroke and joint symptoms were significantly more likely to have difficulty across all 6 functional activities categories compared with individuals who had stroke alone: difficulty with gripping and holding (52.5% vs 18.1%, p < 0.001), standing and walking (68.9% vs 28.9%, p < 0.001), getting up and down stairs (55.2% vs 21.1%, p < 0.001), getting up from a chair or toilet (51.1% vs 17.5%, p < 0.001), putting on socks and shoes (50.4% vs 17.6%, p < 0.001) and brushing and combing hair (27% vs 17.24%, p < 0.001). These results are adjusted for age.
Logistic regression modelling was created for all 6 functional activities; 2 are shown in Table IV. These models were chosen as illustrative of upper and lower limb function respectively: gripping and holding; and standing and walking.
Participants who reported stroke affecting the left arm had increased odds of reporting difficulty with gripping and holding by 9.9 (p < 0.001, 95% CI 5.3–18.5). The presence of joint symptoms in the left wrist, hand or thumb increased the odds of reporting difficulty with this activity by 5.3 (p < 0.001, 95% CI 2.1–13.6). However, the combined effect of having both these neurological and musculoskeletal impairments considerably increased the odds of reporting difficulty with gripping and holding by 53 (95% CI 24.0–117.0).
Similarly, stroke affecting either leg increased the odds of reporting difficulty with standing and walking by more than 4 (for right leg, odds ratio (OR) 4.8, p < 0.001, 95% CI 2.5–9.2); joint symptoms affecting the left hip increased the odds by 10.3 (p = 0.05, 95% CI 1.0–106.3). Having both impairments considerably increased disability compared with having either impairment alone (e.g. stroke affecting the right leg and left hip joint symptoms increased the odds of reporting difficulty with standing and walking by 49.1 (95% CI 10.7–225.4)). Other combinations of stroke and joint impairments, which resulted in significantly raised odds of reporting difficulty with these activities, are illustrated in Table IV.
| Table IV. Logistic regression models to investigate the effect of stroke and/or joint symptoms on reporting difficulty with common activities of daily living |
| Activity/impairment | Odds ratio | 95% CI |
| Difficulty with gripping and holdinga | | |
| Stroke OR joint symptoms alone | | |
| Stroke left arm | 9.91 | 5.32–18.46 |
| Stroke right arm | 8.78 | 4.73–16.28 |
| Left wrist, hand or thumb joint symptoms | 5.34 | 2.10–13.56 |
| Right wrist, hand or thumb joint symptoms | 4.23 | 1.88–9.53 |
| Left shoulder joint symptoms | 2.90 | 0.93–9.00 |
| Right elbow joint symptoms | 2.40 | 0.58–10.03 |
| Stroke AND joint symptoms togetherb | | |
| Stroke left arm and left wrist, hand or thumb joint symptoms | 52.98 | 24.00–116.98 |
| Stroke right arm and left wrist, hand or thumb joint symptoms | 46.99 | 21.33–103.54 |
| Stroke right arm and left shoulder joint symptoms | 25.43 | 10.41–62.12 |
| Stroke left arm and right elbow symptoms | 23.83 | 8.37–67.83 |
| Difficulty with standing and walkingc | | |
| Stroke OR joint symptoms alone | | |
| Stroke left leg | 4.52 | 2.40–8.51 |
| Stroke right leg | 4.76 | 2.47–9.17 |
| Left hip joint symptoms | 10.31 | 1.00–106.29 |
| Left knee joint symptoms | 3.99 | 1.04–15.33 |
| Left ankle or foot joint symptoms | 4.61 | 1.25–17.00 |
| Stroke AND joint symptoms togetherb | | |
| Stroke right leg and left hip joint symptoms | 49.11 | 10.7–225.43 |
| Stroke left leg and left knee joint symptoms | 18.05 | 7.22–45.11 |
| Stroke left leg and left ankle or foot joint symptoms | 20.86 | 7.76–56.09 |
| aLogistic regression modelling for difficulty with gripping and holding things is shown (R2 = 0.425). bCombined odds ratios (ORs)are a summative calculation of the ORs for each impairment. cLogistic regression modelling for difficulty with standing and walking is shown (R2 = 0.373). CI: confidence interval. |
Table V shows the influence on function of having stroke-specific and joint-specific impairments on ipsilateral vs contralateral limbs. For activities involving the upper limbs, such as gripping and holding, the greatest risk of having functional difficulty occurred with stroke and joint impairments on contralateral limbs (e.g. stroke affecting the left side and joint pain in the right arm increased the odds of functional loss by almost 33 (OR 32.7, p = 0.001, 95% CI 4.4–241.7) compared with having both stroke and joint symptoms on the left side (OR 9.3, p < 0.001, 95% CI 3.2–26.5)). Similar findings were seen with the functional indicator “brushing and combing hair”, which also relies predominantly on upper limb function. However, for activities that predominantly involved lower limb function, such as standing and walking, the highest risk of reporting difficulty was with a combination of left-sided stroke and left-sided joint symptoms (stroke affecting left side and symptoms in any left leg joint, OR 22.6, p = 0.002, 95% CI 3.1–165.9). Similar findings were seen with other functional indicators, which relied mostly on lower limb function, such as difficulty with climbing stairs.
| Table V. Logistic regression investigating the impact of laterality: influence of having stroke and joint impairments on ipsilateral vs contralateral limbs on functiona |
| Activity/impairment | Odds ratio | 95% CI | p |
| a) Difficulty with gripping and holding | | | |
| Left-sided strokeb | 2.46 | 1.60–3.78 | p < 0.001 |
| Right-sided strokec | 3.26 | 2.07–5.12 | p < 0.001 |
| Left-sided stroke and any right arm joint symptoms | 32.69 | 4.42–241.67 | p = 0.001 |
| Left-sided stroke and any left arm joint symptoms | 9.27 | 3.22–26.50 | p < 0.001 |
| Right-sided stroke and any left arm joint symptoms | 12.24 | 2.85–52.40 | p = 0.001 |
| Right-sided stroke and any right arm joint symptoms | 8.10 | 3.12–21.02 | p < 0.001 |
| b) Difficulty with standing and walking | | | |
| Left-sided stroke | 3.38 | 1.20–5.71 | p < 0.001 |
| Right-sided stroke | 2.25 | 1.36–3.71 | p = 0.002 |
| Left-sided stroke and any left leg joint symptoms | 22.59 | 3.08–165.90 | p = 0.002 |
| Left-sided stroke and any right leg joint symptoms | 9.19 | 2.18–38.75 | p = 0.003 |
| Right-sided stroke and any left leg joint symptoms | 5.00 | 1.50–16.64 | p = 0.009 |
| Right-sided stroke and any right leg joint symptoms | 4.37 | 1.69–11.30 | p = 0.002 |
| aOdds ratios and 95% confidence intervals (CI) for the unadjusted main effects are shown. bCombination of stroke impairments affecting left arm and left leg. cCombination of stroke impairments affecting right arm and right leg. |
Discussion
We have reported the prevalence, patterns and functional impact of joint problems in stroke survivors living in the community. Forty-seven percent of individuals who reported a physician-diagnosed stroke also reported having joint pain, stiffness or swelling lasting more than 6 weeks over the previous 3-month period. This is substantially higher than the reported prevalence of joint symptoms in all community-dwellers over the age of 55 years, which was 39.11% (25). Self-reported joint symptoms were higher in women with stroke compared with men. This is consistent with gender differences in self-reported joint pain in the general population over 55 years of age.
The prevalence of symptoms in all joints was higher in the stroke population compared with individuals in the general population over the age of 55 years. However, this difference was greatest in the smaller peripheral joints, particularly the elbows, wrists, ankles and feet. These findings contrast with previously published studies, which have shown increased reporting of shoulder pain alone in people with stroke (9–13, 26). Most of these studies, however, have focused on complications following stroke in the acute setting or in the first year after stroke. This is the first study to examine the epidemiology and functional impact of joint symptoms in community-dwellers who have previously had a stroke. The reason for the increased reporting of joint symptoms in the smaller joints may relate to a number of factors. Increase in self-reported smaller upper limb joint pain, could be due the additional stresses put on these joints due to the prolonged use of walking aids or the consequence of using the arms during transfers. In the legs, change in gait pattern after stroke may lead to an increase in foot and ankle symptoms due to difficulty in normal foot placement. However, self-reported rates of back symptoms were almost identical in the 2 populations.
Participants with stroke impairments affecting one side of the body were more likely to report joint symptoms affecting the affected side. Due to the self-reported nature of the survey, it is difficult to ascertain whether symptoms were due to true joint pathology or a consequence of neurological impairments such as spasticity or post-stroke pain. The present study addressed the confounding affects of post-stroke pain by using the pattern of self-reported joint symptoms. Our analysis of the data indicates that the influence of central post-stroke pain in erroneous self-reporting of joint symptoms is small (i.e. self-reported joint symptoms in people with stroke is likely to be related to joint pathology rather than presence of post-stroke pain affecting the limb). However, we may have underestimated the true impact of joint symptoms on disability in people with stroke by assuming that when the participant reported pain in all joints on the side of the body affected by stroke this was due to post-stroke pain. This study was not designed to capture self-reported post-stroke pain, which is a limitation of the data-set.
Not surprisingly, individuals with stroke and joint symptoms were more likely to have difficulty with functional tasks compared with participants with stroke alone. However, the increase in difficulty was greater than merely the additive effects of having both impairments (Table IV). There is therefore a substantial penalty in terms of loss of function when stroke survivors also have joint symptoms. These findings concur with published data (14) reporting poorer early rehabilitation outcomes after acute stroke in those who also had osteoarthritis.
The presence of musculoskeletal symptoms and stroke impairments on ipsilateral vs contralateral limbs appears to have different effects on function depending on whether the upper limbs or the lower limbs are affected. In the case of the upper limbs, stroke and joint impairments on contralateral sides will be more likely to reduce function. In the legs, ipsilateral involvement of stroke and joint pain (e.g. stroke leg impairment and joint pain are present in the same leg) results in greater functional loss. It is likely that joint problems in the stroke-affected leg can make load-bearing much more difficult due to presence of weakness and pain. If inability to take load through the stroke-affected limb is compromised, then transferring, sit to stand and walking activities would be more difficult compared with contralateral leg joint pain and stroke symptoms.
Our exploration of the associations in the data was limited by the constraints of the data collected through an existing community survey. The data used in the analysis were self-reported and therefore will be subject to self-report bias. However, the reliability of ascertainment of stroke for the survey method used in this study was good (15). Further research is needed to clarify the influence of laterality of stroke and joint impairments on function, as our analysis is performed on data from a study not originally designed to capture these associations. Other potentially interesting associations, for example, between handedness and functional limitations in the context of joint pain and laterality of stroke, need to be explored. In addition, the presence of neurological conditions may cause a differential phenotype in the presence of musculoskeletal conditions that generally cause symmetrical joint symptoms. For example, osteoarthritis affecting the joints of the hand may be less prominent in the hand affected by stroke (27). A prospective study to investigate these factors is ongoing.
Both stroke and musculoskeletal problems are far more common in older age groups (1, 3). With changing population demographics, the prevalence of individuals with both conditions is set to rise. Our study suggests that these individuals are at risk of substantial loss of function and independence. Consequently there is likely to be an increased burden on health resources and the social services. Clinical services and guidelines on stroke are limited in their coverage of joint symptoms following stroke, with existing care pathways focusing almost exclusively on shoulder pain following stroke (28). Our study shows that almost half of all stroke survivors will have joint pain, and this is more likely to affect the smaller peripheral joints. In view of these findings, changes need to be made to the understanding of joint symptoms after stroke and the planning of long-term care for stroke survivors. The mechanisms of joint symptoms following stroke needs further research in order to explore possible preventive and treatment strategies. This information also has important implications for clinical trials on stroke treatments. Given that concurrent musculoskeletal problems in people with stroke can have such a significant effect on physical functioning, it is vital that musculoskeletal impairments are captured in people with stroke who are recruited into randomized clinical trials that use functional outcomes as primary end-points, as an imbalance of musculoskeletal problems across the intervention groups may confound the interpretation of functional outcomes.
References