OBJECTIVE: The aim of this study was to demonstrate the use of the International Classification of Functioning, Disability and Health (ICF) to measure the effect of physiotherapy treatment.
DESIGN: A prospective cohort study with an additional case report.
Patients: Individuals were eligible for the study if they were patients at the University Hospital of Zurich and had received physiotherapeutic interventions during their inpatient stay.
METHODS: Patient’s functioning was assessed by physiotherapists at initiation of physiotherapeutic treatment and at discharge using ICF Core Sets.
RESULTS: A total of 425 patients were analysed, mean age 60 years, 42% female. The median of treatment days varied between 4 (intensive care unit) and 19 (low back pain). The majority of patients had improved or stable results; improvement was most prominent in the surgical and internal medicine group. The ICF category d450 “Walking” appears in 4 out of 6 ICF Core Sets, being only infrequently treated in intensive care unit and low back pain.
CONCLUSION: Analysis showed that the ICF can be used to record precise information on patients’ functioning in the acute hospital. Typical impairments and restrictions, intervention goals and trajectories of functioning could be documented.
The qualifiers used in our clinical example were sensitive to change. Definitions of qualifiers, however, should be the subject of further research.
Key words: ICF; physiotherapy; physical therapy; goals; outcome assessment; classification.
J Rehabil Medicine 2011; 43: 174–177
Correspondence address: Eva Grill, Institute for Health and Rehabilitation Sciences, Ludwig-Maximilians-Universität München, 81377 Munich, Germany. E-Mail eva.grill@med.uni-muenchen.de
Submitted May 25, 2010; accepted September 7, 2010
INTRODUCTION
Physiotherapeutic interventions are an important part of coordinated treatment in the acute hospital. The aim of these interventions is to prevent impairments, medical complications and risks, and to restore selected aspects of functioning. Specific goals of physical therapy depend on diagnosis and functional status, but also on the patient‘s age, life situation and person factors. Early planning and onset of physiotherapy improves functioning and ultimately contributes to the prevention of impairment and disability (1–4).
Physiotherapeutic interventions are part of a continuous process of defining and addressing patients’ needs and goals. The success of any intervention should be evaluated to be able to adapt goals and interventions if necessary (5). Thus, physiotherapeutic interventions might be described by their respective goals.
Despite this importance for patient outcome, until now there has been no standardized tool that describes both the goals of physiotherapeutic interventions and measures the effect of these interventions. An instrument is needed that is easy to use in the hands of the prospective user, which is not time-consuming, and which focuses on the specific needs of the patients in the acute hospital.
The International Classification of Functioning, Disability and Health (ICF) is an interesting option for describing single components of functioning and specific goals of physiotherapy. Introduced by the World Health Organization (WHO) to classify and structure human functioning in all its facets, it is specifically intended for the documentation of health status to be used by all groups of health professionals (6). It has been shown to be relatively simple to use, valid and reliable in the hands of physical therapists in the acute hospital (7, 8), applicable regardless of the underlying health condition or clinical situation, comprehensive across elements of functioning, and there are short versions useful for specific health conditions or settings, such as the acute hospital (9).
ICF categories can have multiple purposes, namely for assessment and categorization of functional impairment and activity restriction from the patient perspective. In particular, they can be used to standardize goals of physiotherapeutic interventions (10). It has to be emphasized that the assessment of functioning should always be a team effort, with each profession contributing. ICF-based items can therefore be the basis of a common language in the acute hospital setting. Selections of the ICF, called ICF Core Sets for the acute hospital were developed and validated for clinical practice. Yet, experience with the practical application of the ICF Core Sets is scarce. The physiotherapy department of the Institute of Physical Medicine of the University Hospital in Zurich has been part of the ICF research since its beginning and has been using the ICF Core Sets for patient assessment. Thus, motivation was high to provide the first examples of the application of the ICF in physiotherapy in the acute hospital.
The aim of this study was to demonstrate the use of the ICF to describe therapy goals and to assess the potential effect of rehabilitation interventions, first by implementing operationalized ICF qualifiers and, secondly, through a case report.
METHODS
Patients and data collection
Individuals were eligible for the study if they were patients at the University Hospital of Zurich from April to September 2008 and had received physiotherapeutic interventions during their inpatient stay. Patients were characterized primarily by their respective health condition requiring medical treatment, i.e. patients in surgical (SUR) and internal medicine wards (INT), patients in the intensive care unit (ICU), patients with neurological conditions (NEU) or after neurosurgery (NES), and patients with low back pain (LBP). This allocation was chosen according to the organizational structure of the physiotherapeutic services of the hospital. To find a balance between practicability and representativeness, we recruited up to 100 patients by health condition group, allowing a maximum of 6 months for recruitment.
Measures
The ICF is a model and multipurpose classification that belongs to the WHO family of international classifications. In a preceding Delphi study ICF categories representing goals of physiotherapeutic interventions typical for the acute hospital had been defined (11). Along this choice of categories, typical second-level ICF categories were chosen. A problem was defined as typical if 10% or more of the patients were treated for it. This led to 6 ICF Core Sets in accordance with the organizational structure of the physiotherapeutic services, an ICF Core Set for SUR, INT, ICU, NEU, NES and LBP. The 6 ICF Core Sets consisted of 42–121 categories per set (SUR = 45, INT = 56, ICU = 42, NEU = 121, NES = 87, LBP = 48).
Physiotherapists with expertise in assessment and the ICF decided on the appropriate operationalization of the ICF categories. Detailed description of the process and operationalization of the items is given in Grill et al. (12).
Data collection
Each patient’s impairment in Body Functions and Structures or restriction in Activities and Participation was assessed by physical therapists according to 1 of the 6 ICF Core Sets. The assessment took place at initiation of physiotherapeutic treatment and at the end. In addition, the physical therapists recorded whether the respective problem was the goal of a PT intervention. Since we report routine data serving as a hospital specific quality improvement system, informed consent and approval of the ethics committee was not obtained. The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statistical analyses
We reported means and standard deviations or the respective median and quantiles for continuous variables and percentages for ordinal or nominal variables. For the reporting of treatment outcomes we excluded patients with missing values at the end of treatment.
RESULTS
Implementation of ICF Core Sets for quantitative physiotherapeutic reporting
A total of 549 patients were recruited initially. For the analyses 124 patients were excluded due to missing data at the end of the treatment (SUR 6 patients, INT 20 patients, ICU 59 patients, NEU 24 patients, NES 13 patients and LBP 2 patients). Mean age was 60 years, 42% were female. Detailed demographic information is shown in Table I. Median of treatment days varied between 4 (ICU) and 19 (LBP). All patients presented with more problems present than were treated.
| Table I. Demographic characteristics of included patients, stratified for International Classification of Functioning, Disability and Health (ICF) Core Set surgery (SUR), internal medicine (INT), intensive care unit (ICU), neurology (NEU), neuro-surgery (NES) and low back pain (LBP) |
| | ALL | SUR | INT | ICU | NEU | NES | LBP |
| Patients, n | 425 | 94 | 80 | 41 | 73 | 81 | 56 |
| Female, % | 41.9 | 39.4 | 38.8 | 36.6 | 37 | 48.2 | 51.8 |
| Mean age (SD) | 59.9 (16.9) | 57.8 (19.4) | 59.0 (16.5) | 62.0 (14.7) | 60.2 (18.0) | 61.2 (14.6) | 61.1 (16.7) |
| Days with therapy, median (1st quartile; 3rd quartile) | 8 (4;15) | 7 (4;11) | 8 (4;20.5) | 4 (3;7) | 8 (5;11) | 8 (4;14) | 19 (11;26) |
| Mean number of problems present, n | 13.0 | 9.2 | 12.8 | 10.8 | 16.1 | 17.9 | 10.2 |
| Mean number of problems treated, n | 9.7 | 7.6 | 9 | 8.8 | 9.6 | 15.2 | 7.1 |
| SD: standard deviation. |
The most frequent diagnoses were bypass, valvular transplant and traumatic brain injury for SUR; conditions affecting the lungs (e.g. pneumonia, asthma, chronic obstructive pulmonary disease) and neoplasms (e.g. leukaemia, lymphoma, tumours of the internal organs) for INT; stroke and multiple sclerosis for NEU; brain disease (e.g. subarachnoidal bleeding, tumours) with or without neurological deficits for NES and chronic low back pain for LBP. The ICU included patients from all clinical departments, regardless of the underlying diagnosis. The 3 categories most frequently treated per ICF Core Set are shown in Table II. The ICF category Walking (d450) appears in 4 out of 6 ICF Core Sets, being only infrequently treated in ICU and LBP.
| Table II. Most frequently treated International Classification of Functioning, Disability and Health (ICF) categories, stratified for ICF Core Set surgery (SUR), internal medicine (INT), intensive care unit (ICU), neurology (NEU), neuro-surgery (NES) and low back pain (LBP), and the percentage of patients improved, stable or deteriorated in the respective category |
| Core Set | ICF Category | Definition | Improved % | Stable % | Deteriorated % |
| SUR (n = 94) | d450 | Walking | 85.7 | 14.3 | 0.0 |
| | b4550 | General physical endurance | 89.4 | 10.6 | 0.0 |
| | d4551 | Climbing | 73.0 | 27.0 | 0.0 |
| INT (n = 80) | d450 | Walking | 65.7 | 28.4 | 6.0 |
| | b4550 | General physical endurance | 60.6 | 31.0 | 8.5 |
| | d4551 | Climbing | 63.2 | 32.4 | 4.4 |
| ICU (n = 41) | b440 | Respiration functions | 56.4 | 38.5 | 5.1 |
| | b4402 | Depth of respiration | 10.3 | 89.7 | 0.0 |
| | d410 | Changing basic body position | 55.0 | 45.0 | 0.0 |
| NEU (n = 73) | b755 | Involuntary movement reaction functions | 15.9 | 84.1 | 0.0 |
| | b760 | Control of voluntary movement functions | 8.6 | 91.4 | 0.0 |
| | d450 | Walking | 62.1 | 37.9 | 0.0 |
| NES (n = 81) | b735 | Muscle tone functions (hypotone) | 8.2 | 91.8 | 0.0 |
| | b760 | Control of voluntary movement functions | 9.1 | 90.9 | 0.0 |
| | d450 | Walking | 23.9 | 65.8 | 1.4 |
| LBP (n = 56) | b280 | Sensation of pain | 79.3 | 20.8 | 0.0 |
| | b4550 | General physical endurance | 71.2 | 28.9 | 0.0 |
| | b710 | Mobility of joint functions | 39.6 | 60.4 | 0.0 |
Outcomes of the 3 categories most frequently treated per ICF Core Set are shown in Table II. The majority of patients had improved or stable results; improvement was most prominent in the surgical and internal medicine group.
Application of ICF Core Sets to a case report
In the following case report we describe the therapy process of a 39-year-old male patient with a cerebrovascular insult after a carotid artery dissection on the left side. The current medical treatment was intravenous thrombolysis. The consequences of the diagnosis presented a hemiparesis of the right side and regredient aphasia. His ability to speak was regressive (d330). He could not remain in a sitting position (d4153) or a standing position (d4154) and was unable to walk (d450). Paresis of his right hand resulted in restricted hand and arm use (d445), making it impossible to lift and carry objects (d430) and restricted his fine hand use (d440). Carrying out daily routine was restricted (d230). The patient had the full support of his immediate family (e310) acting as a facilitator for therapy. Extensor muscles of his fingers were hypotonic (b7300). Single muscle contractions of the hand could be evoked; they were, however, insufficient for hand use because of impaired muscle endurance (b740). Coordination (b760), proprioception (b260) and sensibility (b265) were impaired and thus affected coordination of movement. Lower extremity muscle function (b7301) was weakened; proprioception (b1801, b260) and sensibility were reduced accordingly. Balance was impaired (b755). Aphasia presented itself by impaired fluency and rhythm of speech (b330).
The therapy goals were upper and lower extremity functions and activities to enable autonomy and return to work (d440, d445, d450). Physiotherapeutic interventions comprised several units with the goal to remain in standing position (d4154) and to carry out daily routine (d230). Specific exercises aimed at muscle power of isolated muscles or muscle groups (b7300), muscle power of an extremity (b7301), reduced muscle tone (b735), control of voluntary movements (b760), proprioception (b260), touch function (b265), body experience (b1801), and involuntary movement functions (b755).
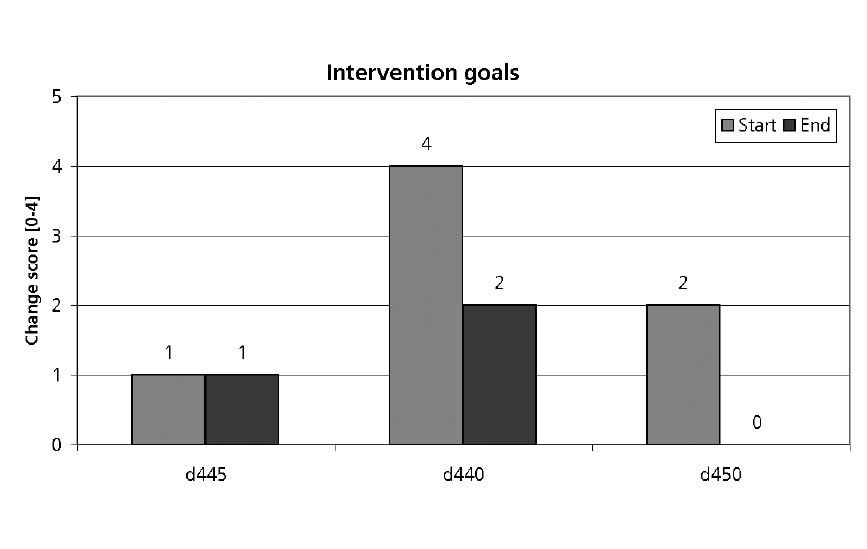
Fig. 1 shows evaluation of intervention goals Fine hand use (d440), Hand and arm use (d445) and Walking (d450) at admission and discharge. Qualifier 4 stands for complete restriction, 0 stands for no or minimal restriction.
Fig. 1. Change of functioning from beginning of physical therapy to the end for 3 International Classification of Functioning, Disability and Health (ICF) categories, Hand and arm use (d445), Fine hand use (d440) and Walking (d450) for a patient with cerebrovascular insult. Lower scores indicate less restriction.
Although there was improvement in the patient’s hand and arm use, the qualifier scale was not sensitive enough to assess the changes experienced. Improvements in Fine hand use (d440) and Walking (d450), however, were shown.
DISCUSSION
We demonstrated that physiotherapists in the acute hospital can code functioning, treatment goals and treatment results with the help of the ICF. Physiotherapeutic documentation in the acute hospital is very challenging because it has to include the entire process of diagnosis, goal-setting, intervention and outcomes. Additionally, documentation has to be meaningful for other health professionals involved in patient management.
There are few examples and proposals for standardized documentation of physiotherapeutic interventions and their outcomes in the acute hospital. Few recent studies explored the possibilities to use the ICF as a multidisciplinary language in the acute hospital e.g. to compare patients’ functioning profiles (13) or to classify facilitators and barriers to effective communication with the patient (14). We could show that categories of the ICF can be useful in the hands of physiotherapists in several ways. Firstly, they can serve as an assessment of the patient’s actual problems. Secondly, once assessed, those categories can help to define therapy goals. Thirdly, refining qualifiers and delving into lower levels of the classification may help to specify interventions. Fourthly, once specified, therapy goals can serve as outcome measures for the degree of goal attainment and the success of therapy.
There is, to date, no assessment system tailored to the needs of the physiotherapists that would fulfill all 4 purposes. In neurological conditions for example, the Barthel Index (BI) is a commonly used assessment instruments in neurological rehabilitation to measure the independence of a patient (15).
The BI is also used for the assessment of change. While the BI and various other similar measures are established in post-acute neurological rehabilitation, it is not clear if they can capture the specific short-term effects of physiotherapeutic interventions. Likewise, their underlying concepts may not be broad enough to specify therapy goals or interventions.
However, applying the ICF in physical therapy in the proposed way may have several limitations. Early feedback from health professionals suggested that the definition of ICF Core Sets was a step in the right direction towards establishing evidence-based measurement in the acute hospital. Due to the consensus process, the ICF Core Sets in their present version are comprehensive, with applicability for the assessment of individual problems and needs, and for the estimation of prognosis and the potential for rehabilitation potential, and with general applicability for assessment of functioning in the acute situation. As such, the ICF Core Sets can be used to coordinate physiotherapeutic interventions, e.g. at the intensive care unit. However, a minimally sufficient data-set, which is feasible in clinical practice, may encompass only 20 different concepts or topics, but not much more as contained in the comprehensive ICF Core Sets. Thus, subsets can be extracted from the comprehensive Core Sets, according to specific needs of the individual user. There is work in progress to define those smaller sets, also for physiotherapists. On the other hand, patients’ health condition in acute care is often unstable. Therapy goals and interventions may vary from day to day, impeding meaningful documentation. Also, we found that, in some of the functioning aspects, the qualifier scale proposed by the ICF and operationalized by consensus is not sensitive enough to code small effects of therapy. The qualifiers still need to be refined and validated.
Quantitative analysis of a small sample of patients and a case report showed that the ICF can be used to record precise information on patients’ functioning in the acute hospital. Typical impairments and restrictions, intervention goals and trajectories of functioning can be documented. The qualifiers used in our clinical example were sensitive to change. Definitions of qualifiers, however, should be the subject of further research.
ACKNOWLEDGEMENTS
The authors wish to thank the physiotherapists of all wards involved at the University Hospital Zurich for data collection.
REFERENCES